Parasitology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Entamoeba Histolytica
Journal of Clinical Microbiology and Biochemical Technology Piotr Nowak1*, Katarzyna Mastalska1 Review Article and Jakub Loster2 1Laboratory of Parasitology, Department of Microbiology, University Hospital in Krakow, 19 Entamoeba Histolytica - Pathogenic Kopernika Street, 31-501 Krakow, Poland 2Department of Infectious Diseases, University Protozoan of the Large Intestine in Hospital in Krakow, 5 Sniadeckich Street, 31-531 Krakow, Poland Humans Dates: Received: 01 December, 2015; Accepted: 29 December, 2015; Published: 30 December, 2015 *Corresponding author: Piotr Nowak, Laboratory of Abstract Parasitology, Department of Microbiology, University Entamoeba histolytica is a cosmopolitan, parasitic protozoan of human large intestine, which is Hospital in Krakow, 19 Kopernika Street, 31- 501 a causative agent of amoebiasis. Amoebiasis manifests with persistent diarrhea containing mucus Krakow, Poland, Tel: +4812/4247587; Fax: +4812/ or blood, accompanied by abdominal pain, flatulence, nausea and fever. In some cases amoebas 4247581; E-mail: may travel through the bloodstream from the intestine to the liver or to other organs, causing multiple www.peertechz.com abscesses. Amoebiasis is a dangerous, parasitic disease and after malaria the second cause of deaths related to parasitic infections worldwide. The highest rate of infections is observed among people living Keywords: Entamoeba histolytica; Entamoeba in or traveling through the tropics. Laboratory diagnosis of amoebiasis is quite difficult, comprising dispar; Entamoeba moshkovskii; Entamoeba of microscopy and methods of molecular biology. Pathogenic species Entamoeba histolytica has to histolytica sensu lato; Entamoeba histolytica sensu be differentiated from other nonpathogenic amoebas of the intestine, so called commensals, that stricto; commensals of the large intestine; amoebiasis very often live in the human large intestine and remain harmless. -

Proceedings of the Helminthological Society of Washington 51(2) 1984
Volume 51 July 1984 PROCEEDINGS ^ of of Washington '- f, V-i -: ;fx A semiannual journal of research devoted to Helminthohgy and all branches of Parasitology Supported in part by the -•>"""- v, H. Ransom Memorial 'Tryst Fund : CONTENTS -j<:'.:,! •</••• VV V,:'I,,--.. Y~v MEASURES, LENA N., AND Roy C. ANDERSON. Hybridization of Obeliscoides cuniculi r\ XGraybill, 1923) Graybill, ,1924 jand Obeliscoides,cuniculi multistriatus Measures and Anderson, 1983 .........:....... .., :....„......!"......... _ x. iXJ-v- 179 YATES, JON A., AND ROBERT C. LOWRIE, JR. Development of Yatesia hydrochoerus "•! (Nematoda: Filarioidea) to the Infective Stage in-Ixqdid Ticks r... 187 HUIZINGA, HARRY W., AND WILLARD O. GRANATH, JR. -Seasonal ^prevalence of. Chandlerellaquiscali (Onehocercidae: Filarioidea) in Braih, of the Common Grackle " '~. (Quiscdlus quisculd versicolor) '.'.. ;:,„..;.......„.;....• :..: „'.:„.'.J_^.4-~-~-~-<-.ii -, **-. 191 ^PLATT, THOMAS R. Evolution of the Elaphostrongylinae (Nematoda: Metastrongy- X. lojdfea: Protostrongylidae) Parasites of Cervids,(Mammalia) ...,., v.. 196 PLATT, THOMAS R., AND W. JM. SAMUEL. Modex of Entry of First-Stage Larvae ofr _^ ^ Parelaphostrongylus odocoilei^Nematoda: vMefastrongyloidea) into Four Species of Terrestrial Gastropods .....:;.. ....^:...... ./:... .; _.... ..,.....;. .-: 205 THRELFALL, WILLIAM, AND JUAN CARVAJAL. Heliconema pjammobatidus sp. n. (Nematoda: Physalbpteridae) from a Skate,> Psammobatis lima (Chondrichthyes: ; ''•• \^ Rajidae), Taken in Chile _... .„ ;,.....„.......„..,.......;. ,...^.J::...^..,....:.....~L.:....., -
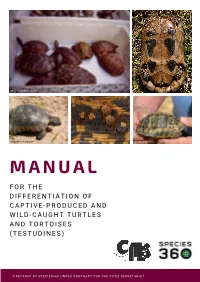
Manual for the Differentiation of Captive-Produced and Wild-Caught Turtles and Tortoises (Testudines)
Image: Peter Paul van Dijk Image:Henrik Bringsøe Image: Henrik Bringsøe Image: Andrei Daniel Mihalca Image: Beate Pfau MANUAL F O R T H E DIFFERENTIATION OF CAPTIVE-PRODUCED AND WILD-CAUGHT TURTLES AND TORTOISES (TESTUDINES) PREPARED BY SPECIES360 UNDER CONTRACT FOR THE CITES SECRETARIAT Manual for the differentiation of captive-produced and wild-caught turtles and tortoises (Testudines) This document was prepared by Species360 under contract for the CITES Secretariat. Principal Investigators: Prof. Dalia A. Conde, Ph.D. and Johanna Staerk, Ph.D., Species360 Conservation Science Alliance, https://www.species360.orG Authors: Johanna Staerk1,2, A. Rita da Silva1,2, Lionel Jouvet 1,2, Peter Paul van Dijk3,4,5, Beate Pfau5, Ioanna Alexiadou1,2 and Dalia A. Conde 1,2 Affiliations: 1 Species360 Conservation Science Alliance, www.species360.orG,2 Center on Population Dynamics (CPop), Department of Biology, University of Southern Denmark, Denmark, 3 The Turtle Conservancy, www.turtleconservancy.orG , 4 Global Wildlife Conservation, globalwildlife.orG , 5 IUCN SSC Tortoise & Freshwater Turtle Specialist Group, www.iucn-tftsG.org. 6 Deutsche Gesellschaft für HerpetoloGie und Terrarienkunde (DGHT) Images (title page): First row, left: Mixed species shipment (imaGe taken by Peter Paul van Dijk) First row, riGht: Wild Testudo marginata from Greece with damaGe of the plastron (imaGe taken by Henrik BrinGsøe) Second row, left: Wild Testudo marginata from Greece with minor damaGe of the carapace (imaGe taken by Henrik BrinGsøe) Second row, middle: Ticks on tortoise shell (Amblyomma sp. in Geochelone pardalis) (imaGe taken by Andrei Daniel Mihalca) Second row, riGht: Testudo graeca with doG bite marks (imaGe taken by Beate Pfau) Acknowledgements: The development of this manual would not have been possible without the help, support and guidance of many people. -

The Intestinal Protozoa
The Intestinal Protozoa A. Introduction 1. The Phylum Protozoa is classified into four major subdivisions according to the methods of locomotion and reproduction. a. The amoebae (Superclass Sarcodina, Class Rhizopodea move by means of pseudopodia and reproduce exclusively by asexual binary division. b. The flagellates (Superclass Mastigophora, Class Zoomasitgophorea) typically move by long, whiplike flagella and reproduce by binary fission. c. The ciliates (Subphylum Ciliophora, Class Ciliata) are propelled by rows of cilia that beat with a synchronized wavelike motion. d. The sporozoans (Subphylum Sporozoa) lack specialized organelles of motility but have a unique type of life cycle, alternating between sexual and asexual reproductive cycles (alternation of generations). e. Number of species - there are about 45,000 protozoan species; around 8000 are parasitic, and around 25 species are important to humans. 2. Diagnosis - must learn to differentiate between the harmless and the medically important. This is most often based upon the morphology of respective organisms. 3. Transmission - mostly person-to-person, via fecal-oral route; fecally contaminated food or water important (organisms remain viable for around 30 days in cool moist environment with few bacteria; other means of transmission include sexual, insects, animals (zoonoses). B. Structures 1. trophozoite - the motile vegetative stage; multiplies via binary fission; colonizes host. 2. cyst - the inactive, non-motile, infective stage; survives the environment due to the presence of a cyst wall. 3. nuclear structure - important in the identification of organisms and species differentiation. 4. diagnostic features a. size - helpful in identifying organisms; must have calibrated objectives on the microscope in order to measure accurately. -

Lecture 5: Emerging Parasitic Helminths Part 2: Tissue Nematodes
Readings-Nematodes • Ch. 11 (pp. 290, 291-93, 295 [box 11.1], 304 [box 11.2]) • Lecture 5: Emerging Parasitic Ch.14 (p. 375, 367 [table 14.1]) Helminths part 2: Tissue Nematodes Matt Tucker, M.S., MSPH [email protected] HSC4933 Emerging Infectious Diseases HSC4933. Emerging Infectious Diseases 2 Monsters Inside Me Learning Objectives • Toxocariasis, larva migrans (Toxocara canis, dog hookworm): • Understand how visceral larval migrans, cutaneous larval migrans, and ocular larval migrans can occur Background: • Know basic attributes of tissue nematodes and be able to distinguish http://animal.discovery.com/invertebrates/monsters-inside- these nematodes from each other and also from other types of me/toxocariasis-toxocara-roundworm/ nematodes • Understand life cycles of tissue nematodes, noting similarities and Videos: http://animal.discovery.com/videos/monsters-inside- significant difference me-toxocariasis.html • Know infective stages, various hosts involved in a particular cycle • Be familiar with diagnostic criteria, epidemiology, pathogenicity, http://animal.discovery.com/videos/monsters-inside-me- &treatment toxocara-parasite.html • Identify locations in world where certain parasites exist • Note drugs (always available) that are used to treat parasites • Describe factors of tissue nematodes that can make them emerging infectious diseases • Be familiar with Dracunculiasis and status of eradication HSC4933. Emerging Infectious Diseases 3 HSC4933. Emerging Infectious Diseases 4 Lecture 5: On the Menu Problems with other hookworms • Cutaneous larva migrans or Visceral Tissue Nematodes larva migrans • Hookworms of other animals • Cutaneous Larva Migrans frequently fail to penetrate the human dermis (and beyond). • Visceral Larva Migrans – Ancylostoma braziliense (most common- in Gulf Coast and tropics), • Gnathostoma spp. Ancylostoma caninum, Ancylostoma “creeping eruption” ceylanicum, • Trichinella spiralis • They migrate through the epidermis leaving typical tracks • Dracunculus medinensis • Eosinophilic enteritis-emerging problem in Australia HSC4933. -

Reconstruction of the Evolutionary History of Haemosporida
Parasitology International 65 (2016) 5–11 Contents lists available at ScienceDirect Parasitology International journal homepage: www.elsevier.com/locate/parint Reconstruction of the evolutionary history of Haemosporida (Apicomplexa) based on the cyt b gene with characterization of Haemocystidium in geckos (Squamata: Gekkota) from Oman João P. Maia a,b,c,⁎, D. James Harris a,b, Salvador Carranza c a CIBIO Research Centre in Biodiversity and Genetic Resources, InBIO, Universidade do Porto, Campus Agrário de Vairão, Rua Padre Armando Quintas, N° 7, 4485-661 Vairão, Vila do Conde, Portugal b Departamento de Biologia, Faculdade de Ciências, Universidade do Porto, Rua do Campo Alegre FC4 4169-007 Porto, Portugal c Institut de Biologia Evolutiva (CSIC-Universitat Pompeu Fabra), Passeig Maritím de la Barceloneta, 37-49, 08003 Barcelona, Spain article info abstract Article history: The order Haemosporida (Apicomplexa) includes many medically important parasites. Knowledge on the diver- Received 4 April 2015 sity and distribution of Haemosporida has increased in recent years, but remains less known in reptiles and their Received in revised form 7 September 2015 taxonomy is still uncertain. Further, estimates of evolutionary relationships of this order tend to change when Accepted 10 September 2015 new genes, taxa, outgroups or alternative methodologies are used. We inferred an updated phylogeny for the Available online 12 September 2015 Cytochrome b gene (cyt b) of Haemosporida and screened a total of 80 blood smears from 17 lizard species from Oman belonging to 11 genera. The inclusion of previously underrepresented genera resulted in an alterna- Keywords: Haemoproteus tive estimate of phylogeny for Haemosporida based on the cyt b gene. -

Helminth Parasites (Trematoda, Cestoda, Nematoda, Acanthocephala) of Herpetofauna from Southeastern Oklahoma: New Host and Geographic Records
125 Helminth Parasites (Trematoda, Cestoda, Nematoda, Acanthocephala) of Herpetofauna from Southeastern Oklahoma: New Host and Geographic Records Chris T. McAllister Science and Mathematics Division, Eastern Oklahoma State College, Idabel, OK 74745 Charles R. Bursey Department of Biology, Pennsylvania State University-Shenango, Sharon, PA 16146 Matthew B. Connior Life Sciences, Northwest Arkansas Community College, Bentonville, AR 72712 Abstract: Between May 2013 and September 2015, two amphibian and eight reptilian species/ subspecies were collected from Atoka (n = 1) and McCurtain (n = 31) counties, Oklahoma, and examined for helminth parasites. Twelve helminths, including a monogenean, six digeneans, a cestode, three nematodes and two acanthocephalans was found to be infecting these hosts. We document nine new host and three new distributional records for these helminths. Although we provide new records, additional surveys are needed for some of the 257 species of amphibians and reptiles of the state, particularly those in the western and panhandle regions who remain to be examined for helminths. ©2015 Oklahoma Academy of Science Introduction Methods In the last two decades, several papers from Between May 2013 and September 2015, our laboratories have appeared in the literature 11 Sequoyah slimy salamander (Plethodon that has helped increase our knowledge of sequoyah), nine Blanchard’s cricket frog the helminth parasites of Oklahoma’s diverse (Acris blanchardii), two eastern cooter herpetofauna (McAllister and Bursey 2004, (Pseudemys concinna concinna), two common 2007, 2012; McAllister et al. 1995, 2002, snapping turtle (Chelydra serpentina), two 2005, 2010, 2011, 2013, 2014a, b, c; Bonett Mississippi mud turtle (Kinosternon subrubrum et al. 2011). However, there still remains a hippocrepis), two western cottonmouth lack of information on helminths of some of (Agkistrodon piscivorus leucostoma), one the 257 species of amphibians and reptiles southern black racer (Coluber constrictor of the state (Sievert and Sievert 2011). -

Dr. Donald L. Price Center for Parasite Repository and Education College of Public Health, University of South Florida
Dr. Donald L. Price Center For Parasite Repository and Education College of Public Health, University of South Florida PRESENTS Sources of Infective Stages and Modes of Transmission of Endoparasites Epidemiology is the branch of science that deals with the distribution and spread of disease. How diseases are transmitted, i.e. how they are passed from an infected individual to a susceptible one is a major consideration. Classifying and developing terminology for what takes place has been approached in a variety of ways usually related to specific disease entities such as viruses, bacteria, etc. The definitions that follow apply to those disease entities usually classified as endoparasites i.e. those parasites that reside in a body passage or tissue of the definitive host or in some cases the intermediate host. When the definition of terms for the “Source of Infection” or “Mode of Infection” relate to prevention and/or control of an endoparasitic disease, they should be clearly described. For the source of infection, the medium (water, soil, utensils, etc.) or the host organism (vector, or intermediate host) on which or in which the infective stage can be found should be precisely identified. For the mode of transmission, the precise circumstances and means by which the infective stage is able to come in contact with, enter, and initiate an infection in the host should be described. SOURCE OF INFECTION There are three quite distinct and importantly different kinds of sources of the infective stage of parasites: Contaminated Sources, Infested Sources, and Infected Sources. CONTAMINATE SOURCES Contaminated Source, in parasitology, implies something that has come in contact with raw feces and is thereby polluted with feces or organisms that were present in it. -

Opportunistic Mapping of Strongyloides Stercoralis and Hookworm in Dogs in Remote Australian Communities
pathogens Article Opportunistic Mapping of Strongyloides stercoralis and Hookworm in Dogs in Remote Australian Communities Meruyert Beknazarova 1,*, Harriet Whiley 1 , Rebecca Traub 2 and Kirstin Ross 1 1 Faculty of Science and Engineering, Flinders University, Bedford Park, SA 5042, Australia; harriet.whiley@flinders.edu.au (H.W.); kirstin.ross@flinders.edu.au (K.R.) 2 Faculty of Veterinary and Agricultural Sciences, University of Melbourne, Parkville, VIC 3052, Australia; [email protected] * Correspondence: meruyert.cooper@flinders.edu.au or [email protected] Received: 27 April 2020; Accepted: 19 May 2020; Published: 21 May 2020 Abstract: Both Strongyloides stercoralis and hookworms are common soil-transmitted helminths in remote Australian communities. In addition to infecting humans, S. stercoralis and some species of hookworms infect canids and therefore present both environmental and zoonotic sources of transmission to humans. Currently, there is limited information available on the prevalence of hookworms and S. stercoralis infections in dogs living in communities across the Northern Territory in Australia. In this study, 274 dog faecal samples and 11 faecal samples of unknown origin were collected from the environment and directly from animals across 27 remote communities in Northern and Central Australia. Samples were examined using real-time polymerase chain reaction (PCR) analysis for the presence of S. stercoralis and four hookworm species: Ancylostoma caninum, Ancylostoma ceylanicum, Ancylostoma braziliense and Uncinaria stenocephala. The prevalence of S. stercoralis in dogs was found to be 21.9% (60/274). A. caninum was the only hookworm detected in the dog samples, with a prevalence of 31.4% (86/274). This study provides an insight into the prevalence of S. -

A KEY to the COMMON PARASITIC PROTOZOANS of NORTH AMERICAN FISHES Thomas L. Wellborn, Jr. and Wilmer A. Rogers Zoology-Ent
. A KEY to the COMMON PARASITIC PROTOZOANS of NORTH AMERICAN FISHES Thomas L. Wellborn, Jr. and Wilmer A. Rogers Zoology-Entomology Department Series Fisheries No. 4 AGRICULTURAL EXPERIMENT STATION AUBURN UNIVERSITY E. V. Smith, Director March 1966 Auburn, Alabama (Revised June 1970) A KEY TO THE COMMON PARASITIC PROTOZOANS 1 OF NORTH AMERICAN FISHES Thomas L. Wellborn, Jr. 2/— and Wilmer A. Rogers 3/— Private, state, and federal fish husbandry industries suffer great losses each year because of disease and parasites. The parasitic protozoans included in this key are the ones most commonly associated with fish mortalities. A total of 23 genera of parasitic protozoans may be identified by use of this key. The fish protozoan parasites are responsible for a large part of the mortalities that occur at fish hatcheries each year. This is because they are capable of building up tremendous populations within relatively short periods of time, and some are capable of causing extreme damage to fish. Proper treatment and control of the diseases caused by the various protozoans are impossible without knowing their identity. This key will be helpful to fishery workers in identifying the more common genera. It must be remembered, however, that a microscope and knowledge of its use are absolute prerequisites for identifying protozoans. Certain parasitic protozoans cannot be identified below the rank of Order - without use of special techniques; therefore, all known genera are not included in the herein reported key. Protozoans belonging to such Orders should be sent to a specialist for identification. 1/ Supported in part by Southeastern Cooperative Fish Parasite and Disease Project (Fish Restoration Funds). -

Identity of Diphyllobothrium Spp. (Cestoda: Diphyllobothriidae) from Sea Lions and People Along the Pacific Coast of South America
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Faculty Publications from the Harold W. Manter Laboratory of Parasitology Parasitology, Harold W. Manter Laboratory of 4-2010 Identity of Diphyllobothrium spp. (Cestoda: Diphyllobothriidae) from Sea Lions and People along the Pacific Coast of South America Robert L. Rausch University of Washington, [email protected] Ann M. Adams United States Food and Drug Administration Leo Margolis Fisheries Research Board of Canada Follow this and additional works at: https://digitalcommons.unl.edu/parasitologyfacpubs Part of the Parasitology Commons Rausch, Robert L.; Adams, Ann M.; and Margolis, Leo, "Identity of Diphyllobothrium spp. (Cestoda: Diphyllobothriidae) from Sea Lions and People along the Pacific Coast of South America" (2010). Faculty Publications from the Harold W. Manter Laboratory of Parasitology. 498. https://digitalcommons.unl.edu/parasitologyfacpubs/498 This Article is brought to you for free and open access by the Parasitology, Harold W. Manter Laboratory of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Faculty Publications from the Harold W. Manter Laboratory of Parasitology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. J. Parasitol., 96(2), 2010, pp. 359–365 F American Society of Parasitologists 2010 IDENTITY OF DIPHYLLOBOTHRIUM SPP. (CESTODA: DIPHYLLOBOTHRIIDAE) FROM SEA LIONS AND PEOPLE ALONG THE PACIFIC COAST OF SOUTH AMERICA Robert L. Rausch, Ann M. Adams*, and Leo MargolisÀ Department of Comparative Medicine and Department of Pathobiology, Box 357190, University of Washington, Seattle, Washington 98195-7190. e-mail: [email protected] ABSTRACT: Host specificity evidently is not expressed by various species of Diphyllobothrium that occur typically in marine mammals, and people become infected occasionally when dietary customs favor ingestion of plerocercoids. -

Waterborne Zoonotic Helminthiases Suwannee Nithiuthaia,*, Malinee T
Veterinary Parasitology 126 (2004) 167–193 www.elsevier.com/locate/vetpar Review Waterborne zoonotic helminthiases Suwannee Nithiuthaia,*, Malinee T. Anantaphrutib, Jitra Waikagulb, Alvin Gajadharc aDepartment of Pathology, Faculty of Veterinary Science, Chulalongkorn University, Henri Dunant Road, Patumwan, Bangkok 10330, Thailand bDepartment of Helminthology, Faculty of Tropical Medicine, Mahidol University, Ratchawithi Road, Bangkok 10400, Thailand cCentre for Animal Parasitology, Canadian Food Inspection Agency, Saskatoon Laboratory, Saskatoon, Sask., Canada S7N 2R3 Abstract This review deals with waterborne zoonotic helminths, many of which are opportunistic parasites spreading directly from animals to man or man to animals through water that is either ingested or that contains forms capable of skin penetration. Disease severity ranges from being rapidly fatal to low- grade chronic infections that may be asymptomatic for many years. The most significant zoonotic waterborne helminthic diseases are either snail-mediated, copepod-mediated or transmitted by faecal-contaminated water. Snail-mediated helminthiases described here are caused by digenetic trematodes that undergo complex life cycles involving various species of aquatic snails. These diseases include schistosomiasis, cercarial dermatitis, fascioliasis and fasciolopsiasis. The primary copepod-mediated helminthiases are sparganosis, gnathostomiasis and dracunculiasis, and the major faecal-contaminated water helminthiases are cysticercosis, hydatid disease and larva migrans. Generally, only parasites whose infective stages can be transmitted directly by water are discussed in this article. Although many do not require a water environment in which to complete their life cycle, their infective stages can certainly be distributed and acquired directly through water. Transmission via the external environment is necessary for many helminth parasites, with water and faecal contamination being important considerations.