The Management of Cardiac Arrest
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Commotio Cordis
Commotio Cordis Background Sudden unexpected cardiac death that occurs in young people during sports participation is usually associated with previously diagnosed or undiagnosed structural or primary electrical cardiac abnormalities. Examples of such abnormalities include hypertrophic cardiomyopathy, anomalous origin of a coronary artery, arrhythmogenic right ventricular cardiomyopathy, and primary electrical disorders, such as congenital prolongation of the QTc interval and catecholaminergic, polymorphic ventricular tachycardia (CPVT). Sudden death due to ventricular fibrillation may also occur following a blunt, nonpenetrating blow to the chest, specifically the precordial area, in an individual with no underlying cardiac disease. This is termed commotio cordis. Much of our understanding of the clinical and pathophysiologic aspects of commotio cordis is the result of work by N.A. Mark Estes III, MD, and Mark S. Link, MD, from the New England Cardiac Arrhythmia Center at the Tufts University and School of Medicine in Boston, Massachusetts and data derived from the US Commotio Cordis Registry (Minneapolis, Minnesota). Relatively recent data from the registry of the Minneapolis Heart Institute Foundation show that commotio cordis is one of the leading cause of sudden cardiac death in young athletes, exceeded only by hypertrophic cardiomyopathy and congenital cornoary artery abnormalities.[1] Commotio cordis typically involves young, predominantly male, athletes in whom a sudden, blunt, nonpenetrating and innocuous-appearing trauma to the anterior chest results in cardiac arrest and sudden death from ventricular fibrillation. The rate of successful resuscitation remains relatively low but is improving slowly. Although commotio cordis usually involves impact from a baseball, it has also been reported during hockey, softball, lacrosse, karate, and other sports activities in which a relatively hard and compact projectile or bodily contact caused impact to the person's precordium. -

Prolonged Asystole During Hypobaric Chamber Training
Olgu Sunumları Anadolu Kardiyol Derg 520 Case Reports 2012; 12: 517-24 contraction/ventricular tachycardia’s originating from mitral annulus contractions arising from the mitral annulus: a case with a pure annular are rarely reported (1). origin. Pacing Clin Electrophysiol 2009; 32: 680-2. [CrossRef] PVCs arising from the mitral annulus frequently originate from 5. Kimber SK, Downar E, Harris L, Langer G, Mickleborough LL, Masse S, et al. anterolateral, posteroseptal and posterior sites (2). It has been reported Mechanisms of spontaneous shift of surface electrocardiographic configuration that 2/3 of the PVCs arising from the mitral annulus originate from during ventricular tachycardia. J Am Coll Cardiol 1992; 15: 1397-404. [CrossRef] anterolateral site (2). Furthermore, small part of these arrhythmias origi- Address for Correspondence/Yaz›şma Adresi: Dr. Ömer Uz nates from the anteroseptal site of the mitral annulus. Ablation of this Gülhane Askeri Tıp Akademisi Haydarpasa, Kardiyoloji Kliniği, İstanbul-Türkiye site may be technically very challenging. Cases have been reported that Phone: +90 216 542 34 65 Fax: +90 216 348 78 80 successful catheter ablation of the premature ventricular contraction E-mail: [email protected] origin from the anteroseptal site of the mitral annulus can be performed Available Online Date/Çevrimiçi Yayın Tarihi: 22.06.2012 either by a transseptal or transaortic approach in literature (3, 4). ©Telif Hakk› 2012 AVES Yay›nc›l›k Ltd. Şti. - Makale metnine www.anakarder.com web Anterolateral site of the mitral annulus is in close proximity to anterior sayfas›ndan ulaş›labilir. of the right ventricle outflow tract, left ventricular epicardium near to ©Copyright 2012 by AVES Yay›nc›l›k Ltd. -

Medical Memoranda MEDICAJHRNA Haemodynamic Effects of Balloon
27 January 1968 Medical Memoranda MEDICAJHRNA 225 he had been after the myocardial infarction in March 1967. There- He was readmitted on 6 September again in supraventricular after he was maintained on lignocaine infusion 1 mg./min. to a tachycardia and with evidence of congestive failure. On three maximum of 500 mg. in 24 hours and remained in sinus rhythm for occasions over the next 48 hours a precordial thump converted this Br Med J: first published as 10.1136/bmj.1.5586.225 on 27 January 1968. Downloaded from 48 hours with only occasional extrasystoles. By this time the rhythm to sinus rhythm. On each occasion the procedure was infusion had been discontinued and he felt well, was in sinus performed with the patient monitored on the cardioverter, and with rhythm 80/min., and the blood pressure was 120/70. the shock paddles prepared and an intravenous drip available for At this time he suddenly relapsed to the original dysrhythmia- giving sodium bicarbonate or other drugs in the event of more supraventricular tachycardia with right bundle-branch block. On serious arrhythmia developing. In view of the continuing cardiac this occasion, as an alternative to further electrical cardioversion irritability with multifocal extrasystoles he was then put on a but while being monitored on the " cardioverter," he was given a procainamide continuous infusion, 4 g. in 24 hours, which had the sharp blow on the sternum with no effect. A similar heavy thump effect of almost clearing the ventricular ectopic beats. with the ulnar side of the clenched fist on the precordium at the cardiac apex immediately induced sinus rhythm with left bundle- COMMENT branch block (see Fig.). -

Precordial Thump
practical procedures resuscitation skills – part five Precordial thump phil Jevon, pGce, Bsc, rN, is tachycardia, asystole and resuscitation officer/clinical skills complete heart block where a lead, Manor Hospital, Walsall. precordial thump was delivered. The results were as follows: The precordial thump is a blow to l Ninety-one (49%) reverted to the lower half of the patient’s normal sinus rhythm; sternum using the lateral aspect l Seventy-seven (41%) had no of a closed fist. It can successfully change in rhythm; resuscitate the patient when l Nineteen (10%) were worse; given promptly following a l Overall, 90% of patients were cardiac arrest caused by either better or no change and Fig 1. check carotic pulse ventricular fibrillation (VF) or 10% were worse. ventricular tachycardia (VT) (Resuscitation Council (UK), 2006). Procedure This article describes the On discovering a collapsed procedure for delivering a unconscious patient: precordial thump. l Call out for help and activate the emergency buzzer; Mechanism of action l Lie the patient flat; The rationale for delivering a l Look, listen and feel for no precordial thump is that it longer than 10 seconds to generates a mechanical energy, determine if the patient is which is converted to electrical breathing normally (an occasional energy, which then may be gasp, slow, laboured or noisy sufficient to achieve successful breathing is abnormal) or has other cardioversion (Kohl et al, 2005). signs of life (Resuscitation Council Following the onset of VF, the (UK), 2006). If trained and threshold for successful experienced in assessing ill defibrillation rises steeply after a patients, a simultaneous Fig 2. -

Ventricular Rhythms Originate Below the Branching Portion of The
Northwest Community Healthcare Paramedic Program VENTRICULAR DYSRHYTHMIAS Pacemakers Connie J. Mattera, M.S., R.N., EMT-P Reading assignments: Bledsoe Vol 3; pp. 96-109 SOPs: VT with pulse; Ventricular fibrillation/PVT; Asystole/PEA Drugs: Amiodarone, magnesium, epinephrine 1mg/10mL Procedure manual: Defibrillation; Mechanical Circulatory Support (MCS) using a Ventricular Assist Device KNOWLEDGE OBJECTIVES: Upon completion of the reading assignments, class and homework questions, reviewing the SOPs, and working with their small group, each participant will independently do the following with at least an 80% degree of accuracy and no critical errors: 1. Identify the intrinsic rates, morphology, conduction pathways, and common ECG features of ventricular beats/rhythms. 2. Identify on a 6-second strip the following: a) Idioventricular rhythm b) Accelerated idioventricular rhythm c) Ventricular tachycardia: monomorphic & polymorphic d) Ventricular escape beats e) Premature Ventricular Contractions (PVCs) f) Ventricular fibrillation g) Asystole h) Paced rhythms i) Intraventricular conduction defects (Bundle branch blocks) 3. Systematically evaluate each complex/rhythm for the following: a) Rate (atrial and ventricular) b) Rhythm: Regular/irregular - R-R Interval, P-P Interval c) Presence/absence/morphology of P waves d) Presence/absence/morphology of QRS complexes d) P-QRS relationships f) QRS duration 4. Correlate the cardiac rhythm with patient assessment findings to determine the emergency treatment for each rhythm according to NWC EMSS SOPs. 5. Discuss the action, prehospital indications, side effects, dose and contraindications of the following during VT a) Amiodarone b) Magnesium 6. Describe the indications, equipment needed, critical steps, and patient monitoring parameters for cardioversion and defibrillation. 7. Identify the management of a patient with an implanted defibrillator and/or pacemaker. -

The Unsuspected Complications of Bacterial Endocarditis Imaged by Gallium-67 Scanning
The Unsuspected Complications of Bacterial Endocarditis Imaged by Gallium-67 Scanning Shobha P. Desai and David L. Yuille Nuclear Medicine Department, St. Luke's Medical Center, Milwaukee, @V&sconsin tivity in the region of the aortic valve which extended into the In this case report, we present a patient with bacterial endocar right atrium (Fig. 1)but was better appreciated on an axial SPECF ditiswho was evaluatedby 67(@imagingfor persistentfever image (Fig. 2). despitetreatmentwith multipleintravenousantibiotics.Afthough cardiac catheterizationconfirmeda densely calcified bicuspid evidence of bactenal endocarditiswas absent wfth @“Gaimag aorticvalve with both stenosis and insufficiencyas well as what ing,the studydemonstratedfindingsthat representcomplica was thoughtto be aveiy largerightsinus ofvalsalva aneurysm.At tions of bacterial endocarditis. The procedure demonstrated surgery, there was evidence of epicarditisand pericarditisand a moderatepencardialuptakeof isotopeandthus pro@4dedthe hugerightsinus of valsalva abscess was foundwhich was eroding first evidence of pehcardi@swhich was later confirmed at sur into the aortic wall. The aortic valve annuluswas debrided, the gery.The studyalsodemonstratedmi@ increasedactivityin abscess cavity was drainedandthe patient's diseased aorticvalve thevicinityoftheaorticrootandnghtattium.A sinusofvalsalva was replacedwith a no. 25 St. Jude's prosthesis (St. JudeMedical abscess, complicatingthe underlyingdiagnosis of bacterialen Inc., St. Paul, MN). The immediatepostoperativeperiodwas docarc@bs,was -

Cardiac Arrhythmias in Survivors of Sudden Cardiac Death Requiring Impella Assist Device Therapy
Journal of Clinical Medicine Article Cardiac Arrhythmias in Survivors of Sudden Cardiac Death Requiring Impella Assist Device Therapy Khaled Q. A. Abdullah 1,2, Jana V. Roedler 1, Juergen vom Dahl 1, Istvan Szendey 1, Dimitrios Dimitroulis 1, Lars Eckardt 3, Albert Topf 4, Bernhard Ohnewein 4, Lorenz Fritsch 4, Fabian Föttinger 4, Mathias C. Brandt 4, Bernhard Wernly 4,5,6 , Lukas J. Motloch 4 and Robert Larbig 2,3,* 1 Department of Cardiology, Hospital Maria Hilf Moenchengladbach, 41063 Moenchengladbach, Germany; [email protected] (K.Q.A.A.); [email protected] (J.V.R.); [email protected] (J.v.D.); [email protected] (I.S.); [email protected] (D.D.) 2 Department of Cardiology, University Hospital Aachen, RWTH University Aachen, 52062 Aachen, Germany 3 Department of Cardiovascular Medicine, Division of Electrophysiology, University of Muenster, 48149 Muenster, Germany; [email protected] 4 Department of Cardiology, Clinic II for Internal Medicine, University Hospital Salzburg, Paracelsus Medical University, 5020 Salzburg, Austria; [email protected] (A.T.); [email protected] (B.O.); [email protected] (L.F.); [email protected] (F.F.); [email protected] (M.C.B.); [email protected] (B.W.); [email protected] (L.J.M.) 5 Department of Anesthesiology, Perioperative Medicine and Intensive Care Medicine, Paracelsus Medical University of Salzburg, 5026 Salzburg, Austria 6 Center for Public Health and Healthcare Research, Paracelsus Medical University of Salzburg, 5026 Salzburg, Austria Citation: Abdullah, K.Q.A.; Roedler, * Correspondence: [email protected]; Tel.: +49-216-1892-4770 J.V.; vom Dahl, J.; Szendey, I.; Dimitroulis, D.; Eckardt, L.; Topf, A.; Abstract: In this retrospective single-center trial, we analyze 109 consecutive patients (female: 27.5%, Ohnewein, B.; Fritsch, L.; Föttinger, F.; median age: 69 years, median left ventricular ejection fraction: 20%) who survived sudden cardiac et al. -
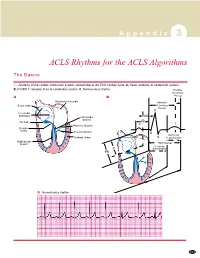
ACLS Rhythms for the ACLS Algorithms
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with -

Severe Hypotension, Bradycardia and Asystole After Sugammadex Administration in an Elderly Patient
medicina Case Report Severe Hypotension, Bradycardia and Asystole after Sugammadex Administration in an Elderly Patient Carmen Fierro 1 , Alessandro Medoro 1 , Donatella Mignogna 1 , Carola Porcile 1 , Silvia Ciampi 1 , Emanuele Foderà 1 , Romeo Flocco 2, Claudio Russo 1,3,* and Gennaro Martucci 2 1 Department of Medicine and Health Sciences, University of Molise, 86100 Campobasso, Italy; c.fi[email protected] (C.F.); [email protected] (A.M.); [email protected] (D.M.); [email protected] (C.P.); [email protected] (S.C.); [email protected] (E.F.) 2 Anesthesia and Intensive Care Unit, “A. Cardarelli” Hospital, Azienda Sanitaria Regionale del Molise, 86100 Campobasso, Italy; romeofl[email protected] (R.F.); [email protected] (G.M.) 3 UOC Governance del Farmaco, Azienda Sanitaria Regionale del Molise, 86100 Campobasso, Italy * Correspondence: [email protected] Abstract: Background and Objectives: Sugammadex is a modified γ-cyclodextrin largely used to prevent postoperative residual neuromuscular blockade induced by neuromuscular aminosteroid blocking agents. Although Sugammadex is considered more efficacious and safer than other drugs, such as Neostigmine, significant and serious complications after its administration, such as hypersen- sitivity, anaphylaxis and, more recently, severe cardiac events, are reported. Case presentation: In this report, we describe the case of an 80-year-old male with no medical history of cardiovascular disease who was scheduled for percutaneous nephrolithotripsy under general anesthesia. The intraoperative course was uneventful; however, the patient developed a rapid and severe hypotension, asystole and cardiac arrest after Sugammadex administration. Spontaneous cardiac activity and hemodynamic Citation: Fierro, C.; Medoro, A.; stability was restored with pharmacological therapy and chest compression. -

Cardiac Lesions Associated with Cardiopulmonary Resuscitation
Rom J Leg Med [19] 1-6 [2011] DOI: 10.4323/rjlm.2011.1 © 2011 Romanian Society of Legal Medicine Cardiac lesions associated with cardiopulmonary resuscitation George Cristian Curcă1, Dan Dermengiu2, Mihai Ceaușu3, Adriana Francisc4, Mugurel Constantin Rusu5, Sorin Hostiuc6 ___________________________________________________________________________________________________________ Abstract: Cardiac arrest is a major cause of morbidity and mortality across the world despite the fact that significant advances were made in basic and advanced life support techniques. Cardiac lesions during CPR are rare, and usually are not involved in thanatologic chains. They can however lead to severe or even lethal complications and may be difficult to differentiate from non-iatrogen trauma, especially in traumatic deaths. We present in this article four cases of cardiac lesions associated with resuscitated cardiac arrest, discuss their forensic significance and review the most important iatrogen cardiac lesions associated with cardiopulmonary resuscitation. Keywords: cardiac contusion, myocardial lesions, cardiopulmonary resuscitation ardiac arrest is a major cause of morbidity and mortality across the world despite the fact that significant advances were made in basic and advanced life support C techniques. Even though cardiopulmonary resuscitation has an overall success rate of 30-40%[1], over 50% of all resuscitated patients die before leaving the hospital, usually due to cardiovascular or CNS complications[2]; many successful resuscitations are in turn -

Part 3: Defibrillation
Resuscitation (2005) 67, 203—211 Part 3: Defibrillation International Liaison Committee on Resuscitation The 2005 Consensus Conference considered ques- sic devices achieve higher first-shock success rates tions related to the sequence of shock delivery than monophasic defibrillators. This fact, combined and the use and effectiveness of various waveforms with the knowledge that interruptions to chest and energies. These questions have been grouped compressions are harmful, suggests that a one- into the following categories: (1) strategies before shock strategy (one shock followed immediately by defibrillation; (2) use of automated external defib- CPR) may be preferable to the traditional three- rillators (AEDs); (3) electrode-patient interface; (4) shock sequence for VF and pulseless ventricular use of the electrocardiographic (ECG) waveform to tachycardia (VT). alter management; (5) waveform and energy lev- els for the initial shock; (6) sequence after failure of the initial shock (i.e. second and subsequent Strategies before defibrillation shocks; and (7) other related topics. The International Guidelines 20001 state that Precordial thump defibrillation should be attempted as soon as ven- W59,W166B tricular fibrillation (VF) is detected, regardless of the response interval (i.e. time between collapse Consensus on science. No prospective studies and arrival of the AED). If the response interval have evaluated the use of the precordial (chest) is >4—5 min, however, there is evidence that thump. In three case series (LOE 5)2—4 VF or pulse- 1.5—3 min of CPR before attempted defibrillation less VT was converted to a perfusing rhythm by a may improve the victim’s chance of survival. -

Fire Fighter FACE Report No. F2005-16, Captain Suffers an Acute Aortic Dissection After Responding to Two Alarms and Subsequentl
F2005 16 A Summary of a NIOSH fi re fi ghter fatality in ves ti ga tion August 24, 2005 Captain Suffers an Acute Aortic Dissection After Responding to Two Alarms and Subsequently Dies Due to Hemopericardium – Pennsylvania SUMMARY On January 21, 2004, a 35-year-old male vol- signifi cant risk to the safety and health of unteer Captain responded to two alarms: a mo- themselves or others. tor vehicle crash (MVC) with an injury, and a reported house fi re that turned out to be a false • Perform an annual physical performance alarm. Returning to the fi re station after the false (physical ability) evaluation to ensure alarm, he complained of not feeling well and went fi re fi ghters are physically capable of home. After being home about 15 minutes, he performing the essential job tasks of collapsed. The Captain was transported to the lo- structural fi re fi ghting. cal hospital and later fl own to a regional hospital for diagnostic testing. Despite having a cardiac • Phase in a mandatory wellness/fi tness pro- catheterization with coronary angiography, and a gram for fi re fi ghters to reduce risk factors chest computed tomography (CT) scan, his aortic for cardiovascular disease and improve dissection went undiagnosed. He was treated for cardiovascular capacity. bilateral pneumonia but his condition continued to deteriorate. Despite cardiopulmonary resus- • Ensure that fi re fi ghters are cleared for citation (CPR) and advanced life support (ALS), duty by a physician knowledgeable about the Captain was pronounced dead approximately the physical demands of fi re fi ghting, the 20 hours after his initial complaint.