Medical Staff References
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Maryland Hospitals by County 2014
Maryland Hospital Association 2014 Member Hospitals by County 57 6 Allegany 43 Garrett 31 Cecil Washington Carroll 36 8 Harford Baltimore 54 46 12 Frederick 11 1340 34 53 23 Baltimore Kent Howard City 50 16 Montgomery 26 44 1 2 20 Queen 39 Anne Anne's 33 15 9 Arundel 3 42 56 32 24 37 Caroline 21 41 Prince George's Talbot 52 10 27 29 49 Calvert Baltimore City Charles 7 51 48 45 19 Dorchester 30 18 5 55 17 Wicomico 47 14 4 38 St. Mary's 28 35 25 Worcester Somerset Hospital Name Number Hospital Name Number Hospital Name Number 22 Adventist Behavioral Health 1 Levindale Hebrew Geriatric Center & Hospital 21 Sinai Hospital of Baltimore 41 Adventist Rehabilitation Hospital of Maryland 2 McCready Foundation 22 Suburban Hospital 42 Anne Arundel Medical Center 3 MedStar Franklin Square Medical Center 23 Union Hospital 43 Atlantic General Hospital 4 MedStar Good Samaritan Hospital 24 Univ of MD Baltimore Washington Medical Ctr 44 Bon Secours Baltimore Health System 5 MedStar Harbor Hospital 25 Univ of MD Charles Regional Medical Center 45 Univ of MD Harford Memorial Hospital 46 Brook Lane 6 MedStar Montgomery Medical Center 26 Calvert Memorial Hospital 7 MedStar Southern Maryland Hospital Center 27 University of Maryland Medical Center 47 Univ of MD Medical Center Midtown Campus 48 Carroll Hospital Center 8 MedStar St. Mary’s Hospital 28 Doctors Community Hospital 9 MedStar Union Memorial Hospital 29 Univ of MD Rehabilitation & Orthopaedic Inst 49 Fort Washington Center Medical Center 10 Mercy Medical Center 30 Univ of MD Shore Medical Ctr at Chestertown 5050 Frederick Regional Health System 11 Meritus Medical Center 31 Univ of MD Shore Medical Ctr at Dorchester 51 Garrett County Memorial Hospital 12 Mt. -

Maryland State Trauma Registry Data Dictionary for Adult Patients April 21
Maryland State Trauma Registry Data Dictionary for Adult Patients April 21, 2017 Maryland Institute for Emergency Medical Services Systems Richard Alcorta, M.D. F.A.C.E.P. Acting Co-Executive Director Patricia Gainer, J.D., M.P.A. Acting Co-Executive Director Melanie Gertner, B.S. Data Services Carole Mays, R.N., M.S., C.E.N. Trauma and Injury Specialty Care Program Cynthia Wright-Johnson, R.N., M.S.N. EMSC Program Maryland Designated Trauma Centers Trauma Program Managers Susie Burleson, R.N., B.S.N., M.S.N., M.B.A Meritus Medical Center Kari Cheezum, R.N., B.S.N., C.E.N. Peninsula Regional Medical Center Diana Clapp, R.N., C.C.R.N., B.S.N., N.R.P. R Adams Cowley Shock Trauma Center Marie Dieter, M.S.N., M.B.A., R.N., C.E.N. Johns Hopkins Bayview Medical Center Jen Fritzeen, M.S.N., R.N. Children's National Medical Center Melissa Meyers, R.N., B.S.N., C.E.N. Suburban Hospital - Johns Hopkins Medicine Dawn Moreland, B.S.N., R.N. Prince George’s Hospital Center Kathy Noll, M.S.N., R.N. Johns Hopkins Hospital Lauren Heinrich Smith, M.S., A.C.N.P. Sinai Hospital Sandy Waak, R.N., C.E.N., T.C.R.N. R Adams Cowley Shock Trauma Center Elizabeth Wooster, R.N., B.S.N., M.S., Ms.E.M. Western Maryland Regional Medical Center Susan Ziegfeld, C.C.R.N., M.S.N., C.P.N.P. Johns Hopkins Hospital Special Acknowledgements ` Daniel A. -
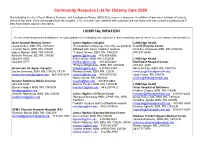
Community Resource List for Ostomy Care 2020
Community Resource List for Ostomy Care 2020 The following is a list of local Wound, Ostomy, and Continence Nurses (WOCN) to use as a resource. In addition, there are a number of ostomy clinics in the area. Once discharged from the hospital, LTC, or home care, patients with ostomies are not alone and can contact a professional if they have future ostomy care needs. HOSPITAL INPATIENT *Denotes that this particular facility/nurse accepts outpatient referrals/physician orders for treatment and your patient can be seen for ostomy related problems. Anne Arundel Medical Center Johns Hopkins Hospital LifeBridge Health Joyce Onken, BSN, RN, CWOCN (For outpatient follow-up, may only see patients Carroll Hospital Center Jennifer Davis, BSN, RN, CWON affiliated with Johns Hopkins Hospital) Christine Arrowood, BSN, RN, CWOCN Agnes Mpanja, BSN, RN, CWCN *Jessica Groom, BSN, RN, CWOCN 410-871-6839 Michelle Perkins, BS, RN, CWON [email protected] 410-955-6668 443-481-5508 Kelly Heffron, BSN, RN, CWOCN LifeBridge Health 443-481-5177 [email protected] 410-955-6647 Northwest Hospital Center *Frances Magliacane, BSN, RN, CWOCN 410-521-2200 Ascension St. Agnes Hospital [email protected] 410-955-5367 Missy McCoy, MSN, RN, CWOCN Sacha Simmons, BSN, RN, CWON, CFCN Rhonda Sewell, BSN, RN, COCN [email protected] [email protected] 667-234-3034 [email protected] 443-287-0392 Judy Coster, RN, CWCN Nancy Sujeta, RN, CWOCN [email protected] Greater Baltimore Medical Center [email protected] 410-955-6667 443-849-6992 Melissa Venker, BSN, -

2016 Annual Report
Alvin & Lois Lapidus Cancer Institute 2016 ANNUAL REPORT Alvin & Lois Lapidus Cancer Institute TABLE OF LETTER FROM THE CANCER COMMITTEE CHAIRWOMAN, ABBIE FIELDS, M.D. 1 CONTENTS CANCER LIAISON PHYSICIAN SUMMARY, DONA HOBART, M.D. 2 LETTER FROM MARVIN JACK FELDMAN, M.D. MEDICAL DIRECTOR 3 SINAI HOSPITAL OF BALTIMORE AND NORTHWEST HOSPITAL 4-5 A LifeBridge Health Center Commission On Cancer Program CANCER SERVICES AVAILABLE AT SINAI HOSPITAL 6 OF BALTIMORE AND NORTHWEST HOSPITAL ALVIN & LOIS LAPIDUS CANCER INSTITUTE 7 THE HERMAN & WALTER SAMUELSON BREAST CARE CENTER SINAI HOSPITAL OF BALTIMORE AND NORTHWEST HOSPITAL THE QUALITY MEASURES FOR BREAST CANCER DIAGNOSTICS AND TREATMENT 8-9 LUNG CANCER FACTS – Lung Screening Program 10 THE ROLE OF OUR PATHOLOGY TEAM 11 THE ROLE OF OUR DIAGNOSTIC RADIOLOGISTS 12 PSYCHOSOCIAL HEALTH AND THE CANCER PATIENT 13 COMPLEMENTARY HEALTH SERVICES 14 2016 PATIENT NAVIGATION PROGRAM ACTIVITIES / INITIATIVES 15 2016 PREVENTION, EDUCATION, COMMUNITY OUTREACH 16 AND SCREENING ACTIVITIES / INITIATIVES THE CANCER REGISTRY 17 THE NATIONAL CANCER DATABASE 18 2015 CANCER REGISTRY STATISTICAL YEAR 19-20 2016 CANCER COMMITTEE MEMBERS 21 LETTER The cancer program at the Alvin & Lois Lapidus Cancer Institute, caring for patients at both FROM THE Sinai and Northwest hospital, in Baltimore City and County, proudly entered into collaboration with the William E. Kahlert Regional Cancer Center at Carroll Hospital in Westminster, Md. CANCER This collaboration contributed to the LifeBridge Health cancer program obtaining status of Integrated Network Cancer Program (INCP) through the American College of Surgeons COMMITTEE Commission on Cancer. Through this network, we are able to offer cutting-edge, evidence- CHAIRWOMAN based cancer care to patients within their own community-based institutions. -

[email protected]
Number Refresher Training Names E-Mail Address Business Name County Zip Code Business Phone RPS0001 NEED REFRESHER David L. Barnes [email protected] MAPCB Baltimore 21022 (866)537-5340 RPS0002 NEED REFRESHER Lauretha Vargas [email protected] Phoenix Health Center Washington 21740 (240)420-0000 RPS0003 5/9/2019 LaToya Nkongolo [email protected] Nick's Place Prince George's 20705 (301)937-4356 RPS0004 NEED REFRESHER Almustaphael Al-Kahlil-Bey [email protected] Interdynamics Inc. Prince George's 20706 (301)306-4590 RPS0005 8/10/2018 Stacie Grogin [email protected] Phoenix Health Center Washington 21740 (240)420-0000 RPS0006 2/27/2019 Kheninh Daniels [email protected] Maryand Recovery Organizations Connecting Communities 21227 (410)522-2230 RPS0007 6/21/2019 Denise Marcell Camp [email protected] On our Own of Maryland, Inc. Baltimore 21227 (410)646-0262 x-26 RPS0008 RPS0009 RPS0010 RPS0011 2/27/2019 Monica A. Kirkpatrick [email protected] Mountain Manor Tx. Ctr. Frederick 21701 (301)662-1407 RPS0012 NEED REFRESHER Willie J. Wilson [email protected] Baltimore Crisis Response 21231 (410)433-5255 x-348 RPS0013 NEED REFRESHER Charles Williams [email protected] In & Out Program Prince George's 20748 (202)230-7992 RPS0014 NEED REFRESHER George Phillips [email protected] Anne Arundel County Dept. of Health Anne Arundel 21060 (410)222-0119 RPS0015 NEED REFRESHER Wayne Allen [email protected] State of Maryland 21501 (301)777-2346 RPS0016 NEED REFRESHER Debbie D. Andersen [email protected] On Our Own of Howard County Howard 21045 (410)772-7905 RPS0017 NEED REFRESHER Carolyn E. Miller [email protected] Baltimore County Bureau of Behavioral Health Baltimore 21212 (410)887-3828 RPS0018 2/27/2019 Lauren Elaine McCarthy [email protected] Mountain Manor Tx. -

Carroll Hospital's Clinical Decision Unit
JANUARY 2017 NONPROFIT ORG U.S. POSTAGE PAID WESTMINSTER, MD PERMIT NO. 348 SCOPE 200 Memorial Avenue Westminster, MD 21157 A PUBLICATION FOR THE MEDICAL STAFF OF CARROLL HOSPITAL CarrollHospitalCenter.org Physicians Message from President Leslie Simmons, R.N., F.A.C.H.E. of the Month As we near the halfway mark of fiscal year 2017, I wanted to remind everyone of our organization’s corporate goals and the essential role that you, as a member of our medical staff, play in helping us achieve them. Every year, we set goals for the organization to challenge ourselves to raise the bar and continue our focus on providing high quality care and the best patient experience. For FY17, the LifeBridge Health corporate goals for each hospital fall under the following categories: August 2016 • Appropriate Utilization — ensuring patients are receiving the right care in the right Melvin Yeshnik, M.D., setting and that they have the resources they need when they go home to prevent a OB/GYN readmission. • Patient Experience — improving customer service scores (Hospital Consumer Assessment of Healthcare Providers and Systems [HCAHPS] — or patients’ perceptions of their care). • Employee and Physician Engagement — finding ways to enhance our employees’ and physicians’ involvement in their departments, increase their satisfaction and make LifeBridge Health the best place to work and practice medicine. • Financial — accomplishing all of the above while meeting our financial targets. Based on our reimbursement model, the quality of care we provide can have a big impact on our finances. September 2016 Medical and Carroll Health Group Staff – Additions Douglas Weber, M.D., Our success in achieving these goals depends on every medical staff member and employee understanding his or emergency medicine Department of Diagnostic Wendy Miller, M.D. -

Economic Development Summary
Economic Development Summary Original Adjusted % Change % Change Actual Budget Budget Budget From From FY 16 FY 17 FY 17 FY 18 O ri g. FY 17 Adj. FY 17 Economic Development Administration $976,782 $914,760 $929,340 $966,250 5.63% 3.97% Business and Employment Resource Center 261,941 219,290 231,550 249,200 13.64% 7.62% ED Infrastructure and Investments 1,583,226 1,504,440 1,504,440 750,070 -50.14% -50.14% Farm Museum 1,045,671 939,590 952,890 962,040 2.39% 0.96% Tourism 214,245 295,900 297,510 307,150 3.80% 3.24% Total Economic Development $4,081,864 $3,873,980 $3,915,730 $3,234,710 -16.50% -17.39% Total Without Benefits $3,470,607 $3,573,550 $3,570,270 $2,887,470 -19.20% -19.12% FY 17 Adjusted Budget reflects a change in OPEB allocations. Mission and Goals The mission of the Department of Economic Development is to create a positive business environment to foster the growth and retention of resident companies and encourage the attraction of new industry. The purpose is to provide jobs for local residents, promote a healthy economy, and increase the industrial tax base to provide for government services. Goals include: Increase the commercial/industrial tax base Increase the number of quality jobs Support the development of new technology and the growth of resident industries Create an environment that fosters small business creation, sustainability, and growth Increase tourism in Carroll County and support the efforts of local tourism related businesses Assist Carroll County businesses with workforce development needs, and citizens in finding employment opportunities Highlights, Changes, and Useful Information Carroll County’s average annual unemployment rate for CY 2016 was 3.6%, an improvement from CY 2015 average of 4.4%. -

Map of MHA Member Hospitals by County
Maryland Hospital Association Member Hospitals by County WM BL Allegany UH Garrett Meritus Cecil Washington Carroll CH Harford Baltimore UMUC UMHM GRMC Frederick FRHS GBMC SPHS UMSJ NWH MSFS Baltimore Kent Howard City UMSC HCGH HCG MSM Montgomery UMBW AHPH UML AHSG Queen Anne Anne's NIH AAMC SH HCH DCH Arundel AHWA CNHS MWPH MSGS UMPG Caroline SHB Prince George's Talbot UMSE FWMC MSSM MSUM Calvert UMRO Baltimore City Charles CHMC UMSD UMMid KKI UMCR Dorchester Mercy JHH VA BSBH JHB Wicomico UMMC HSCR AGH SAH St. Mary's MSStM PRMC MSHH Worcester Somerset Hospital Name Hospital Name Hospital Name MCH Howard County General Hospital HCGH Sheppard Pratt Health System SPHS Adventist HealthCare Physical Health and Rehabilitation AHPH Johns Hopkins Bayview Medical Center JHB Sinai Hospital of Baltimore SHB Adventist HealthCare Shady Grove Medical Center AHSG The Johns Hopkins Hospital and Health System JHH Suburban Hospital SH Adventist HealthCare Washington Adventist Hospital AHWA Kennedy Krieger Institute KKI Union Hospital of Cecil County UH Anne Arundel Medical Center AAMC McCready Health MCH Univ of MD Baltimore Washington Medical Ctr UMBW Atlantic General Hospital AGH MedStar Franklin Square Medical Center MSFS Univ of MD Charles Regional Medical Center UMCR Bon Secours Baltimore Health System BSBH MedStar Good Samaritan Hospital MSGS Univ of MD Harford Memorial Hospital UMHM Independent Hospitals Brook Lane BL MedStar Harbor Hospital MSHH Univ of MD Laurel Regional Hospital UML CalvertHealth Medical Center CHMC MedStar Montgomery Medical Center MSM University of Maryland Medical Center UMMC Adventist HealthCare Carroll Hospital CH MedStar Southern Maryland Hospital Center MSSM Univ of MD Medical Center Midtown Campus UMMid Holy Cross Health Children’s National Health System CNHS MedStar St. -

Name Provtype Address Suite City County State Zip Phone
NAME PROVTYPE ADDRESS SUITE CITY COUNTY STATE ZIP PHONE Inpatient Intensive Outpatient Partial Residential Outpatient Hospital Program ACED-A Center for Eating Disorders PD 2401 Arlington Avenue South Birmingham JEFFERSON AL 35205 (205) 933-0041 X X Highlands Treatment Center, LLC PD 2807 Greystone Commerical Blvd. Suite 36 Birmingham SHELBY AL 35242 (205) 552-0417 X X Magnolia Creek, LLC RTF 645 Crenshaw Road Columbiana SHELBY AL 35051 (205) 678-4372 X X Flagstaff Medical Center HO 1200 North Beaver Street Flagstaff COCONINO AZ 86001 (928) 779-3366 X X Doorways, LLC IO 1825 East Northern Avenue Suite 200 Phoenix MARICOPA AZ 85020 (602) 997-2880 X North Valley Clinical Services IO 4414 North 19th Avenue Phoenix MARICOPA AZ 85015 (480) 661-1075 X Healthy Futures IO 8065 North 85th Way Scottsdale MARICOPA AZ 85258 (480) 451-8500 X North Valley Clinical Services IO 10575 North 114th Street Suite 109 Scottsdale MARICOPA AZ 85259 (480) 661-1075 X Rosewood Ranch PSH 950 West Elliot Road Suite 201 Tempe MARICOPA AZ 85284 (480) 303-0844 X X X Rosewood Ranch PD 20 East University Drive Suite 301 Tempe MARICOPA AZ 85281 (486) 303-0844 X X Desert Milagros, LLC IO 2561-2 East Fort Lowell Road Tucson PIMA AZ 85716 (520) 531-1040 X Desert Milagros, LLC IO 3438 North Country Club Road Tucson PIMA AZ 85716 (520) 531-1040 X Desert Star ARC, LLC IO 7493 North Oracle Road Suite 203 Tucson PIMA AZ 85704 (520) 638-6000 X Tucson Medical Center HO 5301 East Grant Road Tucson PIMA AZ 85712 (520) 327-5461 X X Rosewood Ranch PSH 36075 South Rincon Road Wickenburg YAVAPAI AZ 85390 (926) 684-9594 X X X Rosewood Ranch PSH 521 West Wickenburg Way Wickenburg MARICOPA AZ 85390 (928) 684-8981 X X X Rosewood Ranch PD 521 West Wickenburg Way Wickenburg MARICOPA AZ 85390 (928) 684-8951 X Monte Nido Vista RTF 28855 Lake Vista Drive Agoura Hills LOS ANGELES CA 91301 (818) 338-7890 X Cielo House IO 1200 Sixth Avenue Suite 201 Belmont SAN MATEO CA 94002 (650) 455-9242 X X Center for Discovery PD 8484 Wilshire Blvd. -

MAHSL Members 2013 Kristin Chapman Medical Library Medstar
Maryland Association of Health Sciences Librarians Members 2013 Item Type Other Publication Date 2013 Keywords Maryland Association of Health Sciences Librarians; Medical librarians Download date 02/10/2021 17:39:54 Item License https://creativecommons.org/licenses/by-nc-nd/4.0/ Link to Item http://hdl.handle.net/10713/5381 MAHSL Members 2013 Kristin Chapman P.J. Grier National Network of Libraries, Medical Library Southeastern/Atlantic Region 601 W. Medstar Franklin Square Medical Center Lombard Street Baltimore, MD 21201-1512 9000 Franklin Square Drive Phone: 410-706-2855 E-mail: Baltimore, MD 21237 [email protected] Phone: 443-777-7463 Fax: 410-687-1742 Patricia Hinegardner HS/HS Library E-mail: [email protected] University of Maryland, Baltimore 601 W. Lombard Street Darcie Cote-Rumsey Baltimore, MD 21201-1513 Health Sciences Library Phone: 410-706-8863 Northwest Hospital Email: [email protected] 5401 Old Court Road Randallstown, MD 21133 Andrea Lamb Medical Library St. Agnes Phone: 410-521-2200, x55682 Healthcare Hospital 900 Caton Avenue Fax: 410-496-7549 Baltimore, MD 21229 Phone: 410-368-3124 E-mail: [email protected] Email: [email protected] W. Lee Cook Eisenberg Medical Library Sinai Shirley Lay Hospital of Baltimore 2401 W. Belvedere Ave Health Sciences Library Baltimore, MD 21215 Phone: 410-601-5015 Med-Star Harbor Hospital Center Fax: 410-664-7432 E-mail: 3001 S. Hanover Street [email protected] Baltimore, MD 21225-1290 Phone: 410-350-3419 Meg Del Baglivo E-mail: [email protected] HS/HS Library University of Maryland, Baltimore Carole Lever 601 W. -

Annual Report FY 2009
Annual Report FY 2009 www.arccarroll.com 1 Mission To support people in their individual pursuit of a fulfilling life. Vision We are a leading organization that champions for and supports people with developmental disabilities, while cultivating relationships that enrich our community. Core Values Innovation – our founders pioneered the opportunities that exist today for people with developmental disabilities. We build on their courageous tradition of innovation and creativity in the design and delivery of our services. Integrity – we operate with integrity in all that we do – as a service provider, as an employer, and as members of our community. Respect – we treat everyone with respect. Dignity, choice, ability, privacy and opinion are fundamental principles of who we are. Quality – we embrace the highest standards in all that we do. Quality in service and character drives our actions and attitudes. Caring – we act with a genuine spirit of caring. A sincere interest in and concern for the complete well-being of all people define our actions. Strategic Priorities To achieve The Arc’s mission and vision, the following strategic priorities will be emphasized during this planning period: n Evaluate the individual program and service needs of those we serve. n Evaluate all tangible and intangible assets and develop strategies to manage and maximize those resources. n Enhance staff development through structured training, orientation and target recruiting for hard-to-fill positions. n Advance program quality through improved staff training, innovation and continual feedback. n Increase awareness of The Arc. n Develop and improve relationships and partnerships with all major stakeholders. n Assure sound fiscal management. -

COMMUNITY BENEFIT NARRATIVE REPORT FY2014 Community
COMMUNITY BENEFIT NARRATIVE REPORT FY2014 Community Benefit Reporting Carroll Hospital Center 200 Memorial Avenue Westminster, MD 21157 CarrollHospitalCenter.org Carroll Hospital Center FY2014 BACKGROUND The Health Services Cost Review Commission’s (HSCRC or Commission) Community Benefit Report, required under §19-303 of the Health General Article, Maryland Annotated Code, is the Commission’s method of implementing a law that addresses the growing interest in understanding the types and scope of community benefit activities conducted by Maryland’s nonprofit hospitals. The Commission’s response to its mandate to oversee the legislation was to establish a reporting system for hospitals to report their community benefits activities. The guidelines and inventory spreadsheet were guided, in part, by the VHA, CHA, and others’ community benefit reporting experience, and was then tailored to fit Maryland’s unique regulated environment. The narrative requirement is intended to strengthen and supplement the qualitative and quantitative information that hospitals have reported in the past. The narrative is focused on (1) the general demographics of the hospital community, (2) how hospitals determined the needs of the communities they serve, and (3) hospital community benefit administration. For the purposes of this report, the IRS defines a CHNA as a: Written document developed for a hospital facility that includes a description of the community served by the hospital facility: the process used to conduct the assessment including how the hospital took into account input from community members and public health experts; identification of any persons with whom the hospital has worked on the assessment; and the health needs identified through the assessment process.