Topical Immunomodulators in Dermatology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Complementary and Alternative Treatments for Alopecia: a Comprehensive Review
Review Article Skin Appendage Disord 2019;5:72–89 Received: April 22, 2018 DOI: 10.1159/000492035 Accepted: July 10, 2018 Published online: August 21, 2018 Complementary and Alternative Treatments for Alopecia: A Comprehensive Review Anna-Marie Hosking Margit Juhasz Natasha Atanaskova Mesinkovska Department of Dermatology, University of California, Irvine, Irvine, CA, USA Keywords Introduction Alopecia · Complementary and alternative medicine · Efficacy According to the National Center for Complementary and Integrative Health (NCCIH), a branch of the Nation- al Institutes of Health (NIH; Bethesda, MD, USA), more Abstract than 30% of adults and 12% of children utilize treatments The treatment of alopecia is limited by a lack of therapies developed “outside of mainstream Western, or conven- that induce and sustain disease remission. Given the nega- tional, medicine,” with a total USD 30.2 billion out-of- tive psychosocial impact of hair loss, patients that do not pocket dollars spent annually [1]. In the treatment of alo- see significant hair restoration with conventional therapies pecia, there is an unmet need for therapies providing sat- often turn to complementary and alternative medicine isfying, long-term results. Patients often turn to (CAM). Although there are a variety of CAM treatment op- complementary and alternative medicine (CAM) in an tions on the market for alopecia, only a few are backed by attempt to find safe, natural, and efficacious therapies to multiple randomized controlled trials. Further, these mo- restore hair. Although CAMs boast hair-growing poten- dalities are not regulated by the Food and Drug Administra- tial, patients may be disappointed with results as there is tion and there is a lack of standardization of bioactive in- a lack of standardization of bioactive ingredients and lim- gredients in over-the-counter vitamins, herbs, and supple- ited scientific evidence. -

WO 2014/167554 A2 16 October 2014 (16.10.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/167554 A2 16 October 2014 (16.10.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 47/10 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/IB20 14/060675 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 12 April 2014 (12.04.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: zw. 1103/DEL/2013 12 April 2013 (12.04.2013) IN (84) Designated States (unless otherwise indicated, for every (71) Applicant: VYOME BIOSCIENCES PVT. LTD. kind of regional protection available): ARIPO (BW, GH, [IN/IN]; 459 F.I.E, First Floor, Patparganj Industrial Area, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, New Delhi 110092 (IN). -

Herb Lotions to Regrow Hair in Patients with Intractable Alopecia Areata Hideo Nakayama*, Ko-Ron Chen Meguro Chen Dermatology Clinic, Tokyo, Japan
Clinical and Medical Investigations Research Article ISSN: 2398-5763 Herb lotions to regrow hair in patients with intractable alopecia areata Hideo Nakayama*, Ko-Ron Chen Meguro Chen Dermatology Clinic, Tokyo, Japan Abstract The history of herbal medicine in China goes back more than 1,000 years. Many kinds of mixtures of herbs that are effective to diseases or symptoms have been transmitted from the middle ages to today under names such as Traditional Chinese Medicine (TCM) in China and Kampo in Japan. For the treatment of severe and intractable alopecia areata, such as alopecia universalis, totalis, diffusa etc., herb lotions are known to be effective in hair regrowth. Laiso®, Fukisin® in Japan and 101® in China are such effective examples. As to treat such cases, systemic usage of corticosteroid hormones are surely effective, however, considering their side effects, long term usage should be refrained. There are also these who should refrain such as small children, and patients with peptic ulcers, chronic infections and osteoporosis. AL-8 and AL-4 were the prescriptions removing herbs which are not allowed in Japanese Pharmacological regulations from 101, and salvia miltiorrhiza radix (SMR) is the most effective herb for hair growth, also the causation to produce contact sensitization. Therefore, the mechanism of hair growth of these herb lotions in which the rate of effectiveness was in average 64.8% on 54 severe intractable cases of alopecia areata, was very similar to DNCB and SADBE. The most recommended way of developing herb lotion with high ability of hairgrowth is to use SMR but its concentration should not exceed 2%, and when sensitization occurs, the lotion should be changed to Laiso® or Fukisin®, which do not contain SMR. -

Hypertrichosis in Alopecia Universalis and Complex Regional Pain Syndrome
NEUROIMAGES Hypertrichosis in alopecia universalis and complex regional pain syndrome Figure 1 Alopecia universalis in a 46-year- Figure 2 Hypertrichosis of the fifth digit of the old woman with complex regional complex regional pain syndrome– pain syndrome I affected hand This 46-year-old woman developed complex regional pain syndrome (CRPS) I in the right hand after distor- tion of the wrist. Ten years before, the diagnosis of alopecia areata was made with subsequent complete loss of scalp and body hair (alopecia universalis; figure 1). Apart from sensory, motor, and autonomic changes, most strikingly, hypertrichosis of the fifth digit was detectable on the right hand (figure 2). Hypertrichosis is common in CRPS.1 The underlying mechanisms are poorly understood and may involve increased neurogenic inflammation.2 This case nicely illustrates the powerful hair growth stimulus in CRPS. Florian T. Nickel, MD, Christian Maiho¨fner, MD, PhD, Erlangen, Germany Disclosure: The authors report no disclosures. Address correspondence and reprint requests to Dr. Florian T. Nickel, Department of Neurology, University of Erlangen-Nuremberg, Schwabachanlage 6, 91054 Erlangen, Germany; [email protected] 1. Birklein F, Riedl B, Sieweke N, Weber M, Neundorfer B. Neurological findings in complex regional pain syndromes: analysis of 145 cases. Acta Neurol Scand 2000;101:262–269. 2. Birklein F, Schmelz M, Schifter S, Weber M. The important role of neuropeptides in complex regional pain syndrome. Neurology 2001;57:2179–2184. Copyright © 2010 by -

Xeljanz Shows Promise As Treatment for Alopecia Areata in Adolescents
Xeljanz shows promise as treatment for alopecia areata in adole... http://www.healio.com/dermatology/hair-nails/news/online/{0c... IN THE JOURNALS Xeljanz shows promise as treatment for alopecia areata in adolescents Craiglow BG, et al. J Am Acad Dermatol. 2016;doi:10.1016/j.jaad.2016.09.006. November 3, 2016 Treatment with Xeljanz in adolescents with alopecia areata resulted in significant hair regrowth for the majority of the patients, with mild adverse events, according to recently published study results. Brent A. King, MD, PhD, assistant professor of dermatology, Yale School of Medicine, and colleagues studied 13 adolescent patients (median age 15 years; 77% male) with alopecia areata treated with Xeljanz (tofacitinib, Pfizer) between July 2014 and May 2016 at a tertiary care center clinic. They used the Severity of Alopecia Tool (SALT) to measure severity of disease, and laboratory monitoring, physical examinations and review of systems to measure adverse events. The patients were treated for a median duration of 5 months. Patient age ranged from 12 to 17 years at time of treatment initiation. Six patients had alopecia universalis, one had alopecia totalis and six had alopecia areata. The median duration of disease before beginning therapy of Brent A. King 8 years. All patients received tofacitinib 5 mg twice daily. One patient who had complete regrowth over 5 months developed four 1- to 3-cm patches of alopecia, and received an increased dose of 10 mg in the morning and 5 mg in the evening, with full regrowth occurring again. Clinically significant hair growth was experienced by nine patients, and very minimal hair growth was experienced by three patients. -

What's the Best Treatment for Cradle Cap?
From the CLINIcAL InQUiRiES Family Physicians Inquiries Network Ryan C. Sheffield, MD, Paul Crawford, MD What’s the best treatment Eglin Air Force Base Family Medicine Residency, Eglin Air for cradle cap? Force Base, Fla Sarah Towner Wright, MLS University of North Carolina at Chapel Hill Evidence-based answer Ketoconazole (Nizoral) shampoo appears corticosteroids to severe cases because to be a safe and efficacious treatment of possible systemic absorption (SOR: C). for infants with cradle cap (strength of Overnight application of emollients followed recommendation [SOR]: C, consensus, by gentle brushing and washing with usual practice, opinion, disease-oriented baby shampoo helps to remove the scale evidence, and case series). Limit topical associated with cradle cap (SOR: C). ® Dowden Health Media Clinical commentary ICopyrightf parents can’t leave it be, recommend brush to loosen the scale. Although mineral oil andFor a brush personal to loosen scale use noonly evidence supports this, it seems safe Cradle cap is distressing to parents. They and is somewhat effective. want everyone else to see how gorgeous This review makes me feel more FAST TRACK their new baby is, and cradle cap can make comfortable with recommending ketocon- their beautiful little one look scruffy. My azole shampoo when mineral oil proves If parents need standard therapy has been to stress to the insufficient. For resistant cases, a cute hat to do something, parents that it isn’t a problem for the baby. can work wonders. If the parents still want to do something -

An Unpleasant Reality with Interferon Alfa-2B and Ribavirin Treatment for Hepatitis C
Advanced Research in Gastroenterology & Hepatology Case Report Adv Res Gastroentero Hepatol Volume 1 Issue 3 - January 2016 Copyright © All rights are reserved by Parveen Malhotra Alopecia Universalis- An Unpleasant Reality with Interferon Alfa-2b and Ribavirin Treatment for Hepatitis C Parveen Malhotra*, Naveen Malhotra, Vani Malhotra, Ajay Chugh, Abhishek Chaturvedi, Parul Chandrika and Ishita Singh Department of Medical Gastroenterology, Anaesthesiology, Obstetrics & Gynaecology, Pt.B.D.S. Post Graduate Institute of Medical Sciences (PGIMS), India Submission: January 01, 2016; Published: January 29, 2016 *Corresponding author: Parveen Malhotra, Department of Medical Gastroenterology, PGIMS, 128/19, Civil Hospital Road, Rohtak– 124001 (Haryana) India, Tel: 919671000017; Email: Abstract Numerous cutaneous side effects of combination Pegylated interferon alfa-2b (PEG-IFN) and ribavirin (RBV) therapy have been reported. Although cases alopecia areata (AA) associated with PEG-IFN/RBV therapy have been reported in the literature, but alopecia universalis is uncommon entity. We have treated up till now around 3500 patients suffering from this disease with Pegylated Interferon-2b and ribavirin, as oral directly acting antivirals has been recently launched in India. Out of these 3500 patients, 1470 (42%) patients developed alopecia during various stages of treatment, some even after stopping of treatment. Five patients developed Alopecia Universalis (AU) while undergoing the treatment which makes prevalence rate of 14% in total of 3500 but if we calculate prevalence of Alopecia Universalis in patients who developed alopecia on treatment, it increases to 34%. Now the good thing is that we have already entered the phase of Interferon free treatment in India, thus patients will get rid of these frustrating side effects like AA and AU which undermines the importance of successful treatment after achievement of sustained virological response. -

Alopecia Areata: Evidence-Based Treatments
Alopecia Areata: Evidence-Based Treatments Seema Garg and Andrew G. Messenger Alopecia areata is a common condition causing nonscarring hair loss. It may be patchy, involve the entire scalp (alopecia totalis) or whole body (alopecia universalis). Patients may recover spontaneously but the disorder can follow a course of recurrent relapses or result in persistent hair loss. Alopecia areata can cause great psychological distress, and the most important aspect of management is counseling the patient about the unpredictable nature and course of the condition as well as the available effective treatments, with details of their side effects. Although many treatments have been shown to stimulate hair growth in alopecia areata, there are limited data on their long-term efficacy and impact on quality of life. We review the evidence for the following commonly used treatments: corticosteroids (topical, intralesional, and systemic), topical sensitizers (diphenylcyclopropenone), psor- alen and ultraviolet A phototherapy (PUVA), minoxidil and dithranol. Semin Cutan Med Surg 28:15-18 © 2009 Elsevier Inc. All rights reserved. lopecia areata (AA) is a chronic inflammatory condition caus- with AA having nail involvement. Recovery can occur spontaneously, Aing nonscarring hair loss. The lifetime risk of developing the although hair loss can recur and progress to alopecia totalis (total loss of condition has been estimated at 1.7% and it accounts for 1% to 2% scalp hair) or universalis (both body and scalp hair). Diagnosis is usu- of new patients seen in dermatology clinics in the United Kingdom ally made clinically, and investigations usually are unnecessary. Poor and United States.1 The onset may occur at any age; however, the prognosis is linked to the presence of other immune diseases, family majority (60%) commence before 20 years of age.2 There is equal history of AA, young age at onset, nail dystrophy, extensive hair loss, distribution of incidence across races and sexes. -
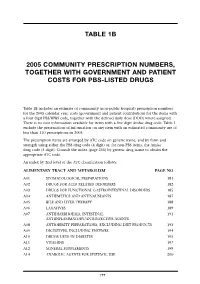
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

Case of Persistent Regrowth of Blond Hair in a Previously Brunette Alopecia Areata Totalis Patient
Case of Persistent Regrowth of Blond Hair in a Previously Brunette Alopecia Areata Totalis Patient Karla Snider, DO,* John Young, MD** *PGYIII, Silver Falls Dermatology/Western University, Salem, OR **Program Director, Dermatology Residency Program, Silver Falls Dermatology, Salem, OR Abstract We present a case of a brunette, 64-year-old female with no previous history of alopecia areata who presented to our clinic with diffuse hair loss over the scalp. She was treated with triamcinolone acetonide intralesional injections and experienced hair re-growth of initially white hair that then partially re-pigmented to blond at the vertex. Two years following initiation of therapy, she continued to have blond hair growth on her scalp with no dark hair re-growth and no recurrence of alopecia areata. Introduction (CBC), comprehensive metabolic panel (CMP), along the periphery of the occipital, parietal and Alopecia areata (AA) is a fairly common thyroid stimulating hormone (TSH) test and temporal scalp), sisaipho pattern (loss of hair in autoimmune disorder of non-scarring hair loss. antinuclear antibody (ANA) test. All values were the frontal parietotemporal scalp), patchy hair unremarkable, and the ANA was negative. The loss (reticular variant) and a diffuse thinning The disease commonly presents as hair loss from 2 any hair-bearing area of the body. Following patient declined a biopsy. variant. Often, “exclamation point hairs” can be hair loss, it is not rare to see initial growth of A clinical diagnosis of alopecia areata was seen in and around the margins of the hair loss. depigmented or hypopigmented hair in areas made. The patient was treated with 5.0 mg/mL The distal ends of these hairs are thicker than the proximal ends, and they are a marker of active of regrowth in the first anagen cycle. -

Zinc Therapy in Dermatology: a Review
Hindawi Publishing Corporation Dermatology Research and Practice Volume 2014, Article ID 709152, 11 pages http://dx.doi.org/10.1155/2014/709152 Review Article Zinc Therapy in Dermatology: A Review Mrinal Gupta, Vikram K. Mahajan, Karaninder S. Mehta, and Pushpinder S. Chauhan DepartmentofDermatology,Venereology&Leprosy,Dr.R.P.Govt.MedicalCollege,Kangra(Tanda),HimachalPradesh176001,India Correspondence should be addressed to Vikram K. Mahajan; [email protected] Received 1 May 2014; Accepted 23 June 2014; Published 10 July 2014 Academic Editor: Craig G. Burkhart Copyright © 2014 Mrinal Gupta et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Zinc, both in elemental or in its salt forms, has been used as a therapeutic modality for centuries. Topical preparations like zinc oxide, calamine, or zinc pyrithione have been in use as photoprotecting, soothing agents or as active ingredient of antidandruff shampoos. Its use has expanded manifold over the years for a number of dermatological conditions including infections (leishmaniasis, warts), inflammatory dermatoses (acne vulgaris, rosacea), pigmentary disorders (melasma), and neoplasias (basal cell carcinoma). Although the role of oral zinc is well-established in human zinc deficiency syndromes including acrodermatitis enteropathica, it is only in recent years that importance of zinc as a micronutrient essential for infant -

Australian Statistics on Medicines 1997 Commonwealth Department of Health and Family Services
Australian Statistics on Medicines 1997 Commonwealth Department of Health and Family Services Australian Statistics on Medicines 1997 i © Commonwealth of Australia 1998 ISBN 0 642 36772 8 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be repoduced by any process without written permission from AusInfo. Requests and enquiries concerning reproduction and rights should be directed to the Manager, Legislative Services, AusInfo, GPO Box 1920, Canberra, ACT 2601. Publication approval number 2446 ii FOREWORD The Australian Statistics on Medicines (ASM) is an annual publication produced by the Drug Utilisation Sub-Committee (DUSC) of the Pharmaceutical Benefits Advisory Committee. Comprehensive drug utilisation data are required for a number of purposes including pharmacosurveillance and the targeting and evaluation of quality use of medicines initiatives. It is also needed by regulatory and financing authorities and by the Pharmaceutical Industry. A major aim of the ASM has been to put comprehensive and valid statistics on the Australian use of medicines in the public domain to allow access by all interested parties. Publication of the Australian data facilitates international comparisons of drug utilisation profiles, and encourages international collaboration on drug utilisation research particularly in relation to enhancing the quality use of medicines and health outcomes. The data available in the ASM represent estimates of the aggregate community use (non public hospital) of prescription medicines in Australia. In 1997 the estimated number of prescriptions dispensed through community pharmacies was 179 million prescriptions, a level of increase over 1996 of only 0.4% which was less than the increase in population (1.2%).