Headmasters Epigenetic Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
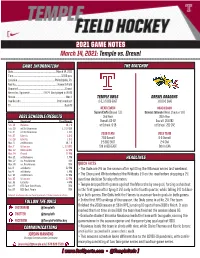
2021 GAME NOTES March 14, 2021: Temple Vs. Drexel
2021 GAME NOTES March 14, 2021: Temple vs. Drexel GAME INFORMATION THE MATCHUP Date ...........................................................................March 14, 2021 Time ................................................................................... 12:00 p.m. Location .................................................................Philadelphia, Pa. Facility ........................................................................Howarth Field Opponent ..................................................................................Drexel Record vs. Opponent .......................19-12-1 (last played in 2019) Streak .......................................................................................Won 1 TEMPLE OWLS DREXEL DRAGONS Live Results...............................................................Statbroadcast 2-5, 1-5 BIG EAST 1-0 (0-0 CAA) TV .............................................................................................OwlsTV HEAD COACH HEAD COACH Susan Ciufo (Drexel ‘11) Denise Zelenak (West Chester ‘91) 2021 SCHEDULE/RESULTS 2nd Year 26th Year Date Opponent Time/Result Overall: 63-42 Overall: 251-242 Feb. 12 Hofstra W, 1-0 at School: 9-15 at School: 251-242 Feb. 20 at Old Dominion L, 2-3 (SO) Feb. 21 at Old Dominion L, 0-1 2019 TEAM 2019 TEAM Feb. 27 Liberty L, 0-2 Feb. 28 Liberty L, 0-2 7-10 Overall 9-9 Overall Mar. 6 at Villanova W, 1-0 2-5 BIG EAST 2-4 CAA Mar. 7 Villanova L, 1-2 (OT) 5th in BIG EAST 6th in CAA Mar. 12 Monmouth 12 PM Mar. 14 Drexel 12 PM Mar. 21 at Delaware 1 PM HEADLINES Mar. 27 vs. Providence TBA Mar. 28 vs. Providence TBA QUICK FACTS Apr. 3 at Liberty 12 PM > The Owls are 2-5 on the season after splitting the Villanova series last weekend. Apr. 4 at Liberty 1 PM Apr. 10 at Villanova 12 PM > The Cherry and White defeated the Wildcats 1-0 on the road before dropping a 2-1 Apr. 10 Villanova 12 PM overtime decision Sunday afternoon. -

Chevalier Jackson Collection of Photographs and Etchings 1990-108
Chevalier Jackson collection of photographs and etchings 1990-108 Last updated on September 14, 2018. Historical Medical Library of The College of Physicians of Philadelphia 2012 Chevalier Jackson collection of photographs and etchings Table of Contents Summary Information....................................................................................................................................3 Biography/History..........................................................................................................................................3 Scope and Contents....................................................................................................................................... 4 Administrative Information........................................................................................................................... 4 - Page 2 - Chevalier Jackson collection of photographs and etchings Summary Information Repository Historical Medical Library of The College of Physicians of Philadelphia Title Chevalier Jackson collection of photographs and etchings Call number 1990-108 Date 1923-1957 Extent 1.5 linear feet Language English Biography/History Chevalier Jackson (1865-1958) was a laryngologist. Jackson attended the Western University of Pennsylvania (now the University of Pittsburgh) from 1879 to 1883, and received his MD from Jefferson Medical College. He also studied laryngology with the British specialist Sir Morell McKenzie. In the course of his career Jackson introduced many improved techniques -

Chevalier Jackson, MD
Thomas Jefferson University Jefferson Digital Commons Department of Surgery Gibbon Society Historical Department of Surgery Profiles 5-1-2013 Chevalier Jackson, M.D. (1865-1958): Il ne se repose jamais. Phi D Nguyen, B.A. Thomas Jefferson University Scott .W Cowan, MD Thomas Jefferson University, [email protected] Charles J. Yeo, MD Thomas Jefferson University, [email protected] Nathaniel R. Evans III, M.D. Thomas Jefferson University, [email protected] Let us know how access to this document benefits ouy Follow this and additional works at: https://jdc.jefferson.edu/gibbonsocietyprofiles Part of the History of Science, Technology, and Medicine Commons, and the Surgery Commons Recommended Citation Nguyen, B.A., Phi D; Cowan, MD, Scott .;W Yeo, MD, Charles J.; and Evans III, M.D., Nathaniel R., "Chevalier Jackson, M.D. (1865-1958): Il ne se repose jamais." (2013). Department of Surgery Gibbon Society Historical Profiles. Paper 17. https://jdc.jefferson.edu/gibbonsocietyprofiles/17 This Article is brought to you for free and open access by the Jefferson Digital Commons. The effeJ rson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The ommonC s is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The effeJ rson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Surgery Gibbon Society Historical Profiles by an authorized administrator of the Jefferson Digital Commons. -
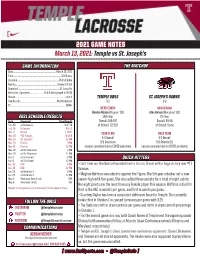
2021 GAME NOTES March 13, 2021: Temple Vs St. Joseph's
2021 GAME NOTES March 13, 2021: Temple vs St. Joseph’s GAME INFORMATION THE MATCHUP Date ...........................................................................March 13, 2021 Time ................................................................................... 12:00 p.m. Location .........................................................................Philadelphia Facility ........................................................................Howarth Field Opponent ........................................................................St. Joseph’s Record vs. Opponent ........................19-4-0 (last played in 2019) Streak .......................................................................................Lost 3 TEMPLE OWLS ST. JOSEPH’S HAWKS Live Results...............................................................StatBroadcast 3-1 2-2 TV ...............................................................................................ESPN+ HEAD COACH HEAD COACH Bonnie Rosen (Virginia ‘93) Alex Kahoe (Maryland ‘00) 2021 SCHEDULE/RESULTS 15th Year 7th Year Date Opponent Time/Result Overall: 189-197 Overall: 54-48 Feb. 20 at Delaware W 17-10 at School: 121-116 at School: Same Feb. 26 Villanova W 17-2 Mar. 3 Drexel L 19-11 2019 TEAM 2019 TEAM Mar. 10 #11 Towson W 12-8 Mar. 13 St. Joseph’s 12 PM 5-4 Overall 4-3 Overall Mar. 19 Florida 3 PM 0-0 American 0-0 Atlantic-10 Mar. 21 Florida 12 PM season canceled due to COVID pandemic season canceled due to COVID pandemic Mar. 26 at Old Dominion 4 PM Mar. 28 at Old Dominion 11 AM Apr. 2 at Cincinnati 3 PM QUICK HITTERS Apr. 4 at Cincinnati 12 PM Apr. 16 ECU 4 PM > Last time out the Owls rebounded from a loss to Drexel with a huge victory over #11 Apr. 18 ECU 12 PM Towson. Apr. 23 at Vanderbilt 3 PM Apr. 25 at Vanderbilt 12 PM > Meghan Hoffman was electric against the Tigers. The 5th year attacker set a new May 6 American Semifinals TBA career-high with five goals. -

Accepting 2019 Scholarship Applications Green Upgrades for Your Home
MoneyLineLine ACCEPTING 2019 SCHOLARSHIP APPLICATIONS GREEN UPGRADES FOR YOUR HOME BE CAREFUL ABOUT SHARING PERSONAL INFORMATION APRIL 2019 PHILADELPHIA FEDERAL CREDIT UNION PFCU IN ACTION SPREADING SOME CHEER OVER THE HOLIDAY SEASON PFCU employees purchased gifts including blankets, towels and clothing for the women at Gaudenzia House of Passage, a local nonprofit organization that provides supportive services for single women in the community. On Wednesday, December 19, representatives from PFCU’s Marketing Department were so excited to deliver the gifts and spread some holiday cheer to the residents. Residents and staff from House of Passage and PFCU. From left to right top row: Lisa, resident; Mary Simmons, VP of Marketing, PFCU; Tamika Artis, Program Supervisor HOP; Karen Williams, Case Manager Supervisor HOP; Erin Ellis, Financial Educator, PFCU. From left to right bottom row: Shawn, Brenda, Ethel, residents and Mary Posluszny, Marketing Manager, PFCU. Erin Ellis, PFCU’s Accredited Financial Counselor, meets with three residents of Depaul USA, which received the highest number of votes in the credit union’s Annual In This Issue: Giving Campaign. PFCU DONATES $5,000 TO SUPPORT THREE LOCAL NONPROFIT PFCU Board of Directors – In the Spotlight ...................................3 ORGANIZATIONS PFCU donated $5,000 to three local nonprofit organizations based Thinking about an RV? Great View, Great Relaxation, Great Loans! ..................................................................................................3 on number of votes -
Hugh at Drexel
J-li; li ■iil' I' VOLUME XLVI C ipy rig ti!, 1970 T h i O re x tl T rian g le FRIDAY, MARCH 6, 1970 NUMBER 57 i i'l The following article is reprinted ivith permission from The En kaU-yuga, fires caused by the stupidity of those who think things vironmental Handbook, edited b y Garrett DeBell. The author of the can be gained and lost whereas in truth all is contained vast and article wishes to remain anonymous. free in the Blue Sky and Green Earth of One Mind. Round-bellied to show his kind of nature and that the great Once in the Jurassic, about 150 million years ago, the Great earth has food enough for everyone who loves and trusts her. Sun Buddha In this com er of the Infinite Void gave a great Dis Trampling underfoot wasteful freeways and needless suburbs; s m o k e y course to all the assembled elements and energies: to the stand smashing the worms of capitalism and totalitarianism. ing beings, the walking beings, the flying beings, and the sitting Indicating the Task: his followers, becoming free of cars, beings — even grasses, to the number of thirteen bilUon, each houses, canned food, universities and shoes, master the Three one bom from a seed, were assembled there: a Discourse con Mysteries of their own Body, Speech and Mind, and fearlessly cerning Enlightenment on the planet Earth. chop down the rotten trees and prune out the sick limbs of this t h e “In some future time, there will be a continent called America. -

Halbzeit Temple Owls, Philadelphia Eagles, 6Ers
Halbzeit Temple Owls, Philadelphia Eagles, 6ers, Phillies. Falls die Namen euch allen jetzt nichts sagen: Kein Vorwurf. Mir vor meinem Auslandssemester auch nicht. Es handelt sich um Sportteams. Davon soll dieser Bericht handeln. Ich selbst bin als frenetischer Fußballspieler und Fan (es fällt mir immer noch schwer „Soccer“ zu sagen) in das Land gekommen, in dem der Fußball nicht mal an fünfter Stelle der beliebtesten Sportarten. Die über allem stehenden Sportarten hier sind American Football, Baseball, Basketball und Eishockey. Eins meiner Ziele dieses Auslandssemester für mich sportbegeisterten Menschen war es, Sport hier in Philadelphia zu erleben. Und darum geht es in meiner Halbzeitanalyse an der Temple University. Temple Owls vs Bucknell: 56:12 Meine erste Begegnung mit Sport war das erste Heimspiel der Temple Owl. Die Temple „Eule“ ist Teil des Coporate Designs der Universität und das Maskottchen der universitären Temple American Football Teams. Diese spielen in der NCAAF, der College Football league. Diese Spiele sind ein riesiges Event. Immatrikulierte Studierende können kostenlos das Spiel besuchen, es gibt zu jedem Heimspiel ein eigens dafür eingerichteten Shuttlebus zum Stadion. Wir fuhren also mit den berühmten gelben Schulbussen zum Lincoln Financial Field. Ein Stadion mit fast 70.000 Plätzen. Dort angekommen, staunten wir nicht schlecht, als auf den Parkplätzen rund um das Stadion eine große Sause war. Das sog. „Tailgaiting“ kannte ich jedenfalls noch nicht. Die Footballfans stimmen sich auf das Spiel ein: Mit dabei ein Grill, gekühlte Erfrischungsgetränke, kleine Spiele und Musik. Gestärkt von dem Temple University Tailgate gingen wir ins Stadion. Etwa 20.000 Zuschauer waren dann in den Farben Cherry and White erschienen. -

Electric Power Outlook for Pennsylvania 2018-2023 I Ii Electric Power Outlook for Pennsylvania 2017-2022
ELECTRIC POWER OUTLOOK FOR PENNSYLVANIA 2018–2023 August 2019 Published by: Pennsylvania Public Utility Commission 400 North Street Harrisburg, PA 17105-3265 www.puc.pa.gov Technical Utility Services Paul T. Diskin, Director Prepared by: David M. Washko - Reliability Engineer Electric Power Outlook for Pennsylvania 2018-2023 i ii Electric Power Outlook for Pennsylvania 2017-2022 Executive Summary Introduction Section 524(a) of the Public Utility Code (Code) requires jurisdictional electric distribution companies (EDCs) to submit to the Pennsylvania Public Utility Commission (PUC or Commission) information concerning plans and projections for meeting future customer demand.1 The PUC’s regulations set forth the form and content of such information, which is to be filed on or before May 1 of each year.2 Section 524(b) of the Code requires the Commission to prepare an annual report summarizing and discussing the data provided, on or before Sept. 1. This report is to be submitted to the General Assembly, the Governor, the Office of Consumer Advocate and each affected public utility.3 Since the enactment of the Electricity Generation Customer Choice and Competition Act,4 the Commission’s regulations have been modified to reflect the competitive market. Thus, projections of generating capability and overall system reliability have been obtained from regional assessments. Any comments or conclusions contained in this report do not necessarily reflect the views or opinions of the Commission or individual Commissioners. Although issued by the Commission, this report is not to be considered or construed as approval or acceptance by the Commission of any of the plans, assumptions, or calculations made by the EDCs or regional reliability entities and reflected in the information submitted. -

Explorer News February 2004 La Salle University
La Salle University La Salle University Digital Commons Explorer News University Publications 2-2004 Explorer News February 2004 La Salle University Follow this and additional works at: http://digitalcommons.lasalle.edu/athletics_explorer_news Recommended Citation La Salle University, "Explorer News February 2004" (2004). Explorer News. 9. http://digitalcommons.lasalle.edu/athletics_explorer_news/9 This Book is brought to you for free and open access by the University Publications at La Salle University Digital Commons. It has been accepted for inclusion in Explorer News by an authorized administrator of La Salle University Digital Commons. For more information, please contact [email protected]. The Newsletter of the Explorer Club February 2004 Message from Dr. Tom Brennan, La Salle Athletics Logo Unveiling Director of Athletics Greetings from 20th Street and Olney Avenue. The fall season was a rewarding one. It was mixed Dr. Thomas in terms of success on the athletic fields, but not in Brennan terms of success in the classroom or with regard to the efforts of our student athletes and coaches to enhance neighborhood activity. In the academic area, several of our teams received National Recognition for their work in the classroom with field hockey and men's tennis leading the way. The field hockey team accumulated a 3.47 GPA in the fall, while the men's tennis team had a 3.38. Several athletes earned A-10 and MAAC ac academic accolades and men's soc cer senior Matt Hemberger was named to the Middle Atlantic Regional All-American Academic Team. The NCAA reported La Salle's 10-year graduation rate for student-athletes at 84%. -

Chevalier Jackson, MD
Thomas Jefferson University Jefferson Digital Commons Department of Surgery Gibbon Society Historical Profiles Department of Surgery 5-1-2013 Chevalier Jackson, M.D. (1865-1958): Il ne se repose jamais. Phi D Nguyen, B.A. Thomas Jefferson University Scott W. Cowan, MD Thomas Jefferson University Charles J. Yeo, MD Thomas Jefferson University Nathaniel R. Evans III, M.D. Thomas Jefferson University Follow this and additional works at: https://jdc.jefferson.edu/gibbonsocietyprofiles Part of the History of Science, Technology, and Medicine Commons, and the Surgery Commons Let us know how access to this document benefits ouy Recommended Citation Nguyen, B.A., Phi D; Cowan, MD, Scott W.; Yeo, MD, Charles J.; and Evans III, M.D., Nathaniel R., "Chevalier Jackson, M.D. (1865-1958): Il ne se repose jamais." (2013). Department of Surgery Gibbon Society Historical Profiles. Paper 17. https://jdc.jefferson.edu/gibbonsocietyprofiles/17 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Surgery Gibbon Society Historical Profiles yb an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Surgical Leaders Chevalier Jackson, M.D. -

Reliving the Feb. 10, 1988 Temple-Villanova Classic Through the Pages of the Daily News and Inquirer
Reliving the Feb. 10, 1988 Temple-Villanova Classic Through the Pages of the Daily News and Inquirer Compiled by Bob Vetrone Jr. INDEX ► CLASH HAS PEOPLE LOOKING AHEAD (Feb. 5/Kevin Mulligan) ► TEMPLE MIGHT BECOME NO. 1 IN POLLS (Feb. 8/Kevin Mulligan) ► TEMPLE CLIMBS TO TOP OF POLLS (Feb. 9/Kevin Mulligan) ► WILDCATS FUELED BY LATEST POLLS ... (Feb. 10/Dick Weiss) ► … AS CHANEY TAKES ON HIS CRITICS (Feb. 10/Kevin Mulligan) ► DICK WEISS SIZES UP VILLANOVA (Feb. 10) ► KEVIN MULLIGAN SIZES UP TEMPLE (Feb. 10) ► OWLS OUTLAST NOVA IN BIG 5 MASTERPIECE (Feb. 11/Kevin Mulligan) ► MACON, EVANS LIFT OWLS TO 98-86 WIN (Feb. 11/M.G. Missanelli) ► BOX SCORE ► OWLS NEED A LARGER SHOWROOM (Feb. 11/Stan Hochman) ► EVANS DEALS 20 ASSISTS IN OWLS WIN (Feb. 11/Dick Weiss) ► EVANS’ GAME IS ONE TO REMEMBER (Feb. 11/Jayson Stark) ► WITH THE PRESSURE ON, THE OWLS COOKED (Feb. 12/M.G. Missanelli) VILLANOVA-TEMPLE CLASH HAS PEOPLE LOOKING AHEAD Feb.5, 1988 / Philadelphia Daily News By KEVIN MULLIGAN The heading at the top of the page says “TV Weekend,” but only on special occasions (and slow weekends) do we stray ahead to midweek TV happenings. Villanova vs. Temple Wednesday night at McGonigle Hall is one of those special occasions. Unless you’re one of the chosen 4,800 — yes, Temple has oversold McGonigle’s 4,500 capacity — the only place to catch the long-awaited City Series showdown will be on PRISM at 9 p.m. Out-of-town cable subscribers can tune in USA Network, which will carry the game nationally outside PRISM’s blackout radius. -

August 27, 2021: Temple Vs Penn
2021 WEEKLY NOTES August 27, 2021: Temple vs Penn MATCH INFORMATION THE MATCHUP Date ..........................................................................August 27, 2021 Time .....................................................................................4:00 p.m. Location .................................................................Philadelphia, Pa. Facility .......................................................Temple Sports Complex Opponent ....................................................................................Penn Record vs. Opponent ................................................................5-8-0 Streak ..............................................................................................L3 TEMPLE OWLS PENN QUAKERS Live Results...............................................................StatBroadcast 0-1 0-0 TV.................................................................................................ESPN+ (AAC 0-0) (IVY 0-0) HEAD COACH HEAD COACH Nick Bochette (Rensselaer ‘06) Casey Brown (Brown ‘10) 2021 SCHEDULE/RESULTS 5th year 4th Year Date Opponent Time/Result Aug. 19 at Maryland 0-3 L Overall: 33-30-7 Overall: 17-37-14 Aug. 22 at #25 Rutgers Canceled at School: 4-6-1 at School: 0-0 Aug. 27 vs. Penn 4:00 p.m. Aug. 29 vs. Binghamton 1:00 p.m. LAST GAME Sep. 2 at Towson 7:00 p.m. LAST GAME Sep. 4 vs. Rider 7:00 p.m. Loss at Maryland, 0-3 Loss at Princeton, 0-1 (2019) Sep. 9 at St. Joseph’s 7:00 p.m. Sep. 16 at Memphis* 8:00 p.m. 2019 LEADERS Sep. 19 vs. Drexel 1:00 p.m. 2020-21 LEADERS Sep. 23 vs. Cincinnati* 7:00 p.m. Goals......Gutowski, Johnson, McGovern (2) Goals................. Lawton (3) Sep. 30 vs. Tulsa* 7:00 p.m. Assists................. Endres (4) Assists................. Schachter (4) Oct. 7 at ECU* 7:00 p.m. Points.................Endres (6) Points................. Lawton (7) Oct. 17 vs. Houston* 12:00 p.m. Oct. 20 at SMU* 8:00 p.m. Saves................. Stablein (60) Saves................N/A Oct. 24 at UCF* 1:00 p.m.