M Rith Bergstr M Isacsson
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plaggen Som Säger Mer Än Tusen Ord Lars Wallins Fashion Stories
No.08 HÖSTEN 2013 Inspiration från storbildsvärlden PÅ SPÅRET MED NY DEKOR Publikfavoriten i nya kläder NYA PERSPEKTIV I FILMVÄRLDEN Taken 2 tar oss till Istanbul ABBA THE MUSEUM Upplev legenden som fascinerar Plaggen som säger mer än tusen ord Lars Wallins Fashion Stories sjöj la un il g l f r n u e n d p å n s e t o r a s c No.08 HÖSTEN 2013 LEDAREN ...............................................................3 Några ord från big chief LITTLE BIG THINGS ...........................................4 Korta nedslag i storbildsvärlden TRONARVINGEN: INFINITUS JR ....................5 Printern som kan trycka på allt ABBA THE MUSEUM ........................................... 6 TÅLAMOD Om bandet som förändrade mer än musiken PÅ SPÅRET MED NY DEKOR ............................. 9 Tv-konceptet vi fortfarande älskar ÄR EN KONST UTOMHUSBILDER i går väl alla runt och bär på idéer av olika kreationer. På sidan 16 berättar han om hur allt UTÖVER DET VANLIGA ....................................10 V slag. Renoveringstankar för hemmet, sem- började, om kärleken till klädskapandet och hur Att synas i det offentliga rummet esterplaner, projekt att förverkliga i jobbet och fotografi blev en naturlig del i processen. så de där som liksom tar över helt och vägrar Här i Täby är vi precis klara med vår senaste AKUSTIK I DEN HÖGRE SKOLAN ..................12 lämna en förrän de har blivit testade. Varje dag uppfinning, printern Infinitus Jr. Tillskillnad Täby enskilda gymnasium satsar på ljudmiljön möter vi kunder som har just de stora idéerna, från sin större föregångare Infinitus, kan Jr och det finns inget bättre än att vara med att trycka på alla material, en idé som länge kändes EN BACKDROP TILL HÅKAN ......................... -

Mottagning I Stadshuset För Deltagare Och Arrangörer I Melo- Difestivalen 2006
Bilaga 4:8 till kommunstyrelsens protokoll den 22 februari 2006, § 19 PM 2006 RI (Dnr 007-247/2006) Mottagning i Stadshuset för deltagare och arrangörer i Melo- difestivalen 2006 Borgarrådsberedningen föreslår kommunstyrelsen besluta följande 1. En mottagning med buffé arrangeras i Stadshuset i samband med finalen i Melodifestivalen 2006. Mottagningen finansieras ur kommunstyrelsens repre- sentationsanslag. 2. Stadsledningskontoret får i uppdrag att se över regelverket för representation i Stadshuset och föreslå lämpliga förändringar till kommunstyrelsen. Föredragande borgarrådet Annika Billström anför följande. Bakgrund Melodifestivalturnéerna 2002-2005 har blivit stora framgångar, både på plats och i TV. En stor mängd människor har följt deltävlingarna på plats i städerna och drygt tre miljo- ner TV-tittare har följt varje deltävling under 2005. Den stora finalen i Globen i Stock- holm den 12 mars 2005 sågs av över fyra miljoner TV-tittare. År 2006 är Leksand, Karlstad, Karlskrona, Göteborg och slutligen inför finalen Stockholm officiella melodifestivalstäder. Vid varje delfinal är det vanligt att värdstaden inbjuder artister och arrangörer m. fl. till en mottagning. Stockholm Visitors Board har till kommunfullmäktiges presidium inkommit med förslag att staden inbjuder artister, arrangörer m. fl. till en buffémottagning i samband med 2006 års final av melodifestivalen som äger rum i Globen. Mottagningen beräknas för cirka 400 personer. Ärendets beredning Ärendet har beretts av stadsledningskontoret i samverkan med Stockholm Visitors Board. Mina synpunkter Att Stockholms stad återigen får möjligheten att vara värdstad för den stora finalen me- lodifestivalen är ett resultat av aktiva insatser från Stockholm Visitors Board. De vinster som arrangemanget ger staden i form av positiv marknadsföring och ökad besöksnäring har stor betydelse för stadens invånare, näringsliv och utveckling. -

Inte Bara Bögarnas Fest” En Queer Kulturstudie Av Melodifestivalen
”Inte bara bögarnas fest” En queer kulturstudie av Melodifestivalen Institutionen för etnologi, religionshistoria och genusvetenskap Examensarbete 30 HP Mastersprogrammet i genusvetenskap 120 HP Vårterminen 2018 Författare: Olle Jilkén Handledare: Kalle Berggren Abstract Uppsatsen undersöker hur TV-programmet Melodifestivalen förhåller sig till sin homokulturella status genom att studera programmets heteronormativa ramar och porträttering av queerhet. Det teoretiska ramverket grundar sig i representationsteori, kulturstudier, gaystudier och queerteori. Analysen resulterar i att de heteronormativa ramarna framställer heterosexualitet som en given norm i programmet. Detta uppvisas bland annat av en implicit heterosexuell manlig blick som sexualiserar kvinnokroppar och ser avklädda män, queerhet och femininitet som något komiskt. Detta komplicerar tidigare studiers bild av melodifestivaler som huvudsakligen investerade och accepterande av queera subjekt. Den queera representationen består främst av homosexuella män. Den homosexuellt manliga identiteten görs inte enhetlig och bryter mot heteronormativa ideal i olika grad. Några sätt som den homosexuellt manliga identiteten porträtteras är artificiell, feminin, icke-monogam, barnslig och investerad i schlager. Analysen påpekar att programmet har queert innehåll trots dess kommersiella framställning och normativa ideal. Nyckelord: Melodifestivalen, schlager, genusvetenskap, homokultur, gaystudier, bögkultur, heteronormativitet. Innehållsförteckning 1. En älskad och hatad ”homofilfestival” 1 -

Det Händer På Södra Teatern Den 18 - 31 Oktober
Det händer på Södra Teatern den 18 - 31 oktober Gripande popmusik blir det när Rebekka Karijord kommer till Kägelbanan den 19 oktober, med färska albumet ”We become ourselves” i bagaget. Samma kväll bjuder El Tunche Soundystem – Dj Mateo, Kuto Selektah Quilla och El Pilas – på bastunga rytmer från Sydamerika i Södra Bar. Den 20 oktober gör Club Barracuda, Mosquito och Outernational gemensam sak för en helkväll med musik från städer som Miami, Kingston och Dakar. I Etablissemanget och i Södra Bar med öppet till 03.00! Den 24 oktober är det dags för Klezmatics att ge sin skickligt snidade klezmermusik på Stora Scenen. Den ekonomiska krisen i Europa och EMU står i fokus i Stefan de Vylders nya bok Eurokrisen. Den uppmärksammas med samtal med Kajsa Ekis Ekman och releasefest på Kägelbanan, den 25 oktober. Starka rytmer från södra Iran ger Shanbehzadeh när de uppträder på Stora Scenen den 26 oktober. Stark musik i det mörkare och mer orgeldrivna registret bjuder Anna von Hausswolff på då hon spelar på Kägelbanan samma kväll. En av Sveriges mest produktiva och lekfulla rappare, Organismen, gästar eminenta hiphopklubben Yes! den 27 oktober. Pjäsen ”Cabares Cabarei” är en berättelse om den absurda människan i den postmoderna världen, skriven av den Sarajevofödde regissören och skådespelaren Zijah Sokolovic. På Stora Scenen den 28 oktober. Andrius Mamontovas är en av Litauens främsta rockartister, det kommer han att visa på Kägelbanan den 28 oktober. ”Made in India” är en interaktiv föreställning om babyindustrin i Indien, skriven av sociologen och skådespelaren Amrita Pande. På Stora Scen den 30 oktober. Kvällen därpå, den 31 oktober, kommer Love Antell till Södra Teatern för att leverera sina träffsäkra Stockholmsskildringar. -

ARTISTER 2014 JONAS HEDQVIST Under Mer Än Tio Års Tid Har Jonas Hedqvist Befäst Sin Ställning Som Scenestradör
ARTISTER 2014 JONAS HEDQVIST Under mer än tio års tid har Jonas Hedqvist befäst sin ställning som scenestradör. Från starten 2001 med “I Am What I Am”, den första officiella låten för Stockholm Pride via flera singlar som alla nått de svenska listorna, med en Top 3 på singellistan och en Top 5 på Sverige Topp 40 som bäst, har Jonas mött och behållit en publik. I Malmö har han etablerat sig som underhållare genom upprepade framgångar med Allsång i Parken som blivit en succé i Malmö Folkets Park. Addera till allt detta otaliga turnéer och konserter, i Sverige och utomlands, själv och tillsammans med andra pop- och schlagerstjärnor så framträder en klar och tydlig bild av entertainer av högsta klass. ALvaro EstreLLA Med sitt fantastiska framförande, i Melodifestivalen, av låten Bedroom blev Alvaro Estrella snabbt en förhandsfavorit och av genrepspubliken en tippad vinnare! Även om han därefter inte röstades vidare till final så går hans popularitet inte att missuppfattas. Bedroom gick rakt in på iTunes förstaplats! Alvaro Estrella har utvecklat en känsla som kräver åratal av träning och förfinat sitt artisteri till en rak- bladsvass spets. Han har jobbat i underhållningsbranschen i mer än ett decennium och är redan ett bekant ansikte för svenska folket. Alvaro har sjungit bakom både Eric Saade och Danny Saucedo men även till- sammans med Farid Mammadow, Azerbajdzjans bidrag i Eurovision. Han har även dansat bakom Darin, Agnes och världsartisten Ricky Martin under MTV European Music Awards. MATHIAS HOLMGREN Mathias gjorde sitt genombrott i Fame Factory 2002. Han har setts som sångare i Barbados, medverkat i Melodifestivalen, deltagit i Så ska det låta, Doobidoo, Fångarna på fortet, Gokväll, gjort en omfattande julturné med Åsa Jinder, samarbetat med Carola Häggkvist och Staffan Hellstrand på skiva och mycket mera. -

SVT:S Öppet Arkiv 2015 Sida 1 Av
SVT:s Öppet arkiv 2015 ID-nr Programnamn Episodnamn Utbud 1370140-1 401 Prod Year 1970 Drama 1356320-1 10 ÅR MED CAROLA Prod Year 1993 Artistshow 1357554-1 1000 ÅR PÅ 2 TIMMAR Episod 1 Humaniora 1357554-2 1000 ÅR PÅ 2 TIMMAR Episod 2 Humaniora 1361824-24 20:00 1985-1986 Episod 24: Special - Stina möter Silvia Politik, samhälle 1358953-1 21 - MED ESS I LEKEN Prod Year 1977 Blandat nöje 1358955-1 21 - MED ESS I LEKEN Prod Year 1979 Blandat nöje 1367093-42 24 MINUTER 2003 Episod 42: Timbuktu Blandat nöje 1367093-78 24 MINUTER 2003 Episod 78: Leif GW Persson Blandat nöje 1367093-0 24 minuter 2003 1359448-1 24-TIMMARS, EN ANNORLUNDA REGATTA Prod Year 1975 Idrottstävling 1357538-1 300 ÅR AV ÖGONBLICK Episod 1 Politik, samhälle 1357538-2 300 ÅR AV ÖGONBLICK Episod 2 Politik, samhälle 1357538-3 300 ÅR AV ÖGONBLICK Episod 3 Politik, samhälle 1358773-1 7 TILL 9 Episod 1 Blandat nöje 1358773-5 7 TILL 9 Episod 5 Blandat nöje 1358773-6 7 TILL 9 Episod 6 Blandat nöje 1366976-1 900 SEK Episod 1 Blandat nöje 1366976-2 900 SEK Episod 2 Blandat nöje 1366976-3 900 SEK Episod 3 Blandat nöje 1366976-4 900 SEK Episod 4 Blandat nöje 1366976-5 900 SEK Episod 5 Blandat nöje 1366976-6 900 SEK Episod 6 Blandat nöje 1366976-7 900 SEK Episod 7 Blandat nöje 1366976-8 900 SEK Episod 8 Blandat nöje 1366976-9 900 SEK Episod 9 Blandat nöje 1365430-1 A FÖR AGNETHA Prod Year 1985 Musik 1169205-1 AB DUN OCH BOLSTER Prod Year 1988 Drama 1367022-1 ABSOLUT SAMTAL Episod 1 Kulturgestaltning 1367022-2 ABSOLUT SAMTAL Episod 2 Kulturgestaltning 1367022-3 ABSOLUT SAMTAL Episod 3 -
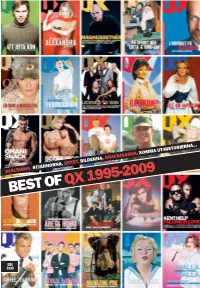
Best of Qx 1995-2009
HJÄLTARNA. STJÄRNORNA. SEXET. BILDERNA. SNACKISARNA. KOMMA UT-HISTORIERNA... BEST OF QX 1995-2009 DEC 2009 VEMTYCKER DUSKAFÅPRIS PÅGAYGALAN 2010? VEM ÄR ÅRETS HOMO? VEM ÄR ÅRETS HETERO? VILKET ÄR ÅRTES GAYSTÄLLE? VILKA ÄR ÅRETS DUO? VILKEN ÄR ÅRETS LÅT? VILKEN ÄR ÅRETS FILM? Nominera dina favoriter på www.qx.se fram till och med den 10 december. Gaygalan hålls på Cirkus i Stockholm måndagen den 1 februari 2010. Dörrarna öppnas 18.00. Show 21.00. Biljetterna släpps torsdag den 17 december på ticnet.se. Galakonferencier: Petra Mede QX <:?6D:D<E ?J£C A6CD:D<E ?J£C 42D:?@ E@FC 3CF?49 =2 G682D =25:6D 42D:?@ ?:89E =6E|D>656=92GDE6>2 86E G2=6?E:?6 >2CC:65 3CF?49 3C2DD6C:6E E6>2<G¢==2C E;6; <G¢== A@<6C EFC?6C:?82C >2C<FD 2F;2=2J 9¢>E25:EEAC@8C2>A£<2D:?@E6==6C36D´<HHH42D:?@4@D>@A@=D6 DE@4<9@=>8´E63@C8>2=>´DF?5DG2== HHH42D:?@4@D>@A@=D6 INNEHÅLL INGÅNG Det här är det sista numret av QX. daktionen satt och skrev in. Vi tog sedan Idag finns det säkert 100 mer eller Och det bästa. hand om alla svarsbrev som folk skrev mindre kända svenskar som är öppet H, Nej, så allvarligt är det inte, men an- och postade dem vidare till rätt avsändare. B eller T. ledningen till att vi gjort ett ”Best of ” i Ibland blev det ofrivilligt roligt när man Fantastiskt. det här numret är att QX i och med nästa läste annonserna i tidningen, i en annons Utan öppna homosar skulle QX ald- FOTO: LOUISE BILLGERT nummer byter format och design. -

Carola Vinner Melodifestivalen 2006 - Vinsterna Utbetalas Omedelbart
2006-03-14 15:09 CET Vi ger upp! Carola vinner Melodifestivalen 2006 - vinsterna utbetalas omedelbart Ladbrokes stänger spelet och betalar ut Carola som vinnare redan nu. Pengarna är på väg ut till Sveriges alla schlagerspelare. Ladbrokes tvingas att göra detta för att stoppa ytterligare förluster på spelet. Vi har tagit emot en enorm ström av pengar enbart på Carola, och vi ser oss tvingade att vidta denna åtgärd för att skydda Ladbrokes, säger Douglas Roos, Ladbrokes VD i Norden, i en kommentar. Från och med idag är det möjligt att spela på vem som tar andra plats i Melodifestivalen. Alexander Bard/BWO, trots elitistiska angrepp på nationalhjältinnan, har favoritoddset 2,25 för en charmig andra plats i Melodifestivalen 2006. Carola ger 7 gånger pengarna för vinst i Eurovision Song Contest i maj i Aten. Vem kommer två i Melodifestivalen den 18 mars 2006? BWO - Temple Of Love 2,25 Andreas Johnson - Sing For Me 3,25 Linda Bengtzing - Jag ljuger så bra 6 The Poodles - Night Of Passion 8 Magnus Backlund - The Name Of Love 15 Rednex - Mama Take Me Home 15 Bjorn Kjellman - Älskar du livet 15 Magnus Carlsson - Lev Livet 26 Kikki Danielsson - Idag & imorgon 34 För mer information: Douglas Roos, VD Ladbrokes Norden, +46-8-407 64 43, +46-70-735 21 25, [email protected] Ladbrokes grundades 1886 och är ett världsledande spelföretag med 2583 vadslagningsbutiker och 14,000 anställda. Ladbrokes.com har 2 miljoner registrerade kunder från 200 länder och säljer speltjänster på 12 språk. Ladbrokes grundades 1886 och är ett världsledande spelföretag med med närmare 3000 vadslagningsbutiker i Storbritannien, Irland, Belgien och Spanien. -

Julkonsert I Sparbanken Lidköping Arena: Måns Zelmerlöws ”Christmas with Friends”
2012-09-17 10:37 CEST Julkonsert i Sparbanken Lidköping Arena: Måns Zelmerlöws ”Christmas with Friends” Sedan dörrarna till Sparbanken Lidköping Arena öppnades för första gången, har vi varit bortskämda med att varje säsong ha minst en riktigt bra julshow i Arenan. Så var det år 2010 då ”Dansdax” med Jill Johnson m.fl. intog Arenans stora scen och både bjöd på show så väl som dans, med Kindbergs och Perikles, in på småtimmarna. Året efter underhöll ”The Blues Mothers ” med La Gaylia Frazier och Anna Sahlene medan Arvingarna svarade för Dansmusiken. Bägge åren gästades Arenan också av Familjens Julkalas med artister som Erik Saade, Darin och Timoteij m.fl. Det är därför med stor glädje som vi kan presentera årets Julevenemang i form av en Julkonsert, med en av Sveriges, för närvarande, bredaste och mest folkkära artister Måns Zelmerlöw. Måns har trots sin relativa ungdom, han är född 13/6 1986, hunnit med mer än de flesta artister kanske hinner med under en hel artistkarriär. Han har bland annat medverkat i Idol (År 2005), där han fick sitt genombrott, samt Melodifestivalen (2007 med Cara Mia och 2009 med Hope & Glory) och Så skall det låta (2009). Han har dessutom varit programledare för program som Lilla Melodifestivalen (År 2007), Sommarkrysset (2009), Melodifestivalen (År 2010) samt Allsång på Skansen (2011-). Dessutom vann han Let's Dance 2006 tillsammans med Maria Bild. Måns har vidare en stor erfarenhet av att framträda på Musikalscener runt om i landet. Han bland annat har spelat huvudrollerna som Danny Zuko i musikalen Grease samt Romeo i Romeo och Julia. -

Veckans Kändis
VECKANS KÄNDIS MÅNS ZELMERLÖW Måns Petter Albert Sahlén Zelmerlöw föddes den 13 juni 1986 i Lund. Han är en svensk programledare, låtskrivare och artist. Som artist har han deltagit i program som Idol, Let's dance, Så ska det låta, Melodifestivalen och Eurovision Songcontest. Han deltog även i Diggilooturnén med andra svenska artister. Han har varit programledare för bland annat Sommarkrysset, Melodifestivalen och Allsång på Skansen. År 2005 tävlade han i TV4.s Idol där han slutade på en femte plats. Året efter deltog han i Let's dance och vann tillsammans med Maria Bild. År 2006 spelade han även huvudrollen, Danny Zuko, i musikalen Grease som framfördes i Malmö. År 2007 deltog han i Melodifestivalen för första gången och gick till final med låten Cara Mia. Han slutade på tredje plats med näst flest röster från tittarna. Låten blev mycket populär och vann sedan Second Chance Contest och National Finals Song Contest. Den låg även etta på den svenska försäljningslistan. Samma år var han även programledare för lilla Melodifestivalen. År 2009 deltog han i Meloidifestivalen för andra gången med låten Hope and Glory. Han tog sig direkt till final i Globen och hamnade på en fjärde plats med 144 poäng. Under samma år uppträdde han på kronprinsessan Victorias födelsedag som sändes den 14 juni i Sveriges Television. Den 10 november utsågs han till en av de tre programledarna för Melodifestivalen 2010. Han ledde programmet tillsammans med Dolph Lundgren och Christine Meltzer. Den 23 februari 2011 var det klart att Måns skulle leda Allsång på Skansen. Under tre år var han programledare för Allsång på Skansen men valde sedan att avgå, därefter tog Petra Marklund över rollen. -

Adam Lambert Flator Som Surfar Hur Går Det I Oslo? 19 Frågor Till Jessica Andersson 10 Tips Inför Hbt-Gbg Sia Köket & En Bög Ricky Martin Botox Paris
maj 2010 #174 eddie &rabih har nåt ihop eddie om Rebound, idol, uppväxten & det där andra... adam lambert flator som surfar hur går det i oslo? 19 frågor till jessica andersson 10 tips inför hbt-gbg sia köket & en bög ricky martin botox PAris OMSLAG.indd 1 2010-04-22 11.06 Jumbojet nonstop till Fritidsresors Thailand. I vinter kan du fl yga Jumbojet med oss till Phuket och Bangkok. Vi erbjuder Sveriges billigaste fl ygstol och har ett Thailand för både debutanter och proffs. Välj mellan allt från populära favoriter på Phuket, unika hotell med personlighet och nya Blue Village Exotic på Koh Samet i Siambukten. Säkra vinterns drömsemester redan idag. Flygstol t/r Thailand 1 *v fr. 5 998:– LÄS MER OCH BOKA PÅ FRITIDSRESOR.SE Boka på Fritidsresor.se eller ring 0771-84 01 00. Besök din närmaste resebyrå. * Pris per person för fl yg tur och retur Arlanda – Bangkok, 1 vecka med avresa 7/3 2011. Arlanda – Phuket 1 v med avresa 4/3 2011 6 498:-. Begränsat antal platser. Omslagsannonser + glossad inlaga maj10.indd 6 2010-04-22 10.13 www.dragster.se | Foto: | Foto: www.dragster.se DDR GBG workshop på röhsska 12–16 maj Under HBT-festivalen i Göteborg är det premiär för Stitch – Årets skönaste nyhet som inte bara är en snygg lampa utan ett helt DIY-koncept. Stitch HBT-Edition kostar 895 kr, och då ingår ett startkit med stoppnål och garn i regnbågens alla färger. Under hela festivalen har vi en broderiworkshop på Röhsska där du kan prova på att designa en lampa. -

Facts About Stockholm's Tourism Industry
Facts about Stockholm’s tourism industry Statistics for 2008 – August 2009 Contents Stockholm – The Capital of Scandinavia .......................... 4 Stockholm in perspective ..........7 Stockholm’s international position......8 Stockholm’s position in Sweden ......10 Visitors to Stockholm...............13 Where visitors come from...............14 How visitors get to Stockholm..........16 Where visitors stay. .......................18 Commercial accommodation...........22 Leisure travel and business travel .....28 International meetings/conventions. 30 Visitor destinations in Stockholm ...32 Events in Stockholm ......................34 Stockholm on the water................35 How long visitors stay......... ...........36 What visitors spend.......................37 Economy and employment .... 39 Stockholm Visitors Board ....... 44 About the statistics .................. 46 Facts about Stockholm’s tourism industry Stockholm continues to retain its position as ”The Capital of Scandinavia” and the engine of the Swedish tourist industry. Over the last ten years the number of guest nights in Stockholm has risen by 40 percent. 2008 saw a new peak of 9.6 million guest nights. And the first eight months of 2009 continue to show strong growth for Stockholm, especially in the leisure travel segment, which grew by 11 percent over the same period in 2008. This trend is clearly superior to that seen by other Scandinavian capitals. Success breeds success as is well known, but this doesn’t mean that we can rest on our laurels. In cooperation with the LFV (the Swedish Civil Aviation Administration), we are continuing our efforts to preserve and expand the number of international airlines coming to Stockholm. 2010 promises to be an extremely exciting year for Stockholm. It’s certainly not every year that we simultaneously experience the wedding of a crown princess, a big year for conventions, new attractions, new hotels and the honor of being Europe’s first environmental capital.