Implementation Guide to Support Use of Elastomeric Half Mask Respirators in Healthcare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BFS 2005 Respiratory Protection Program
Bureau of Forensic Services Issue Date: Revision: Respiratory Protection Program 3/26/2007 1.0 Table of Contents Page #: 1 of 31 Issued by: Lance Gima, Chief 1. Introduction…………………………………………………….. 2 2. Responsibilities………………………………… …………….. 3 3. Definitions……………………………………………………. 5 4. Classification, Description and Limitations of Respirators……. 8 5. Selection of Respirators……………………………………….. 10 6. Use of Respirators……………………………………………… 13 7. Maintenance of Respirators……………………………………. 16 8. Special Issues…..………………………………………………. 18 9. Medical Evaluation…………………………………………….. 19 10. Program Evaluation……………………………………………. 20 Appendix A: Decision Logic for Respirator Selection…………….. 21 Appendix B: Respirator Change-out Schedules…………………… 24 Appendix C: SCBA Monthly Inspection Form……………………. 29 Appendix D: Manufacturer’s Safety Advisory Notices …………... 31 +++ALL PRINTER COPIES ARE UNCONTROLLED+++ Official document location: M:Safety Manual\respprot2007.pdf Bureau of Forensic Services Issue Date: Revision: Respiratory Protection Program 3/26/2007 1.0 Introduction Section 1.0 Page #: 2 of 31 Issued by: Lance Gima, Chief 1. INTRODUCTION Scope This program sets forth accepted practices for respirator users, and provides information and guidance on proper selection, use and maintenance of respirators. Purpose The purpose of this program is to ensure that the Bureau of Forensic Services Respiratory Protection Program provides guidance to all employees using respiratory protection. This program applies to all job related respiratory hazards encountered both in the field and in the laboratory with the exception of clandestine drug labs. Respiratory Protection requirements for response to clandestine drug labs are found in the BFS/BNE Clandestine Laboratory Manual for Instruction and Procedure. Permissible Practice When working in an environment containing harmful dusts, fumes, sprays, mist, fogs, smokes, vapors or gases, the primary method of protection for employees will be engineering control. -

Evaluation of Occupational Exposures to Illicit Drugs at Controlled Substances Laboratories
Evaluation of Occupational Exposures to Illicit Drugs at Controlled Substances Laboratories HHE Report No. 2018-0090-3366 January 2020 Authors: Kendra R. Broadwater, MPH, CIH David A. Jackson, MD Jessica F. Li, MSPH Analytical Support: Bureau Veritas North America Desktop Publisher: Aja Powers Editor: Cheryl Hamilton Industrial Hygiene Field Assistance: Karl Feldmann Logistics: Donnie Booher, Kevin Moore Medical Field and Analytic Assistance: Krishna Surasi, Marie de Perio Keywords: North American Industry Classification System (NAICS) 922120 (Police Protection), Maryland, Forensic Laboratory, Forensic Scientist, Forensic Chemist, Law Enforcement, Illicit Drug, Cocaine, Fentanyl, Heroin, Opioid, Methamphetamine Disclaimer The Health Hazard Evaluation Program investigates possible health hazards in the workplace under the authority of the Occupational Safety and Health Act of 1970 [29 USC 669a(6)]. The Health Hazard Evaluation Program also provides, upon request, technical assistance to federal, state, and local agencies to investigate occupational health hazards and to prevent occupational disease or injury. Regulations guiding the Program can be found in Title 42, Code of Federal Regulations, Part 85; Requests for Health Hazard Evaluations [42 CFR Part 85]. Availability of Report Copies of this report have been sent to the employer, employees, and union at the laboratories. The state and local health departments and the Occupational Safety and Health Administration Regional Office have also received a copy. This report is not copyrighted and may be freely reproduced. Recommended Citation NIOSH [2020]. Evaluation of occupational exposures to illicit drugs at controlled substances laboratories. By Broadwater KR, Jackson DA, Li JF. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Health Hazard Evaluation Report 2018-0090-3366, https://www.cdc.gov/niosh/hhe/reports/pdfs/2018-0090-3366.pdf. -
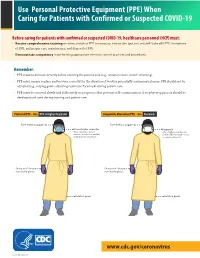
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -
Elastomeric Respirators Effectiveness and Use
Elastomeric Respirators Effectiveness and Use Presented by Nicolas Smit Advocacy • https://twitter.com/ppetoheros • https://correcttheoversight.com/success-stories-news • https://www.northernontariobusiness.com/regional-news/sudbury/sudbury- engineer-urging-mining-industry-to-donate-respirators-2273156 • https://www.ola.org/en/legislative-business/committees/finance-economic- affairs/parliament-42/transcripts/committee-transcript-2020-jul-13#P547_134915 • https://www.sudbury.com/local-news/with-ongoing-n95-shortage-sudburian- advocating-for-donations-of-elastomeric-respirators-2910127 What are elastomeric respirators? • They are tight fitting respirators made of synthetic or natural rubber material, can be repeatedly used, disinfected, stored, and re-used. • They are equipped with replaceable filter cartridges or flexible, disc or pancake-style filters, which are not housed in a cartridge body. • They may also have sealing surfaces and adjustable straps that accommodate a better fit. • Elastomeric respirators have the same basic requirements for an OSHA-approved respiratory protection program as filtering facepiece respirators such as N95s, including medical evaluation, training, and fit testing. However, they have additional maintenance requirements which also include cleaning and disinfection of the face piece components such as straps, valves, and valve covers. Hierarchy of Controls for COVID-19 Prevention https://www.ccohs.ca/bestpractice/resources/1089-COVID-19---Hierarchy-of-Controls-(1).pdf N95 vs Half Face vs Full Face Different -

Respiratory Protection Program
Respiratory Protection Program Document History Version Date Comments 1 Dec. 2017 Replaced Respirator Policy with Respiratory Protection Program 1 Rev 12-2017 CONTENTS PURPOSE .................................................................................................................................................................. 4 SCOPE .............................................................................................................................................................. 4 POLICY STATEMENT ......................................................................................................................................... 4 PROCEDURES FOR RPP ENROLLMENT .............................................................................................................. 5 RESPONSIBILITIES ............................................................................................................................................. 5 4.1 Program Administrator ............................................................................................................................................................ 5 4.2 Supervisors/Principal Investigators (PIs) .................................................................................................................................. 6 4.3 Respirator Users/Employees .................................................................................................................................................... 6 PROGRAM ELEMENTS ..................................................................................................................................... -

SAS Safety & Compliance Catalog
When Protection Counts SAS Safety & Compliance Catalog SAS Safety Corp. | Tel (800) 262-0200 | Fax (800) 244-1938 | www.sassafety.com About SAS Safety Corp. Whether you’re a safety manager, business owner or DIY’er, SAS Safety Corp. provides quality safety products and equipment designed to make workplaces safer. As an ISO 9001 Certified company and over 30 years in the business, we are dedicated to protect our most valuable resource: people. Our Safety Products We offer a complete line of head-to-toe personal protective equipment; Respiratory, Hearing, Eye, Hand/Body Protection, Ergonomic/Traffic Safety, First-Aid Kits and Spill Control. We understand the importance of meeting customer’s needs from the distributor to the end-user. Commitment to your satisfaction is our #1 priority! Mission Statement Leadership Excellence SAS Safety Corp. is committed to providing its customers with quality products and services through continued improvement in technology, process and personnel. Being ISO certified is more than just a certificate; it is about maintaining a quality management system that assures valued customers that they can rely on SAS Safety products. Hand Protection 2-25 Respiratory Protection 26-46 Hi-Viz Protection 48 - 56 Eye Protection 58 - 73 Hearing Protection 74 - 76 Protective Wear 78 - 81 Head / Face Protection 82 - 83 First Aid 86 -87 Additional Products 84, 89 - 92 Charts Chemical Resistance Chart, Gloves .................................. 11 Lens Color Guide, Safety Eyewear ................................... 71 Hearing -

CDC/NIOSH-Approved Elastomeric Respirators with P100 Filters Brittany E. Howard, MD (Mayo Clinic, Phoenix, AZ) 1. Definition
CDC/NIOSH-Approved Elastomeric Respirators with P100 Filters Brittany E. Howard, MD (Mayo Clinic, Phoenix, AZ) 1. Definition Elastomeric Respirators 2. Reasons for Consideration of Elastomeric Respirators in High Risk Areas/Procedures 3. Safety/Certification 4. Cost and Disposables 5. Maintenance and Cleaning 6. Provider Fitting 7. Considerations with Surgical Use 1. Definition • Elastomeric Half-Mask Respirators are a reusable and washable rubber facemasks that in combination with reusable filters purifies a provider’s breathing air • These are used in healthcare and industrial settings.1 • The CDC has a list of all approved respirators of this type including versions by 3M and Drager https://www2a.cdc.gov/drds/cel/cel_results.asp?startrecord=1&Search=cel_form&max records=50&schedule=84A&producttype=aptype_2&contaminant=32&appdatefrom=& appdateto=&facepiecetype=Half+Mask&powered=no&scbatype=&scbause=&privatelab el 2. Reasons for Consideration of Elastomeric Respirators in High Risk Areas/Procedures: 1 https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/respsource1quest3.html#half • In the current pandemic of COVID-19, N95 masks are being used and promoted as one of the highest levels PPE for provider protection o However, an N95 only blocks at least 95 percent of very small (0.3 micron) test particles2 o It is the minimum respiratory protection approved for airborne protection from SARS by the CDC o Per CDC “A NIOSH-certified, disposable N95 respirator is sufficient for routine airborne isolation precautions. Use of a higher -

Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use (2019)
THE NATIONAL ACADEMIES PRESS This PDF is available at http://nap.edu/25275 SHARE Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use (2019) DETAILS 226 pages | 6 x 9 | PAPERBACK ISBN 978-0-309-48515-9 | DOI 10.17226/25275 CONTRIBUTORS GET THIS BOOK Linda Hawes Clever, Bonnie M. E. Rogers, Olivia C. Yost, and Catharyn T. Liverman, Editors; Committee on the Use of Elastomeric Respirators in Health Care; Board on Health Sciences Policy; Health and Medicine Division; National FIND RELATED TITLES Academies of Sciences, Engineering, and Medicine SUGGESTED CITATION National Academies of Sciences, Engineering, and Medicine 2019. Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use. Washington, DC: The National Academies Press. https://doi.org/10.17226/25275. Visit the National Academies Press at NAP.edu and login or register to get: – Access to free PDF downloads of thousands of scientific reports – 10% off the price of print titles – Email or social media notifications of new titles related to your interests – Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. (Request Permission) Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Copyright © National Academy of Sciences. All rights reserved. Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use Committee on the Use of Elastomeric Respirators in Health Care Linda Hawes Clever, Bonnie M. E. Rogers, Olivia C. Yost, and Catharyn T. Liverman, Editors Board on Health Sciences Policy Health and Medicine Division A Consensus Study Report of Copyright National Academy of Sciences. -

View the Safety and Practicality of Elastomeric Respirators for Protecting Themselves and Others from the Novel Coronavirus Or COVID-19
Chiang et al. International Journal of Emergency Medicine (2020) 13:39 International Journal of https://doi.org/10.1186/s12245-020-00296-8 Emergency Medicine PRACTICE INNOVATIONS IN EMERGENCY MEDICINE Open Access Elastomeric respirators are safer and more sustainable alternatives to disposable N95 masks during the coronavirus outbreak James Chiang1, Andrew Hanna1, David Lebowitz1,2 and Latha Ganti1,2* Abstract Background: In this paper, the authors review the safety and practicality of elastomeric respirators for protecting themselves and others from the novel coronavirus or COVID-19. They also describe the safe donning and doffing procedures for this protective gear. Main text: Due to the shortage of personal protective equipment (PPE), the CDC has recommended ways to conserve disposable N95 masks, including re-use and extended use, and reserving N95 masks for aerosol- generating procedures. However, these were never made to be re-used. Although the modes of transmission of COVID-19 are not fully understood, based on what we know about severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), droplets and aerosolized droplets contribute to the spread of this virus. More evidence from Wuhan, China, has demonstrated that COVID-19 viral particles are aerosolized and found in higher concentrations in rooms where PPE is being removed. Thus, it is best for all healthcare providers to have full aerosol protection. Conclusion: Given the shortage of PPE for aerosols, it is logical to utilize reusable elastomeric respirators with filter efficiency of 95% or higher. A single elastomeric respirator may replace hundreds to thousands of new disposable N95 masks. Background N95 masks for aerosol generating procedures, and using Since the coronavirus (2019-nCoV) or coronavirus dis- reusable elastomeric respirators with appropriate filters ease (COVID-19) outbreak, shortage of personal protect- [3]. -

REF-Respiratory-Protection-Plan
RESPIRATORY PROTECTION PLAN VBDEMS RESPIRATORY PROTECTION PLAN Contents 1 Purpose ..................................................................................................................................... 4 2 Plan administration .................................................................................................................. 5 3 Identifying airborne hazards requiring respirator use ........................................................ 7 3.1 Chemical Hazard Assessment ....................................................................................... 7 3.2 Biological Hazards ............................................................................................................ 7 4 Physical evaluations ................................................................................................................ 8 4.1 Volunteer personnel ......................................................................................................... 9 4.2 Career personnel .............................................................................................................. 9 5 Respirator selection ............................................................................................................... 10 5.1 Negative pressure respirators ...................................................................................... 10 5.2 Positive pressure respirators ........................................................................................ 10 5.3 Filters and cartridges .................................................................................................... -

Respiratory Protection Program
RESPIRATORY PROTECTION PROGRAM Introduction The provisions of the Respiratory Protection Program are per the requirements listed in the Federal Occupational Safety and Health Administration (OSHA) Standard 29 CFR 1910.134, as enforced at Western Kentucky University (WKU) by the Commonwealth of Kentucky Labor Cabinet. Scope The following program establishes guidelines for safe practice in the use of respiratory protective devices at WKU. “At WKU” includes maintenance, academic, or research functions preformed on WKU property or done by/for the purpose of representing WKU. This Respiratory Protection Program will address methods to protect WKU or eliminate inhalation hazards that are at or above the recommended safe exposure limits. WKU will use the hierarchy of hazard controls to minimize exposure levels before respiratory protection is used. This will include: elimination of hazard (ventilation), substitution of a non-hazardous or lesser hazardous substance, changing procedures, and training. Only in an emergency or during the time that engineering controls are being implemented, or the hazard cannot be eliminated will respiratory protection be used. This program applies to all use of respirators, voluntary or mandatory, regardless of frequency of use, reason for use, or duration of use. Respiratory Protection Devices Respirators are devices that protect against harmful chemicals, vapors, dusts, fumes, mists, smokes, or sprays. Some respirators provide air from a tank or an airline hose (atmosphere-supplying); others provide a filter, cartridges, or canisters to remove the contaminants in the air as you breathe in (air purifying). Respirators can also be classified as tight-fitting or loose-fitting. Some respirator facepieces are considered elastomeric meaning they are constructed from Natural or Synthetic Rubber and form a tight seal on the face. -

Personal Protective Equipment (PPE) Frequently Asked Questions (FAQ)
Personal Protective Equipment (PPE) Frequently Asked Questions (FAQ) v.9.2.2020 TABLE OF CONTENTS PURPOSE ................................................................................................................................................... 3 SPECIFIC PPE QUESTIONS ..................................................................................................................... 4 RESPIRATORS ....................................................................................................................................... 4 FACEMASKS .......................................................................................................................................... 6 FACE/EYE PROTECTION ..................................................................................................................... 6 HAND PROTECTION............................................................................................................................. 8 GOWNS ................................................................................................................................................... 8 GENERAL PPE QUESTIONS .................................................................................................................... 9 REQUIREMENT ..................................................................................................................................... 9 OBTAINING PPE ...................................................................................................................................