NPS Clinical Update – Synthetic Cannabinoids and Synthetic Stimulants July 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recommended Methods for the Identification and Analysis of Synthetic Cathinones in Seized Materialsd
Recommended methods for the Identification and Analysis of Synthetic Cathinones in Seized Materials (Revised and updated) MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Photo credits:UNODC Photo Library; UNODC/Ioulia Kondratovitch; Alessandro Scotti. Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Synthetic Cathinones in Seized Materials (Revised and updated) MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2020 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/49/REV.1 Original language: English © United Nations, March 2020. All rights reserved, worldwide. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. -
Moves to Amend HF No. 2128 As Follows: Delete Everything After
04/05/21 10:32 am HOUSE RESEARCH RC/MV H2128DE1 1.1 .................... moves to amend H.F. No. 2128 as follows: 1.2 Delete everything after the enacting clause and insert: 1.3 "ARTICLE 1 1.4 DHS HEALTH CARE PROGRAMS 1.5 Section 1. [62A.002] APPLICABILITY OF CHAPTER. 1.6 Any benefit or coverage mandate included in this chapter does not apply to managed 1.7 care plans or county-based purchasing plans when the plan is providing coverage to state 1.8 public health care program enrollees under chapter 256B or 256L. 1.9 Sec. 2. Minnesota Statutes 2020, section 62C.01, is amended by adding a subdivision to 1.10 read: 1.11 Subd. 4. Applicability. Any benefit or coverage mandate included in this chapter does 1.12 not apply to managed care plans or county-based purchasing plans when the plan is providing 1.13 coverage to state public health care program enrollees under chapter 256B or 256L. 1.14 Sec. 3. Minnesota Statutes 2020, section 62D.01, is amended by adding a subdivision to 1.15 read: 1.16 Subd. 3. Applicability. Any benefit or coverage mandate included in this chapter does 1.17 not apply to managed care plans or county-based purchasing plans when the plan is providing 1.18 coverage to state public health care program enrollees under chapter 256B or 256L. 1.19 Sec. 4. [62J.011] APPLICABILITY OF CHAPTER. 1.20 Any benefit or coverage mandate included in this chapter does not apply to managed 1.21 care plans or county-based purchasing plans when the plan is providing coverage to state 1.22 public health care program enrollees under chapter 256B or 256L. Article 1 Sec. -

Fragmentation Pathways of Odd- and Even-Electron N-Alkylated Synthetic Cathinones
International Journal of Mass Spectrometry 453 (2020) 116354 Contents lists available at ScienceDirect International Journal of Mass Spectrometry journal homepage: www.elsevier.com/locate/ijms Fragmentation pathways of odd- and even-electron N-alkylated synthetic cathinones * J. Tyler Davidson, PhD a, Zachary J. Sasiene, BS b, Glen P. Jackson, Ph.D. a, b, a Department of Forensic and Investigative Science, West Virginia University, Morgantown, WV, 26506-6121, USA b C. Eugene Bennett Department of Chemistry, West Virginia University, Morgantown, WV, 26506-6121, USA article info abstract Article history: Three ionization techniques, isotopic labeling, high-resolution mass spectrometry (HRMS) and multi- Received 19 March 2020 stage mass spectrometry (MSn) were used to analyze a series of N-alkylated synthetic cathinone de- Received in revised form rivatives and gain a deeper understanding of their fragmentation behavior during mass spectrometric 17 April 2020 analysis. The compounds analyzed represent 15 unique structures with common substitutions to the core Accepted 18 April 2020 synthetic cathinone structure, including substitutions to the aromatic ring and the number and types of Available online 23 April 2020 N-alkyl functionalities. The analytical techniques employed include gas chromatography-electron ioni- zation-mass spectrometry (GC-EI-MS), electrospray ionization-tandem mass spectrometry (ESI-MS/MS) with HRMS and direct analysis in real time tandem mass spectrometry (DART-MS/MS) with HRMS. These techniques cover a variety of forensic applications, including seized drug analysis, toxicological analysis and screening analysis, in local, state and federal laboratories. For collision-induced dissociation (CID) of protonated precursors, the spectra of 2 and 3 amines showed evidence for charge-remote and charge- directed fragmentation mechanisms. -

Application of High Resolution Mass Spectrometry for the Screening and Confirmation of Novel Psychoactive Substances Joshua Zolton Seither [email protected]
Florida International University FIU Digital Commons FIU Electronic Theses and Dissertations University Graduate School 4-25-2018 Application of High Resolution Mass Spectrometry for the Screening and Confirmation of Novel Psychoactive Substances Joshua Zolton Seither [email protected] DOI: 10.25148/etd.FIDC006565 Follow this and additional works at: https://digitalcommons.fiu.edu/etd Part of the Chemistry Commons Recommended Citation Seither, Joshua Zolton, "Application of High Resolution Mass Spectrometry for the Screening and Confirmation of Novel Psychoactive Substances" (2018). FIU Electronic Theses and Dissertations. 3823. https://digitalcommons.fiu.edu/etd/3823 This work is brought to you for free and open access by the University Graduate School at FIU Digital Commons. It has been accepted for inclusion in FIU Electronic Theses and Dissertations by an authorized administrator of FIU Digital Commons. For more information, please contact [email protected]. FLORIDA INTERNATIONAL UNIVERSITY Miami, Florida APPLICATION OF HIGH RESOLUTION MASS SPECTROMETRY FOR THE SCREENING AND CONFIRMATION OF NOVEL PSYCHOACTIVE SUBSTANCES A dissertation submitted in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in CHEMISTRY by Joshua Zolton Seither 2018 To: Dean Michael R. Heithaus College of Arts, Sciences and Education This dissertation, written by Joshua Zolton Seither, and entitled Application of High- Resolution Mass Spectrometry for the Screening and Confirmation of Novel Psychoactive Substances, having been approved in respect to style and intellectual content, is referred to you for judgment. We have read this dissertation and recommend that it be approved. _______________________________________ Piero Gardinali _______________________________________ Bruce McCord _______________________________________ DeEtta Mills _______________________________________ Stanislaw Wnuk _______________________________________ Anthony DeCaprio, Major Professor Date of Defense: April 25, 2018 The dissertation of Joshua Zolton Seither is approved. -

Written Witness Statement for U.S. Sentencing Commission's Public
STATEMENT OF TERRENCE L. BOOS, PH.D. SECTION CHIEF DRUG AND CHEMICAL EVALUATION SECTION DIVERSION CONTROL DIVISION DRUG ENFORCEMENT ADMINISTRATION and CASSANDRA PRIOLEAU, PH.D. DRUG SCIENCE SPECIALIST DRUG AND CHEMICAL EVALUATION SECTION DIVERSION CONTROL DIVISION DRUG ENFORCEMENT ADMINISTRATION - - - BEFORE THE UNITED STATES SENTENCING COMMISSION - - - HEARING ON SENTENCING POLICY FOR SYNTHETIC DRUGS - - - OCTOBER 4, 2017 WASHINGTON, D.C. 1 Introduction New Psychoactive Substances (NPS) are substances trafficked as alternatives to well- studied controlled substances of abuse. NPS have demonstrated adverse health effects such as paranoia, psychosis, and seizures to name a few. Cathinones, cannabinoids, and fentanyl-related substances are the most common NPS drug classes encountered on the illicit drug market, all with negative consequences for the user to include serious injury and death. Our early experience saw substances being introduced from past research efforts in an attempt to evade controls. This has evolved to NPS manufacturers structurally altering substances at a rapid pace with unknown outcomes to targeting specific user populations. These substances represent an unprecedented level of diversity and consequences. Due to clandestine manufacture and unscrupulous trafficking, the user is at great risk. A misconception exists that these substances carry a lower risk of harm In reality, published reports from law enforcement, emergency room physicians and scientists, accompanied with autopsies from medical examiners, have clearly demonstrated the harmful and potentially deadly consequences of using synthetic cathinones. These substances are introduced in an attempt to circumvent drug controls and the recent flood of NPS remains a challenge for law enforcement and public health. The United Nations Office on Drugs and Crime reported over 700 NPS encountered.1 The manufacturers and traffickers make minor changes in the chemical structure of known substances of abuse and maintain the pharmacological effect. -
Model Scheduling New/Novel Psychoactive Substances Act (Third Edition)
Model Scheduling New/Novel Psychoactive Substances Act (Third Edition) July 1, 2019. This project was supported by Grant No. G1799ONDCP03A, awarded by the Office of National Drug Control Policy. Points of view or opinions in this document are those of the author and do not necessarily represent the official position or policies of the Office of National Drug Control Policy or the United States Government. © 2019 NATIONAL ALLIANCE FOR MODEL STATE DRUG LAWS. This document may be reproduced for non-commercial purposes with full attribution to the National Alliance for Model State Drug Laws. Please contact NAMSDL at [email protected] or (703) 229-4954 with any questions about the Model Language. This document is intended for educational purposes only and does not constitute legal advice or opinion. Headquarters Office: NATIONAL ALLIANCE FOR MODEL STATE DRUG 1 LAWS, 1335 North Front Street, First Floor, Harrisburg, PA, 17102-2629. Model Scheduling New/Novel Psychoactive Substances Act (Third Edition)1 Table of Contents 3 Policy Statement and Background 5 Highlights 6 Section I – Short Title 6 Section II – Purpose 6 Section III – Synthetic Cannabinoids 13 Section IV – Substituted Cathinones 19 Section V – Substituted Phenethylamines 23 Section VI – N-benzyl Phenethylamine Compounds 25 Section VII – Substituted Tryptamines 28 Section VIII – Substituted Phenylcyclohexylamines 30 Section IX – Fentanyl Derivatives 39 Section X – Unclassified NPS 43 Appendix 1 Second edition published in September 2018; first edition published in 2014. Content in red bold first added in third edition. © 2019 NATIONAL ALLIANCE FOR MODEL STATE DRUG LAWS. This document may be reproduced for non-commercial purposes with full attribution to the National Alliance for Model State Drug Laws. -
Case: 1:18-Cr-00474-JRA; Zheng ECF Filed Indictment
Case: 1:18-cr-00474-JRA Doc #: 1 Filed: 08/17/18 1 of 83. PageID #: 1 IN THE UNITED STATES DISTRICT COURT FOR THE NORTHERN DISTRICT OF OHIO EASTERN DIVISION UNITED STATES OF AMERICA, ) INDICTMENT Plaintiff, ~ JUDGE PO V. ~ CASE10; 18 CR ) Title 21, Sections 33l(a), FUJINO ZHENG, ) 333(b)(7), 35l(d), 841(a)(l), aka, GORDON JIN, ) (a)(2), (b)(l)(A), (b)(l)(C), (h), aka, MR. JIN, ) 843(c)(2)(A), 846, 848, 853, aka, GORDON ZHENG, ) 952(a), 959(a), 960(a)(l) and (3), aka, JINXINXIN, ) (b)(1 ), (b )(3), 963, and 970, aka, FU JING ZHENG, ) Title 18, Sections 1956(a)(2), (h), aka, DENG GAO, ) and 2, GUANGHUA ZHENG, ) United States Code aka, GUANG HUA ZHENG, ) ) Defendants. ) ) COUNT 1 (Conspiracy to Manufacture, Distribute, and Possess with the Intent to Distribute Controlled Substances and Controlled Substance Analogues Resulting in Death, 21 U.S.C. §§ 841(a)(l), (b)(l)(A), (b)(l)(C), all in violation of 21 U.S.C. § 846) The Grand Jury charges: 1. From on or about January 1, 2008 to the Present, the exact dates unknown to the Grand Jury, in the Northern District of Ohio, Eastern Division, the People's Republic of China, and elsewhere, Defendants FUJINO ZHENG, aka GORDON JIN, aka MR. JIN, aka GORDON ZHENG, aka JINXINXIN, aka FU JING ZHENG, aka DENG GAO; GUANGHUA ZHENG, aka GUANG HUA ZHENG; Guangfu Z.; Guifeng C.; Songyan J.; Longbao Z.; Qinghua Y., aka Jason Yen; Lynn X.; Leroy S.; (individuals whose names are known to the Grand Jury); Global United Biotechnology; Global United Holdings; Global Biotech, Inc.; Global Holdings, Inc.; Top Lab RC; Global RC; Golden Chemicals; Cambridge Chemicals; Wonda Science; OneChem; Case: 1:18-cr-00474-JRA Doc #: 1 Filed: 08/17/18 2 of 83. -
Forensic Toxicology Scope of Testing and Detection Limits
J. RYAN MCMAHON II County Executive INDU GUPTA, MD, MPH MEDICAL EXAMINER’S OFFICE Commissioner of Health FORENSIC TOXICOLOGY LABORATORY CAROLYN H. REVERCOMB, MD, DABP ONONDAGA COUNTY HEALTH DEPARTMENT Chief Medical Examiner KRISTIE BARBA, MS, D-ABFT-FT CENTER FOR FORENSIC SCIENCES Toxicologist Forensic Toxicology Scope of Testing and Detection Limits Table of Contents QUALITATIVE ANALYSES.........................................................................................................2 Volatile Screen by GC/FID .............................................................................................................2 Carbon Monoxide by Microdiffusion..............................................................................................2 Carbon Monoxide by CO-Oximeter ................................................................................................2 Ethylene Glycol by GC/MS.............................................................................................................2 ELISA Buprenorphine by IA for Blood/Urine ................................................................................2 ELISA by IA for Blood ...................................................................................................................3 ELISA by IA for Urine....................................................................................................................4 Gamma Hydroxybutyrate (GHB) by GC/MS..................................................................................5 Gabapentin, -
Model Scheduling New Novel Psychoactive Substances
Model Scheduling New/Novel Psychoactive Substances Act September 2018 (original version published in 2014). This project was supported by Grant No. G1799ONDCP03A, awarded by the Office of National Drug Control Policy. Points of view or opinions in this document are those of the author and do not necessarily represent the official position or policies of the Office of National Drug Control Policy or the United States Government. © 2018. NATIONAL ALLIANCE FOR MODEL STATE DRUG LAWS. This document may be reproduced for non- commercial purposes with full attribution to the National Alliance for Model State Drug Laws. Please contact Jon Woodruff at [email protected] or (703) 836-7496 with any questions about the Model Language. This document is intended for educational purposes only and does not constitute legal advice or opinion. Headquarters Office: THE NATIONAL ALLIANCE 1 FOR MODEL STATE DRUG LAWS, 1335 North Front Street, First Floor, Harrisburg, PA, 17102-2629. Model Scheduling New/Novel Psychoactive Substances Act Table of Contents 3 Policy Statement and Background 5 Highlights 6 Section I – Short Title 6 Section II – Purpose 6 Section III – Synthetic Cannabinoids 12 Section IV – Substituted Cathinones 18 Section V – Substituted Phenethylamines 22 Section VI – N-benzyl Phenethylamine Compounds 24 Section VII – Substituted Tryptamines 27 Section VIII – Substituted Phenylcyclohexylamines 28 Section IX – Fentanyl Derivatives 37 Section X – Unclassified NPS © 2018. NATIONAL ALLIANCE FOR MODEL STATE DRUG LAWS. This document may be reproduced for non- commercial purposes with full attribution to the National Alliance for Model State Drug Laws. Please contact Jon Woodruff at [email protected] or (703) 836-7496 with any questions about the Model Language. -
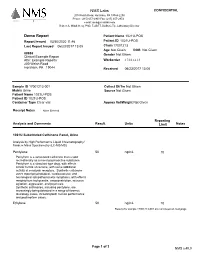
Example Report Attn: Example Reports Workorder 17001213 200 Welsh Road Horsham, PA 19044 Received 06/23/2017 13:00
NMS Labs CONFIDENTIAL 200 Welsh Road, Horsham, PA 19044-2208 Phone: (215) 657-4900 Fax: (215) 657-2972 e-mail: [email protected] Robert A. Middleberg, PhD, F-ABFT, DABCC-TC, Laboratory Director Demo Report Patient Name 1021U-POS Report Issued 03/30/2020 11:46 Patient ID 1021U-POS Last Report Issued 06/23/2017 13:05 Chain 17001213 Age Not Given DOB Not Given 88888 Gender Not Given Clinical Example Report Attn: Example Reports Workorder 17001213 200 Welsh Road Horsham, PA 19044 Received 06/23/2017 13:00 Sample ID 17001213-001 Collect Dt/Tm Not Given Matrix Urine Source Not Given Patient Name 1021U-POS Patient ID 1021U-POS Container Type Clear vial Approx Vol/Weight Not Given Receipt Notes None Entered Reporting Analysis and Comments Result Units Limit Notes 1021U Substituted Cathinone Panel, Urine Analysis by High Performance Liquid Chromatography/ Tandem Mass Spectrometry (LC-MS/MS) Pentylone 50 ng/mL 10 Pentylone is a substituted cathinone that is sold recreationally as a novel psychoactive substance. Pentylone is a stimulant type drug, with effects similar to that of cocaine, with some additional activity at serotonin receptors. Synthetic cathinone users report psychological, cardiovascular, and neurological sympathomimetic symptoms, with effects ranging from tachycardia, vasoconstriction, seizures, agitation, aggression, and psychosis. Synthetic cathinones, including pentylone, are increasingly being detected in a range of forensic toxicology cases, including both human performance and postmortem cases. Ethylone 50 ng/mL 10 Results for sample 17001213-001 are continued on next page Page 1 of 3 NMS v.40.0 NMS Labs CONFIDENTIAL 200 Welsh Road, Horsham, PA 19044-2208 Phone: (215) 657-4900 Fax: (215) 657-2972 e-mail: [email protected] Robert A. -

Written Witness Statement for U.S. Sentencing Commission's Public
Prepared for the United States Sentencing Commission OPINION TESTIMONY ON SYNTHETIC CATHINONES FOR THE PUBLIC HEARING ON OCTOBER 4, 2017 Gregory B. Dudley, Ph.D. Introduction I provide personal opinions and recommendations on how to incorporate new synthetic cathinone controlled substances into the Sentencing Guidelines. Recommendations include listing specific substances as well as providing categorical coverage of other Schedule I or II cathinones. Personal opinions are informed by the scientific literature, review of the current Guidelines, and observations from having served as an expert witness at sentencing hearings over the past few years. Summary of recommended revisions proposed in the context of the current discussion Under Cocaine and Other Schedule I and II Stimulants (and their immediate precursors), I propose inserting the following lines between Methcathinone and N-N-Dimethylamphetamine, as follows:† • 1 gm of Methcathinone = 380 gm of marijuana • 1 gm of Cathinone = 380 gm of marijuana • 1 gm of 3,4-Methylenedioxymethcathinone/Methylone = 100 gm of marijuana • 1 gm of a-pyrrolidinovalerophenone/alpha-PVP = 100 gm of marijuana • 1 gm of 3,4-Methylenedioxy-a-pyrrolidinovalerophenone/MDPV = 40 gm of marijuana • 1 gm of Other Synthetic Cathinone Substances (unless covered elsewhere in these Guidelines) = 100 gm of marijuana • 1 gm of N-N-Dimethylamphetamine = 40 gm of marijuana O O O O O CH H H 3 N NH2 O N N O N N CH3 CH3 CH3 CH3 CH3 O CH3 O CH3 methcathinone cathinone methylone alpha-PVP CH3 MDPV CH3 N,N-dimethyl- (3,4-methylenedioxy- (α-pyrrolidino- (3,4-methylenedioxy- amphetamine methcathinone) valerophenone) α-pyrrolidino- valerophenone) Outline • Definition of a synthetic cathinone substance • Cathinone substances covered under the current Guidelines • Specific synthetic cathinones recommended for inclusion • The importance of categorical coverage exemplified with dibutylone † Note that I recommend the explicit inclusion of “cathinone”, the parent structure of the synthetic cathinones structure class, to the Guidelines. -

221-D100 Controlled Substances Procedures Manual
Department of Forensic Science COPYRIGHT © 2021 CONTROLLEDVIRGINIA SUBSTANCES PROCEDURESDEPARTMENT MANUAL OF FORENSIC SCIENCE 221-D100 Controlled Substances Procedures Manual Qualtrax ID: 2480 Issued by Chemistry Program Manager UNCONTROLLED Qualtrax Revision 18 Issue Date: 18-August-2021 Page 1 of 176 COPY Table of Contents TABLE OF CONTENTS 1 Introduction 1.1 Introduction 1.2 Examination Documentation 2 Analytical Schemes 2.1 Introduction 2.2 Determination of Quantity 2.3 General Unknowns/Powders/Illicit Tablets 2.4 Tablets and Capsules 2.5 Cannabis 2.6 Pharmaceutical Identifiers 2.7 Color Tests 2.8 Chromatography 2.9 Infrared Spectroscopy/MassCOPYRIGHT Spectrometry © 2021 2.10 Further Testing 2.11 Liquids 2.12 Plant Material 3 Drug Item Reduction Program VIRGINIA 3.1 Introduction DEPARTMENT 3.2 Procedures 4 Weighing Practices OF 4.1 Procedures FORENSIC SCIENCE 4.2 Weighing Practices 4.3 References 5 Sampling 5.1 Introduction 5.2 General Sampling 5.3 Administrative Sampling Plan 5.4 Hypergeometric Sampling Plan 5.5 Multiple Specimens 5.6 Bulk Materials 5.7 Residue Samples 5.8 Sampling for Quantitative Analysis 5.9 References 6 Cannabis Plant Material 6.1 Introduction 6.2 Macroscopic Identification 6.3 Microscopic Identification 6.4 4-Aminophenol (4-AP) Color Test 6.5 Duquenois-Levine 6.6 Thin Layer Chromatography (TLC) 6.7 DART-TOF 6.8 Semi-quantitative Gas Chromatography-Flame Ionization-Mass Spectrometry (GC-FID-MS) 6.9 Quantitative Analysis of Total THC in Plant Material using GC/MS (SIM) 6.10 Residues 221-D100 Controlled Substances