Westchester County Community Health Assessment 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2017 Match Day Results by Program
Class of 2017 Match Results Anesthesiology New York Presbyterian Hospital-Columbia University Medical Center University of Illinois College of Medicine-Chicago University of Texas Medical School-Houston Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Florida College of Medicine-Shands Hospital New York Presbyterian Hospital-Weill Cornell Medical Center Einstein/Montefiore Medical Center (New York) New York Presbyterian Hospital-Columbia University Medical Center Dermatology University at Buffalo School of Medicine (New York) University of Buffalo School of Medicine (New York) Cleveland Clinic Foundation (OH) Emergency Medicine Einstein/Montefiore Medical Center (New York) University of Massachusetts Medical School Staten Island University Hospital (New York) Stanford University Programs (California) Stony Brook Teaching Hospitals (New York) New York Hospital Medical Center Queens (New York) Eastern Virginia Medical School University of Washington Affiliated Hospitals Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Connecticut School of Medicine Rhode Island Hospital/Brown University Wake Forest Baptist Medical Center (North Carolina) Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) Einstein/Montefiore Medical Center (New York) Oregon Health and Science University Dartmouth-Hitchcock Medical Center (New Hampshire) Einstein/Montefiore Medical Center (New York) University of Washington Affiliated Hospitals Einstein/Montefiore Medical Center -

Hospitals Locations at a Glance
Hospitals Locations at a glance Nassau County Syosset Hospital Zucker Hillside Hospital Glen Cove Hospital 221 Jericho Turnpike 75-59 263rd Street 101 St. Andrews Lane Syosset, NY 11791 Glen Oaks, NY 11004 Glen Cove, NY 11542 (516) 496-6400 (718) 470-8100 (516) 674-7300 Suffolk County Manhattan Long Island Jewish (LIJ) Huntington Hospital Lenox Hill Hospital Valley Stream 270 Park Avenue 100 East 77th Street 900 Franklin Avenue Huntington, NY 11743 New York, NY 10075 Valley Stream, NY 11580 (631) 351-2000 (212) 434-2000 (516) 256-6000 Mather Hospital Manhattan Eye, Ear North Shore University Hospital 75 North Country Road & Throat Hospital 300 Community Drive Port Jefferson, NY 11777 210 East 64th Street Manhasset, NY 11030 (631) 473-1320 New York, NY 10065 (516) 562-0100 (212) 838-9200 Peconic Bay Medical Center Long Island Jewish 1300 Roanoke Avenue Bronx Medical Center Riverhead, NY 11901 St. Barnabas Hospital 270-05 76th Avenue (631) 548-6000 4487 Third Avenue New Hyde Park , NY 11040 Bronx, NY 10457 (718) 470-7000 South Oaks Hospital (718) 960-9000 400 Sunrise Highway Plainview Hospital Amityville, NY 11701 Kings 888 Old Country Road (631) 264-4000 Maimonides Medical Center Plainview, NY 11803 4802 Tenth Avenue (516) 719-3000 Southside Hospital Brooklyn, NY 11219 301 East Main Street (718) 285-3300 Steven & Alexandra Cohen Bay Shore, NY11706 Children’s Medical Center of (631) 968-3000 Wyckoff Heights Medical Center New York 374 Stockholm Street 269-01 76th Avenue Queens Brooklyn, NY 11237 New Hyde Park , NY 11040 Long Island Jewish -

Sharps Smart Brochure
George Latimer, Westchester County Executive www.westchestergov.com/recycle Department of Health (914) 813-5000 Department of Environmental Facilities Never put Sharps Containers in a Recycling Bin! Sharps Disposal Site List Municipality Facility Name Address Telephone Location Times Accepted Briarcliff Manor Brandywine Nursing Home 620 Sleepy Hollow Road, Briarcliff Manor, NY 10510 914 941-5100 Reception Area Wed. 2-3 Bronxville Lawrence Hospital Center 55 Palmer Avenue, Bronxville, NY 10708 914 787-3056 Receiving Loading Dock M-F 1-3 Cortlandt Cortlandt Healthcare, LLC 110 Oregon Road, Cortlandt Manor, NY 10567 914 739-9150 x226 Main Lobby M-F 9-12 and 1-3 Cortlandt Manor Field Home/Holy Comforter 2300 Catherine Street, Cortlandt Manor, NY 10567 914 739-2244 Front Desk M-F 8-2 Cortlandt Manor Hudson Valley Hospital Center 1980 Crompond Road, Cortlandt Manor, NY 10567 914 737-9000 Front Desk M-F 8-4 Croton-on-Hudson Skyview Health Care Center 280 Albany Post Road, Croton On Hudson, NY 10520 914 271-5151 Main Entrance 9-12, 1st Mon. of the month only Dobbs Ferry St. Cabrini Nursing Home, Inc. 115 Broadway, Dobbs Ferry, NY 10522 914 693-6800 Nursing Office Wed. 1:30-4:30 Harrison St. Vincent's Medical Center 275 North Street, Harrison, NY 10523 914 925-5359 Main Lobby Security 12-2, 1st Thu. of the month only Hastings-on-Hudson Andrus on Hudson 185 Old Broadway, Hastings-on-Hudson, NY 10706 914 478-3700 Main Entrance Wed. 7-12 Hawthorne Rosary Hill Home 600 Linda Avenue, Hawthorne, NY 10532 914 769-0114 Receptionist in Admissions Office Tue. -
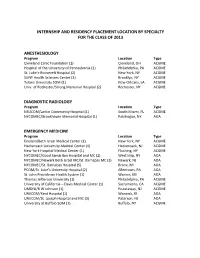
Internship and Residency Placement Location by Specialty for the Class of 2013
INTERNSHIP AND RESIDENCY PLACEMENT LOCATION BY SPECIALTY FOR THE CLASS OF 2013 ANESTHESIOLOGY Program Location Type Cleveland Clinic Foundation (2) Cleveland, OH ACGME Hospital of the University of Pennsylvania (1) Philadelphia, PA ACGME St. Luke’s-Roosevelt Hospital (2) New York, NY ACGME SUNY Health Sciences Center (2) Brooklyn, NY ACGME Tulane University SOM (1) New Orleans, LA ACGME Univ. of Rochester/Strong Memorial Hospital (2) Rochester, NY ACGME DIAGNOSTIC RADIOLOGY Program Location Type NSUCOM/Larkin Community Hospital (1) South Miami, FL ACGME NYCOMEC/Brookhaven Memorial Hospital (1) Patchogue, NY AOA EMERGENCY MEDICINE Program Location Type Einstein/Beth Israel Medical Center (2) New York, NY ACGME Hackensack University Medical Center (1) Hackensack, NJ ACGME New York Hospital Medical Center (1) Flushing, NY ACGME NYCOMEC/Good Samaritan Hospital and MC (2) West Islip, NY AOA NYCOMEC/Newark Beth Israel MC/St. Barnabas MC (3) Newark, NJ AOA NYCOMEC/St. Barnabas Hospital (5) Bronx, NY AOA PCOM/St. Luke’s University Hospital (2) Allentown, PA AOA St. John Providence Health System (1) Warren, MI AOA Thomas Jefferson University (1) Philadelphia, PA ACGME University of California – Davis Medical Center (1) Sacramento, CA ACGME UMDNJ/R W Johnson (1) Piscataway, NJ ACGME UNECOM/Kent Hospital (1) Warwick, RI AOA UNECOM/St. Joseph Hospital and MC (3) Paterson, NJ AOA University at Buffalo SOM (1) Buffalo, NY ACGME FAMILY MEDICINE Program Location Type Clarion Hospital (1) Clarion, PA AOA Einstein/Beth Israel Medical Center (1) New York, NY ACGME Eisenhower Army Medical Center (1) Fort Gordon, GA Military Ellis Hospital (2) Schenectady, NY ACGME Emory University SOM (1) Atlanta, GA ACGME Institute for Family Health/Harlem-Mt. -

We Are Northwell Health
Post-Acute Services Skilled Nursing/Senior Living Facilities Northwell Health GoHealth - Home Care Network - Broadlawn Manor Nursing and Urgent Care Centers We are 61,000 people looking at healthcare differently. - RegionCare Inc. Rehabilitation Center - Amityville - Hospice Care Network - Orzac Center for Rehabilitation - Astoria We are many things, but every day we are one thing: - Stern Family Center for Rehabilitation - Bay Shore Rehabilitation Network - Peconic Bay Skilled Nursing - Bellmore Acute Inpatient Rehabilitation dedicated to the community. and Rehabilitation Center - Commack - Glen Cove Hospital - 34 nursing home/senior living affiliates - Chelsea - Phelps Memorial Hospital Center - Dongan Hills - Staten Island University Hospital, North Special Needs Programs - East 81st - Southside Hospital - Adults and Children with Learning and - East Northport Developmental Disabilities, Inc. (ACLD) Subacute Rehabilitation - Elwood (affiliate) - Broadlawn Manor Nursing and - Forest Hills We are Northwell Health... - Association for the Help of Retarded Rehabilitation Center - Gramercy Children (AHRC)—Nassau (affiliate) - Orzac Center for Rehabilitation - Great Kills - Brookville Center for Children’s Services - Peconic Bay Skilled Nursing and - Greenwich Village (affiliate) Rehabilitation Center - Hampton Bays - Barbara C. Wilson Preschool Program - Stern Family Center for Rehabilitation - Huntington Station - Children’s Education Center - New York’s largest - LeFrak City Outpatient Rehabilitation • Leeds Child Development Center - -

Carrier Hospital Guide
2021 Carrier Hospital Guide EmblemHealth EmblemHealth EmblemHealth Oscar Oxford Oxford Hospital Name Healthfirst County Prime Select Care Millenium Circle Metro Liberty Albert Einstein College of Medicine √ √ √ √ √ Bronx BronxCare Health System √ √ √ √ Bronx Calvary Hospital √ √ √ √ Bronx Jacobi Medical Center √ √ √ √ √ Bronx Lincoln Medical & Mental Health Center √ √ √ √ √ Bronx Montefiore Medical Center √ √ √ √ Bronx Montefiore Westchester Square √ √ Bronx North Central Bronx Hospital √ √ √ √ √ Bronx St. Barnabas Hospital √ √ √ √ √ √ Bronx Total Hospitals in Bronx County 9 4 4 7 2 7 7 Midhudson Regional Hospital √ √ √ Dutchess Northern Dutchess Hospital √ √ √ √ Dutchess Vassar Brothers Medical Center √ √ √ √ Dutchess Total Hospitals in Dutchess County 3 2 0 0 0 3 3 Brookdale University Hospital Medical Center √ √ √ √ √ Kings Brooklyn Hospital Center √ √ √ √ √ √ √ Kings Coney Island Hospital Center √ √ √ √ √ Kings Interfaith Medical Center √ √ √ √ √ Kings Kings County Hospital Center √ √ √ √ √ Kings Kingsbrook Jewish Medical Center √ √ √ √ √ Kings Maimonides Medical Center √ √ √ Kings Mount Sinai Brooklyn √ √ √ √ √ √ √ Kings NYC Health + Hospitals √ √ √ √ √ Kings New York Community Hospital of Brooklyn √ √ √ √ Kings New York Presbyterian Methodist √ √ √ √ √ Kings NYU Lutheran Medical Center √ √ √ √ Kings SUNY Downstate Medical Center √ √ √ √ Kings Woodhull Medical and Mental Health Center √ √ √ √ √ Kings Wyckoff Heights Medical Center √ √ √ √ Kings Total Hospitals in Kings County 15 6 11 10 3 13 15 Cohen Children's Medical Center √ √ -

Newyork-Presbyterian Hospital Annual Report
Letters from Home 2006-2007 Annual Report NEWYORK-PRESBYTERIAN HOSPITAL Important Telephone Numbers THE ALLEN PAVILION OF NEWYORK-PRESBYTERIAN HOSPITAL NEWYORK-PRESBYTERIAN HOSPITAL/ WEILL CORNELL MEDICAL CENTER General Information (212) 932-4000 Patient Information (212) 932-4300 General Information (212) 746-5454 Admitting (212) 932-5079 Patient Information (212) 746-5000 Emergency Department (212) 932-4245 Admitting (212) 746-4250 Patient Services (212) 932-4321 Ambulance Services Dispatcher (212) 472-2222 Development (212) 821-0500 Emergency Department NEWYORK-PRESBYTERIAN HOSPITAL/ Adult (212) 746-5050 COLUMBIA UNIVERSITY MEDICAL CENTER Pediatric (212) 746-3300 General Information (212) 305-2500 Psychiatry (212) 746-0711 Patient Information (212) 305-3101 Human Resources (212) 746-1409 Admitting Marketing (212) 585-6800 Main Reception (212) 305-7091 NewYork-Presbyterian Sloane Hospital for Women (212) 342-1759 Healthcare System (212) 746-3577 Ambulance Services Dispatcher (212) 305-9999 Patient Services (212) 746-4293 Development (212) 342-0799 Physician Referral Service (800) 822-2694 Emergency Department Psychiatry, Payne Whitney Manhattan Adult (212) 305-6204 Referrals and Evaluation (888) 694-5700 Pediatric (212) 305-6628 General Information (212) 746-5700 Psychiatry (212) 305-6587 Public Affairs (212) 821-0560 Human Resources (212) 305-5625 Marketing (212) 821-0634 WESTCHESTER DIVISION OF NEWYORK-PRESBYTERIAN HOSPITAL Patient Services (212) 305-5904 Physician Referral Service (877) NYP-WELL General Information (914) 682-9100 Public Affairs (212) 305-5587 Payne Whitney Westchester Referrals and Evaluation (888) 694-5700 MORGAN STANLEY CHILDREN’S HOSPITAL Table of Contents OF NEWYORK-PRESBYTERIAN Physician Referral (800) 245-KIDS Letters from Home — 2 General Information (212) 305-KIDS Patient Information (212) 305-3101 Noteworthy — 24 Admitting (212) 305-3388 Leadership Report — 26 Emergency Department (212) 305-6628 Facts and Financials — 31 Dr. -
Community Health Needs Assessment and Implementation Plan
Community Health Needs Assessment and Implementation Plan 2016-2018 White Plains Hospital This document is submitted in accordance with the Internal Revenue Service’s Form 990 Schedule H requirements. White Plains Hospital Community Health Needs Assessment and Implementation Strategy 2016-2018 TABLE OF CONTENTS Page 1. Executive Summary 4 COMMUNITY HEALTH NEEDS ASSESSMENT 2. Introduction/Boiler Plate Language 9 a. White Plains Hospital’s Mission and Strategy b. Date CHNA Completed 3. Definition and Description of the Community/Service Area 11 a. The Population of the County b. Health Disparities c. Medically Underserved Communities 4. Assessment of Community Health Need 14 a. Description of Process and Methods i. Data Sources ii. Collaborations/Partnerships 1. Partners/Organizations a. Names of organizations b. Summary of Input Provided from Primary Data Sources c. Which medically underserved, low income or minority populations represented 5. Identification & Prioritization of Community Health Needs 18 a. Secondary Data Analysis b. Primary Data Analysis i. Online Survey 1. Process 2. Methods 3. Demographics 4. Results ii. Primary Data Analysis Key Findings 5. Key Findings from Quantitative Analysis 6. Key Findings from Qualitative Analysis IMPLEMENTATION STRATEGY 6. Measures and Identified Resources to Meet Identified Needs 50 a. Internal Resources and Measures 2 b. New York State Health Improvement Plan - Implementation Plan and Measures c. External Resources and Linkages to Meet Needs not addressed 7. Appendices 115 A. Primary Data Collection Materials i. Community Survey – English ii. Community Survey – Spanish B. White Plains Hospital Community Service Inventory 3 1. Executive Summary The Community Health Needs Assessment Requirement The Affordable Care Act requires hospitals to assess and address the health needs of the communities they serve. -
Multimodal Transportation Center Redevelopment Project
Multimodal Transportation Center Redevelopment Project TASK 4.1 – FINAL EXISTING CONDITIONS REPORT FINAL June 30, 2016 Version 1.1 Prepared for: The City of White Plains Prepared by: TASK 4.1 – FINAL EXISTING CONDITIONS REPORT CONTENTS 1 INTRODUCTION .................................................................................................................................................................. 1 1.1 PROJECT OVERVIEW ................................................................................................................................................ 1 1.2 STUDY AREA ............................................................................................................................................................... 1 1.3 REPORT PURPOSE ..................................................................................................................................................... 2 2 KEY FINDINGS OF THE BASELINE STUDIES .................................................................................................................... I 2.1 PEDESTRIAN CONDITIONS KEY FINDINGS .......................................................................................................... I 2.2 TRAFFIC AND PARKING KEY FINDINGS ...............................................................................................................VI 2.3 LAND USE, URBAN DESIGN, AND DEVELOPMENT KEY FINDINGS .............................................................. IX 2.4 MARKET CONDITIONS KEY FINDINGS ............................................................................................................... -

How Safe Is Your Hospital?
FEATURE SURGICAL INFECTION Patrick Roth of Dartmouth, Mass., can’t walk unassisted since he experienced several complications after surgery. the government doesn’t adequately track it as it does deaths from automobiles, plane crashes, and cancer. It’s appalling.” How safe is That lack of information not only makes it difficult to define the extent of the prob- lem but also makes it challenging for pa- tients to know about the safety of the your hospital? hospitals in their communities. To address that problem, Consumer Our new Ratings find too many pose risks Reports has for the first time rated hospi- tals for safety, using the most current data ospitals should be places says. “That’s like wiping out the entire pop- available to us at the time of our analysis. you go to get better, but too of- ulations of North Dakota, Rhode Island, It included information from government ten the opposite happens. and Vermont. It’s a man-made disaster.” and independent sources on 1,159 hospi- Infections, surgical mistakes, Some hospitals have responded to the tals in 44 states. For this report, we also Hand other medical harm contribute to the crisis with safety initiatives such as elec- interviewed patients, physicians, hospi- deaths of 180,000 hospital patients a year, tronic prescribing to help prevent drug er- tal administrators, and safety experts; re- according to projections based on a 2010 rors and checklists to prevent infections, viewed medical literature; and looked at report from the Department of Health and with some success. Rates of central-line hospital inspections and investigations. -

Index of North Castle History, Volume 26, 1999
INDEX FOR NORTH CASTLE HISTORY Volumes 1 (1974) through 30 (2003) by Sharon Tomback Letters L - Z (The volume year and page number, if available, appear as the last entry on each line) =============================================================== L L. Cundy & Co., Rubber Dealer, 1989:16 L.E. Preston & Co., Philadelphia, 1985:22 La Cremaillere French Restaurant, 2000:29 La Cremaillere Restaurant, 1990:23 La Cremaillere, 2000:23 La Rochelle, France, 1998:5 Labels, 1998:10 labor of love, 1993:5 Labor unions, 1987:20 laborer, 1989:20, 21 Labriola, Lawrence, 1978:10 Lacko, Frank, 1995:9 LaCremaillere Restaurant, 1981:3 Lada Mocarski, Valerin, 1995:9 Ladies' Aid Society, 1983:11 Ladies Aid Society, 1992:5 Ladies Guild, 1992: 9 Ladies Sewing Society, 1992:4 Ladies’ Shoes, 1997:12 Laet, John de, 1979:27 Lafayette Avenue, 1976:10 Lafayette, 1975:13 LaGuardia, Mayor Fiorello, 1976:7 Lafayette, General, 1991:23 LaFever, Miss Anna, 1984:14 Lake Champlain, 1980:31 Lake Champlain, 1985:23 Lake Champlain, 1987:11 Lake Mahopac, 1990:16, 17, 21 Lake Street, White Plains, 1988:10 Lake Street, White Plains, 2000:25 Lake View Hotel, Kensico, 1983:27 Lake View Hotel, Raven's, 1983:8 Lake Waccabuc, 1976:16 Lake, Old Kensico, 1983:17 Lakes, 2002:12, 18 Lakes, four artificial, 1998:21 Lakes, interconnected, 1998:21 Lambelet, Clarence A., 1992:3 Lambert, 1983:18 Lamont, Reverend Thomas, 1987:5 Lamp burning out, 1987:23 lamplight, 1994:10 Land Records and Wills, 1980:25 Land Records Office, Westchester County, 1975:9 Land Records, County Clerk's Office, 1989:27 Land Records, Deeds and Mortgages, Westchester Co. -

Westchester County Department of Health Community Health Assessment 2019
Westchester County 2019 Community Health Assessment Supplemental Data Report V: Emergency Room Utilization Project Director Jiali Li, PhD, Director of Research & Evaluation Renee Recchia, MPH, Acting Deputy Commissioner of Administration Project Staff Thomas Peer, MPH, Medical Data Analyst Contact Jiali Li, PhD Westchester County Department of Health, Planning & Evaluation 10 County Center Road, 2nd Floor, White Plains, New York, 10607 FOREWORD The Westchester County Department of Health (WCDH) plays a leading role in promoting health, preventing disease, and prolonging meaningful life for Westchester County residents. The WCDH’s ongoing mission involves monitoring and controlling the spread of diseases, regulating air and water quality, enforcing state and local sanitary codes, promoting and endorsing local public health activities, and ensuring the availability of community health services. To comply with New York State Public Health Law, WCDH has collaborated with local hospitals and other community health partners to complete a Community Health Assessment (CHA) Survey, which describes the current health status of Westchester County residents, identifies existing gaps and health care barriers, assesses the availability and accessibility of health care services, and specifies public health priorities in the county. In addition, a Community Health Improvement Plan (CHIP) has been crafted to lay out the specific objectives, goals, and actions of the Health Department which address the public health priorities identified in the Community Health Assessment. Supplementing the Westchester County Community Health Assessment (CHA) and Community Health Improvement Plan (CHIP), 2019-2021, six additional data reports are compiled to provide detailed data addressing specific areas relevant to the county’s public health. These reports are: Westchester County Community Health Assessment Supplemental Data Report 1.