Core Submission Dossier
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

214120Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 214120Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review NDA Multidisciplinary Review and Evaluation Application Number NDA 214120 Application Type Type 3 Priority or Standard Priority Submit Date 3/3/2020 Received Date 3/3/2020 PDUFA Goal Date 9/3/2020 Office/Division OOD/DHM1 Review Completion Date 9/1/2020 Applicant Celgene Corporation Established Name Azacitidine (Proposed) Trade Name Onureg Pharmacologic Class Nucleoside metabolic inhibitor Formulations Tablet (200 mg, 300 mg) (b) (4) Applicant Proposed Indication/Population Recommendation on Regulatory Regular approval Action Recommended Indication/ For continued treatment of adult patients with acute Population myeloid leukemia who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (CRi) following intensive induction chemotherapy and are not able to complete intensive curative therapy. SNOMED CT for the Recommended 91861009 Indication/Population Recommended Dosing Regimen 300 mg orally daily on Days 1 through 14 of each 28-day cycle Reference ID: 4664570 NDA Multidisciplinary Review and Evaluation NDA 214120 Onureg (azacitidine tablets) TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................... 2 TABLE OF TABLES ....................................................................................................................................... -
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
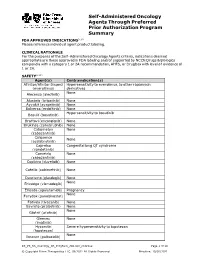
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

An Overview of the Role of Hdacs in Cancer Immunotherapy
International Journal of Molecular Sciences Review Immunoepigenetics Combination Therapies: An Overview of the Role of HDACs in Cancer Immunotherapy Debarati Banik, Sara Moufarrij and Alejandro Villagra * Department of Biochemistry and Molecular Medicine, School of Medicine and Health Sciences, The George Washington University, 800 22nd St NW, Suite 8880, Washington, DC 20052, USA; [email protected] (D.B.); [email protected] (S.M.) * Correspondence: [email protected]; Tel.: +(202)-994-9547 Received: 22 March 2019; Accepted: 28 April 2019; Published: 7 May 2019 Abstract: Long-standing efforts to identify the multifaceted roles of histone deacetylase inhibitors (HDACis) have positioned these agents as promising drug candidates in combatting cancer, autoimmune, neurodegenerative, and infectious diseases. The same has also encouraged the evaluation of multiple HDACi candidates in preclinical studies in cancer and other diseases as well as the FDA-approval towards clinical use for specific agents. In this review, we have discussed how the efficacy of immunotherapy can be leveraged by combining it with HDACis. We have also included a brief overview of the classification of HDACis as well as their various roles in physiological and pathophysiological scenarios to target key cellular processes promoting the initiation, establishment, and progression of cancer. Given the critical role of the tumor microenvironment (TME) towards the outcome of anticancer therapies, we have also discussed the effect of HDACis on different components of the TME. We then have gradually progressed into examples of specific pan-HDACis, class I HDACi, and selective HDACis that either have been incorporated into clinical trials or show promising preclinical effects for future consideration. -

Research in Your Backyard Developing Cures, Creating Jobs
Research in Your Backyard Developing Cures, Creating Jobs PHARMACEUTICAL CLINICAL TRIALS IN ILLINOIS Dots show locations of clinical trials in the state. Executive Summary This report shows that biopharmaceutical research com- Quite often, biopharmaceutical companies hire local panies continue to be vitally important to the economy research institutions to conduct the tests and in Illinois, and patient health in Illinois, despite the recession. they help to bolster local economies in communities all over the state, including Chicago, Decatur, Joliet, Peoria, At a time when the state still faces significant economic Quincy, Rock Island, Rockford and Springfield. challenges, biopharmaceutical research companies are conducting or have conducted more than 4,300 clinical For patients, the trials offer another potential therapeutic trials of new medicines in collaboration with the state’s option. Clinical tests may provide a new avenue of care for clinical research centers, university medical schools and some chronic disease sufferers who are still searching for hospitals. Of the more than 4,300 clinical trials, 2,334 the medicines that are best for them. More than 470 of the target or have targeted the nation’s six most debilitating trials underway in Illinois are still recruiting patients. chronic diseases—asthma, cancer, diabetes, heart dis- ease, mental illnesses and stroke. Participants in clinical trials can: What are Clinical Trials? • Play an active role in their health care. • Gain access to new research treatments before they In the development of new medicines, clinical trials are are widely available. conducted to prove therapeutic safety and effectiveness and compile the evidence needed for the Food and Drug • Obtain expert medical care at leading health care Administration to approve treatments. -

Expression of Genes by Hypomethylating Agents
Wolff et al. Cell Communication and Signaling (2017) 15:13 DOI 10.1186/s12964-017-0168-z REVIEW Open Access The double-edged sword of (re)expression of genes by hypomethylating agents: from viral mimicry to exploitation as priming agents for targeted immune checkpoint modulation Florian Wolff1, Michael Leisch2, Richard Greil2,3,4, Angela Risch1,4 and Lisa Pleyer2,3,4* Abstract Hypomethylating agents (HMAs) have been widely used over the last decade, approved for use in myelodysplastic syndrome (MDS), chronic myelomonocytic leukemia (CMML) and acute myeloid leukemia (AML). The proposed central mechanism of action of HMAs, is the reversal of aberrant methylation in tumor cells, thus reactivating CpG-island promoters and leading to (re)expression of tumor suppressor genes. Recent investigations into the mode of action of azacitidine (AZA) and decitabine (DAC) have revealed new molecular mechanisms that impinge on tumor immunity via induction of an interferon response, through activation of endogenous retroviral elements (ERVs) that are normally epigenetically silenced. Although the global demethylation of DNA by HMAs can induce anti-tumor effects, it can also upregulate the expression of inhibitory immune checkpoint receptors and their ligands, resulting in secondary resistance to HMAs. Recent studies have, however, suggested that this could be exploited to prime or (re)sensitize tumors to immune checkpoint inhibitor therapies. In recent years, immune checkpoints have been targeted by novel therapies, with the aim of (re)activating the host immune system to specifically eliminate malignant cells. Antibodies blocking checkpoint receptors have been FDA-approved for some solid tumors and a plethora of clinical trials testing these and other checkpoint inhibitors are under way. -

Epigenetics in Clinical Practice: the Examples of Azacitidine and Decitabine in Myelodysplasia and Acute Myeloid Leukemia
Leukemia (2013) 27, 1803–1812 & 2013 Macmillan Publishers Limited All rights reserved 0887-6924/13 www.nature.com/leu SPOTLIGHT REVIEW Epigenetics in clinical practice: the examples of azacitidine and decitabine in myelodysplasia and acute myeloid leukemia EH Estey Randomized trials have clearly demonstrated that the hypomethylating agents azacitidine and decitabine are more effective than ‘best supportive care’(BSC) in reducing transfusion frequency in ‘low-risk’ myelodysplasia (MDS) and in prolonging survival compared with BSC or low-dose ara-C in ‘high-risk’ MDS or acute myeloid leukemia (AML) with 21–30% blasts. They also appear equivalent to conventional induction chemotherapy in AML with 420% blasts and as conditioning regimens before allogeneic transplant (hematopoietic cell transplant, HCT) in MDS. Although azacitidine or decitabine are thus the standard to which newer therapies should be compared, here we discuss whether the improvement they afford in overall survival is sufficient to warrant a designation as a standard in treating individual patients. We also discuss pre- and post-treatment covariates, including assays of methylation to predict response, different schedules of administration, combinations with other active agents and use in settings other than active disease, in particular post HCT. We note that rational development of this class of drugs awaits delineation of how much of their undoubted effect in fact results from hypomethylation and reactivation of gene expression. Leukemia (2013) 27, 1803–1812; doi:10.1038/leu.2013.173 -

Cyclacel Announces Grants of New U.S. & European Patents
February 12, 2013 Cyclacel Announces Grants of New U.S. & European Patents Covering Sapacitabine Used in Combination With HDAC Inhibitors Granted Patents Provide Exclusivity for Potential Uses of Sapacitabine in Hematological Malignancies and Solid Tumors BERKELEY HEIGHTS, N.J., Feb. 12, 2013 (GLOBE NEWSWIRE) -- Cyclacel Pharmaceuticals, Inc. (Nasdaq:CYCC) (Nasdaq:CYCCP) (Cyclacel or the Company), a biopharmaceutical company developing oral therapies that target the various phases of cell cycle control for the treatment of cancer and other serious disorders, today announced the issuance of U.S. Patent No. US 8,349,792 ('792) and European Patent No 2,101,790 ('790). Both patents include claims to combination treatment of sapacitabine, the Company's lead product candidate, with HDAC (histone deacetylase) inhibitors. The patents provide exclusivity until June 2029 and December 2027 respectively. "The grants of the '792 and '790 patents are important enhancements of sapacitabine's intellectual property estate. They supplement sapacitabine's existing composition of matter, dosing regimen and combination treatment patent protection and support US and EU market exclusivity toward the end of the next decade," said Spiro Rombotis, President and Chief Executive Officer of Cyclacel. "We are pursuing a broad intellectual property strategy providing us with a strong foundation to achieve our clinical and commercial objectives for sapacitabine and our other assets. As we continue to enroll SEAMLESS, our pivotal Phase 3 trial of sapacitabine as front-line treatment in elderly patients with acute myeloid leukemia (AML), we look forward to providing additional updates for sapacitabine this year, including Phase 2 data in myelodysplastic syndromes (MDS), AML preceded by MDS, and solid tumors." The two patents include claims to combinations of sapacitabine and HDAC inhibitors, pharmaceutical compositions comprising sapacitabine and HDAC inhibitors, and methods of treatment using such compositions of proliferative disorders including leukemias, lymphomas, and lung cancer. -

Biological Heterogeneity of Chondrosarcoma: from (Epi) Genetics Through Stemness and Deregulated Signaling to Immunophenotype
cancers Review Biological Heterogeneity of Chondrosarcoma: From (Epi) Genetics through Stemness and Deregulated Signaling to Immunophenotype Agnieszka Zaj ˛ac 1 , Sylwia K. Król 2 , Piotr Rutkowski 1 and Anna M. Czarnecka 1,3,* 1 Department of Soft Tissue/Bone Sarcoma and Melanoma, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] (A.Z.); [email protected] (P.R.) 2 Department of Molecular and Translational Oncology, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] 3 Department of Experimental Pharmacology, Mossakowski Medical Research Centre, Polish Academy of Sciences, 02-176 Warsaw, Poland * Correspondence: [email protected] Simple Summary: Chondrosarcoma (ChS) is the second most frequently diagnosed malignant bone tumor of cartilaginous origin and is generally resistant to standard treatment options. In this paper, we aim to review the current state of the knowledge regarding ChS. We discuss the genetic, epigenetic, and molecular abnormalities underlying its substantial biological and clinical heterogeneity. This review summarizes the critical genetic and molecular drivers of ChS development and progression, contributing to its radio- and chemotherapy resistance. We describe genomic aberrations and point mutations, as well as epigenetic modifications and deregulated signal transduction pathways. We Citation: Zaj ˛ac,A.; Król, S.K.; provide an insight into the stem-like characteristics and immunophenotype of ChS. The paper also Rutkowski, P.; Czarnecka, A.M. outlines potential diagnostic and prognostic biomarkers of ChS and recently identified novel targets Biological Heterogeneity of for future pharmacological interventions in patients. Chondrosarcoma: From (Epi) Genetics through Stemness and Abstract: Deregulated Signaling to Chondrosarcoma (ChS) is a primary malignant bone tumor. -

BCBSVT Specialty Drug List Effective 2021.07.01.Xlsx
Effective Date: 07/01/2021 SPECIALTY DRUG LIST Revised Date: 05/07/2021 DOSAGE EXCLUDED ON NATIONAL DRUG CLASS DRUG NAME GENERIC NAME FORM PERFORMANCE FORMULARY ANEMIA ARANESP SOLN DARBEPOETIN ALFA SOLN INJ ANEMIA ARANESP SOSY DARBEPOETIN ALFA SOLN PREFILLED SYRINGE ANEMIA EPOGEN SOLN EPOETIN ALFA INJ X ANEMIA PROCRIT SOLN EPOETIN ALFA INJ X ANEMIA REBLOZYL SOLR LUSPATERCEPT-AAMT FOR SUBCUTANEOUS INJ ANEMIA RETACRIT SOLN EPOETIN ALFA-EPBX INJ ANTI-GOUT AGENT KRYSTEXXA SOLN PEGLOTICASE INJ (FOR IV INFUSION) ANTI-INFECTIVE PREVYMIS SOLN LETERMOVIR IV SOLN ANTI-INFECTIVE PREVYMIS TABS LETERMOVIR TAB ASTHMA CINQAIR SOLN RESLIZUMAB IV INFUSION SOLN ASTHMA FASENRA SOSY BENRALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE ASTHMA FASENRA PEN SOAJ BENRALIZUMAB SUBCUTANEOUS SOLN AUTO-INJECTOR ASTHMA NUCALA SOAJ MEPOLIZUMAB SUBCUTANEOUS SOLUTION AUTO-INJECTOR ASTHMA NUCALA SOLR MEPOLIZUMAB FOR INJ ASTHMA NUCALA SOSY MEPOLIZUMAB SUBCUTANEOUS SOLUTION PREF SYRINGE ASTHMA XOLAIR SOLR OMALIZUMAB FOR INJ ASTHMA XOLAIR SOSY OMALIZUMAB SUBCUTANEOUS SOLN PREFILLED SYRINGE CARDIOVASCULAR VYNDAMAX CAPS TAFAMIDIS CAP CARDIOVASCULAR VYNDAQEL CAPS TAFAMIDIS MEGLUMINE (CARDIAC) CAP CENTRAL NERVOUS SYSTEM AGENTS AUSTEDO TABS DEUTETRABENAZINE TAB CENTRAL NERVOUS SYSTEM AGENTS ENSPRYNG SOSY SATRALIZUMAB-MWGE SUBCUTANEOUS SOLN PREF SYRINGE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ CAPS TASIMELTEON CAPSULE CENTRAL NERVOUS SYSTEM AGENTS HETLIOZ LQ SUSP TASIMELTEON ORAL SUSP CHEMOTHERAPY PROTECTANT AMIFOSTINE SOLR AMIFOSTINE CRYSTALLINE FOR INJ CHEMOTHERAPY PROTECTANT ELITEK -

Chemotherapeutic Treatment of Acute Myeloid Leukemia
Clinical Trial Outcomes Mahdi, Mahdi & Knapper Chemotherapeutic treatment of acute myeloid leukemia 5 Clinical Trial Outcomes Chemotherapeutic treatment of acute myeloid leukemia: incorporating the results of recent clinical trials Clin. Invest. (Lond.) Better outcomes for patients with acute myeloid leukemia over the last 30 years have Ali J Mahdi*,1, Eamon J been largely achieved by improvements in supportive care measures rather than Mahdi1 & Steven Knapper1 therapeutic advances. The combination of daunorubicin and cytarabine has remained 1Cardiff University School of Medicine, Hematology Department, Heath Park, the standard of care for patients undergoing intensive induction–consolidation Cardiff CF14 4XN, UK treatment. In less fit older patients, low-dose cytarabine is the equivalent, although *Author for correspondence: the hypomethylating agent azacitidine may be challenging current practice. [email protected] Enhanced understanding of disease pathogenesis and therapy resistance has enabled the entry of novel chemotherapeutic and nonchemotherapeutic agents into clinical development with varied levels of activity. This article examines the evidence behind established chemotherapy practices for intensive and nonintensive acute myeloid leukemia treatments with an emphasis on emerging clinical trial data from novel chemotherapeutic and nonchemotherapeutic agents. Keywords: acute myeloid leukemia • aminopeptidase inhibitors • farnesyl transferase inhibitors • FLT3 inhibitors • gemtuzumab ozogamicin • histone deacytylase inhibitors • hypomethylating • Polo-like kinase 1 inhibitors Methodology AML cases [7]. Older patients over the age of 10.4155/CLI.14.112 An electronic database search (EMBASE, 60 years thus represent an important popula- MEDLINE and PubMed) was undertaken tion from both demographic and therapeutic to identify and review clinical studies in perspectives. Older patients frequently have acute myeloid leukemia (AML) undertaken multiple comorbidities, unfavorable cyto- between 1 January 2009 and 1 June 2014. -

Draft COMP Agenda 16-18 January 2018
12 January 2018 EMA/COMP/818236/2017 Inspections, Human Medicines Pharmacovigilance and Committees Committee for Orphan Medicinal Products (COMP) Draft agenda for the meeting on 16-18 January 2018 Chair: Bruno Sepodes – Vice-Chair: Lesley Greene 16 January 2018, 09:00-19:30, room 2F 17 January 2018, 08:30-19:30, room 2F 18 January 2018, 08:30-18:30, room 2F Health and safety information In accordance with the Agency’s health and safety policy, delegates are to be briefed on health, safety and emergency information and procedures prior to the start of the meeting. Disclaimers Some of the information contained in this agenda is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the COMP meeting reports once the procedures are finalised. Of note, this agenda is a working document primarily designed for COMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the agenda cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). -

WO 2010/135468 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 25 November 2010 (25.11.2010) WO 2010/135468 Al (51) International Patent Classification: [US/ES]; C/ Rio EsIa 77 PO2 A Villamayor, E-37007 GOlN 33/50 (2006.01) Salamanca (ES). LAGO, Santiago [GB/ES]; C/ Fernando Camino 15 3-E, E-29016 Malaga (ES). MATOSES, (21) International Application Number: Maria [ES/ES]; C/ Los Cristos 1 1 C, E-29008 Malaga PCT/US2010/035474 (ES). SUAREZ, Lilia [ES/ES]; C/ Ancla, 27 Casa 13, (22) International Filing Date: E-29720 CaIa Del Moral (ES). SAPIA, Sandra [IT/ES]; 19 May 2010 (19.05.2010) C/ Zapateros, 2 2 C, E-29005 Malaga (ES). BOSAN- QUET, Andrew [GB/GB]; 4 The Brow, Church Road, English (25) Filing Language: Combe Down, BA2 5JL, Bath (GB). GOR- (26) Publication Language: English ROCHATEGUI, Julian [ES/ES]; C/Puerto de los Leones 5, Majadahonda, E-28220 Madrid (ES). (30) Priority Data: TUDELA, Consuelo [ES/ES]; Av. Juan Carlos I 23, M a 61/179,685 19 May 2009 (19.05.2009) US jadahonda, E-28220 Madrid (ES). HERNANDEZ, Pilar (71) Applicant (for all designated States except US): VIVIA [ES/ES]; C/Uruguay 16, E-37OO3 Salamanca (ES). BIOTECH S.L. [ES/ES]; C/ Menendez Pelayo 12, 3d, CAVEDA, Luis Ignacio [ES/ES]; Av. Valladolid 17, E-47001 Valladolid (ES). E-28008 Madrid (ES). (72) Inventors; and (74) Agent: MALLON, Joseph, J.; Knobbe Martens Olson & (75) Inventors/Applicants (for US only): BALLESTEROS, Bear LLP, 2040 Main Street, 14th Floor, Irvine, CA Juan [ES/ES]; C/ Espalter 8 - 7 B, E-28014 Madrid (ES).