PRANDIN® (Repaglinide) Tablets (1 Mg and 2 Mg) Rx Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

Medication Choice Diabetes
Weight Change Low Blood Sugar Blood Sugar Considerations (Hypoglycemia) Blood(A1c Reduction) Sugar Weight Change Low Blood Sugar (A1c Reduction) Considerations (Hypoglycemia) Metformin Metformin Metformin 1 – 2% Metformin In the rst few weeks after starting Metformin, patients may have some nausea, indigestion or diarrhea. None No Severe Risk Minor = 0 – 1% Insulin There are no other side effects associated with Insulin. Insulin Insulin Insulin Unlimited % Pioglitazone 4 to 6 lb. gain Over time, 10 in 100 people may have fluid retention Severe = 1 – 3% Minor = 30 – 40% (edema) while taking the drug. For some it may be as little as ankle swelling. For others, fluid may build up Pioglitazone 1% in the lungs making it difficult to breathe. This may Pioglitazone Pioglitazone resolve after you stop taking the drug. 10 in 100 people at risk of bone fractures who use this drug will have More than 2 to 6 lb. gain a bone fracture in the next 10 years. There appears to No Severe Risk Minor = 1 – 2% be a slight increase in the risk of bladder cancer with Liraglutide/ 0.5 – 1% this drug. Liraglutide/Exenatide Liraglutide/Exenatide Exenatide Liraglutide/Exenatide Some patients may have nausea or diarrhea. In some 3 to 6 lb. loss cases, the nausea may be severe enough that a patient No Severe Risk Minor = 0 – 1% has to stop taking the drug. There are reports of pain in the abdomen that may be caused by inammation Sulfonylureas Sulfonylureas Sulfonylureas 1 – 2% of the pancreas with these agents. Glipizide, Glimepiride, Glyburide Glipizide, Glimepiride, Glyburide Glipizide, Glimepiride, Glyburide Sulfonylureas 2 to 3 lb. -

Association Between Serious Hypoglycemia and Calcium-Channel Blockers Used Concomitantly with Insulin Secretagogues
Research Letter | Diabetes and Endocrinology Association Between Serious Hypoglycemia and Calcium-Channel Blockers Used Concomitantly With Insulin Secretagogues Young Hee Nam, PhD; Colleen M. Brensinger, MS; Warren B. Bilker, PhD; James H. Flory, MD; Charles E. Leonard, MSCE, PharmD; Sean Hennessy, PhD, PharmD Introduction + Supplemental content Serious hypoglycemia is a major, potentially fatal adverse event caused by insulin secretagogues.1 Author affiliations and article information are Previous case reports suggested that calcium-channel blockers (CCBs) might reduce the risk of listed at the end of this article. serious hypoglycemia in patients with hyperinsulinemic hypoglycemia.2,3 However, the association of serious hypoglycemia and CCBs used with insulin secretagogues has remained unclear. Because insulin secretion by the pancreas is mediated by calcium influx in beta cells through calcium channels,4 we conducted a population-based observational study on the hypothesis that concomitant use of CCBs may be associated with reduced rates of serious hypoglycemia in insulin secretagogue users. Methods This self-controlled case series study was approved by the institutional review board of the University of Pennsylvania, which waived the requirement for informed consent because the use or disclosure of the protected health information involved no more than minimal risk to the privacy of individuals, and the research could not practicably be conducted without the waiver or alteration and without access to and use of the protected health information. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. We used claims data from the Medicaid programs of 5 US states (California, Florida, New York, Ohio, and Pennsylvania, encompassing more than a third of the nationwide Medicaid population), supplemented with Medicare claims for dual enrollees, from January 1, 1999, to December 31, 2011, and used the self- controlled case series design. -

Sulfonylureas
Therapeutic Class Overview Sulfonylureas INTRODUCTION In the United States (US), diabetes mellitus affects more than 30 million people and is the 7th leading cause of death (Centers for Disease Control and Prevention [CDC] 2018). Type 2 diabetes mellitus (T2DM) is the most common form of diabetes and is characterized by elevated fasting and postprandial glucose concentrations (American Diabetes Association [ADA] 2019[a]). It is a chronic illness that requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications (ADA 2019[b]). ○ Complications of T2DM include hypertension, heart disease, stroke, vision loss, nephropathy, and neuropathy (ADA 2019[a]). In addition to dietary and lifestyle management, T2DM can be treated with insulin, one or more oral medications, or a combination of both. Many patients with T2DM will require combination therapy (Garber et al 2019). Classes of oral medications for the management of blood glucose levels in patients with T2DM focus on increasing insulin secretion, increasing insulin responsiveness, or both, decreasing the rate of carbohydrate absorption, decreasing the rate of hepatic glucose production, decreasing the rate of glucagon secretion, and blocking glucose reabsorption by the kidney (Garber et al 2019). Pharmacologic options for T2DM include sulfonylureas (SFUs), biguanides, thiazolidinediones (TZDs), meglitinides, alpha-glucosidase inhibitors, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) analogs, amylinomimetics, sodium-glucose cotransporter 2 (SGLT2) inhibitors, combination products, and insulin (Garber et al 2019). SFUs are the oldest of the oral antidiabetic medications, and all agents are available generically. The SFUs can be divided into 2 categories: first-generation and second-generation. -

New Therapeutic Agents Marketed in 2014: Part 1 Daniel A
CPE New therapeutic agents marketed in 2014: Part 1 Daniel A. Hussar Objective: To provide information regarding the most important properties of Daniel A. Hussar, PhD, is Remington Professor of Pharmacy, Philadelphia College new therapeutic agents that have been marketed in 2014. of Pharmacy, University of the Sciences in Data sources: Product labeling supplemented selectively with published studies Philadelphia. and drug information reference sources. Development: This home-study CPE activity Data synthesis: Seven new therapeutic agents that were marketed in the United was developed by the American Pharmacists States in early 2014 are considered in this first of a four-part series: umeclidinium Association. bromide/vilanterol trifenatate, perampanel, eslicarbazepine acetate, apremilast, dapagliflozin propanediol, avanafil, and bazedoxifene/conjugated estrogens. In- dications and information on dosage and administration for these agents are re- viewed, as are the most important pharmacokinetic properties, drug interactions, and other precautions. Practical considerations for use of these new agents are also discussed. When possible, properties of the new drugs are compared with those of older agents marketed for the same indications. Conclusion: Umeclidinium/vilanterol is the first combination formulation for oral inhalation to include both a long-acting muscarinic antagonist and a long-acting beta-2-adrenergic agonist for the maintenance treatment of patients with chronic ob- structive pulmonary disease. Both perampanel and eslicarbazepine have been ap- proved as adjunctive treatment for patients with partial-onset seizures. Perampanel has a unique mechanism of action whereas eslicarbazepine has properties that are most similar to those of oxcarbazepine. Apremilast is indicated for the treatment of patients with active psoriatic arthritis and is effective following oral administra- tion. -

Ambetter 90-Day-Maintenance Drug List- 2020
Ambetter 90-Day-Maintenance Drug List Guide to this list: What is Ambetter 90‐Day‐Maintenance Drug List? Ambetter 90‐Day‐Supply Maintenance Drug List is a list of maintenance medications that are available for 90 day supply through mail order or through our Extended Day Supply Network. How do I find a pharmacy that is participating in Extended Day Supply Network? To find a retail pharmacy that is participating in our Extended Day Supply Network please consult information available under Pharmacy Resources tab on our webpage. Alternatively, you can utilize our mail order pharmacy. Information on mail order pharmacy is available in Pharmacy Resources tab on our webpage. Are all formulary drugs covered for 90 day supply? No, certain specialty and non‐specialty drugs are excluded from 90 day supply. Please consult 90‐Day‐ Supply Maintenance Drug List for information if your drug is included. A Amitriptyline HCl Acamprosate Calcium Amlodipine Besylate Acarbose Amlodipine Besylate-Atorvastatin Calcium Acebutolol HCl Amlodipine Besylate-Benazepril HCl Acetazolamide Amlodipine Besylate-Olmesartan Medoxomil Albuterol Sulfate Amlodipine Besylate-Valsartan Alendronate Sodium Amlodipine-Valsartan-Hydrochlorothiazide Alendronate Sodium-Cholecalciferol Amoxapine Alfuzosin HCl Amphetamine-Dextroamphetamine Aliskiren Fumarate Anagrelide HCl Allopurinol Anastrozole Alogliptin Benzoate Apixaban Alosetron HCl Arformoterol Tartrate Amantadine HCl Aripiprazole Amiloride & Hydrochlorothiazide Armodafinil Amiloride HCl Asenapine Maleate Amiodarone HCl Aspirin-Dipyridamole -

Glucotrol XL (Glipizide) Tablets Label
® GLUCOTROL XL (glipizide) Extended Release Tablets For Oral Use DESCRIPTION Glipizide is an oral blood-glucose-lowering drug of the sulfonylurea class. The Chemical Abstracts name of glipizide is 1-cyclohexyl-3-[[p-[2-(5 methylpyrazinecarboxamido)ethyl] phenyl]sulfonyl]urea. The molecular formula is C21H27N5O4S; the molecular weight is 445.55; the structural formula is shown below: N H C 3 CONHCH CH SO NHCONH 2 2 2 N Glipizide is a whitish, odorless powder with a pKa of 5.9. It is insoluble in water and alcohols, but soluble in 0.1 N NaOH; it is freely soluble in dimethylformamide. GLUCOTROL XL® is a registered trademark for glipizide GITS. Glipizide GITS (Gastrointestinal Therapeutic System) is formulated as a once-a-day controlled release tablet for oral use and is designed to deliver 2.5, 5, or 10 mg of glipizide. Inert ingredients in the 2.5 mg, 5 mg and 10 mg formulations are: polyethylene oxide, hypromellose, magnesium stearate, sodium chloride, red ferric oxide, cellulose acetate, polyethylene glycol, Opadry® blue (OY-LS-20921)(2.5 mg tablets), Opadry® white (YS-2-7063)(5 mg and 10 mg tablet) and black ink (S-1-8106). System Components and Performance GLUCOTROL XL Extended Release Tablet is similar in appearance to a conventional tablet. It consists, however, of an osmotically active drug core surrounded by a semipermeable membrane. The core itself is divided into two layers: an “active” layer containing the drug, and a “push” layer containing pharmacologically inert (but osmotically active) components. The membrane surrounding the tablet is permeable to water but not to drug or osmotic excipients. -
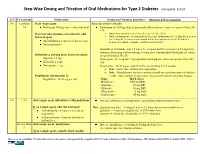
Step-Wise Dosing and Titration of Oral Medications for Type 2 Diabetes Last Update 5/3/10
Step-Wise Dosing and Titration of Oral Medications for Type 2 Diabetes last update 5/3/10 A1C S Creatinine Medications Dosing and Titration guidelines - (Recheck A1C in 3 months) 7-8 Less than Start single agent Increase every 1-2 weeks 1.4 Metformin 500 mg twice a day with food Metformin: by 500 mg daily if preprandial blood glucose values are greater than 130- 150. If on max tolerated dose of metformin, add o Note: slow titration is needed to decrease GI side effects 2nd oral agent o Note: metformin use is contraindicated in renal dysfunction (Scr>1.5mg/dL in men or Scr>1.4mg/dL in females) and should not be used in patients aged >80 unless a Add sulfonylurea (preferred due to cost) measured creatinine clearance is within normal limits. Add pioglitazone Glipizide or Glyburide: add 2.5 mg in the evening and then increase by 2.5 mg in the morning alternating with increasing evening dose if preprandial blood glucose values Sulfonylurea starting doses before breakfast: are greater than 130-150. Glipizide 2.5 mg Glimepiride: by 1 mg daily if preprandial blood glucose values are greater than 130- Glyburide 2.5 mg 150 Glimepiride 1 mg Pioglitazone : by 15 mg per day if A1C is greater than 7 in 3 months. o Note: slower dose titration for pioglitazone o Note: Rosiglitazone has been associated with increased incidence of adverse Pioglitazone starting dose is: events. (American Diabetes Association: Consensus 2009 and 2007 Black Box Warning) Pioglitazone 15-30 mg per day Name MAX doses Metformin - 1000 mg BID Glipizide - 20 mg BID Glyburide - -

ACCEPTABLE COMBINATIONS of DIABETES MEDICATIONS (Updated 01/27/2021)
ACCEPTABLE COMBINATIONS OF DIABETES MEDICATIONS (Updated 01/27/2021) The chart on the following page outlines acceptable combinations of medications for treatment of diabetes. Please note: • Initial certification of all applicants with diabetes mellitus (DM) requires FAA decision; • Use no more than one medication from each group (A-F); • Fixed-dose combination medications - count each component as an individual medication. (e.g., Avandamet [rosiglitazone + metformin] is considered 2-drug components); • Up to 3 medications total are considered acceptable for routine treatment according to generally accepted standards of care for diabetes (American Diabetes Association, American Association of Clinical Endocrinologists); • For applicants receiving complex care (e.g., 4-drug therapy), refer the case to AMCD; • For applicants on AASI for diabetes mellitus, follow the AASI; • Consult with FAA for any medications not on listed on the chart; • Observation times: When initiating NEW diabetes therapy using monotherapy or combination medications: Adding Medication Observation Time Group A ONLY 14 days Group B-D 30 days Group E1 60 days When ADDING a new medication to an ESTABLISHED TREATMENT regimen: Current Medication Adding Medication Observation Time on Group A-D + new Group A-D 14 days on Group E1 + new Group A-D 30 days on Group A-D + new Group E1 60 days Note: If transitioning between injectable GLP-1 RA and oral GLP-1 RA formulation = 72 hours When initiating NEW or ADDING therapy for any regimen (new or established therapy): Adding Medication Observation Time Group F (SGLT2 inhibitors) 90 days Group E2 (insulin): • For agency ATCSs (non-CGM or CGM protocol) 90 days • For Pilots / Part 67 applicants, class 3 non-CGM 90 days protocol only: 180 days • For Pilots / Part 67 applicants, any class CGM protocol: ACCEPTABLE COMBINATIONS OF DIABETES MEDICATIONS (Updated 01/27/2021) Biguanides A -metformin (e.g. -

Pharmaceutical Sciences
IAJPS 2018, 05 (05), 4758-4765 P.Sravani et al ISSN 2349-7750 CODEN [USA]: IAJPBB ISSN: 2349-7750 INDO AMERICAN JOURNAL OF PHARMACEUTICAL SCIENCES http://doi.org/10.5281/zenodo.1260873 Available online at: http://www.iajps.com Research Article PREPARATION AND CHARACTERIZATION OF ESLICARBAZEPINE ACETATE SOLID DISPERSION Sravani.P1*, B. Mounika1, P. Ganesh1, Md.Zeeshanuddin1, Y. Krishna reddy 1, A. Thangathirupathi 2 , K.Rajeswar Dutt 3 1 Department of Pharmaceutics, Nalanda college of pharmacy, Nalgonda, Telangana. 2 Department of Pharmacology, Nalanda college of Pharmacy, Nalgonda, Telangana. 3 Department of Pharmaceutical analysis, Nalanda college of pharmacy, Nalgonda, Telangana. Abstract Solubility is one of the important parameters to achieve desired concentration of drug in systemic circulation for achieving required pharmacological response. Poorly water soluble drugs often require high doses in order to reach therapeutic plasma concentrations after oral administration. Low aqueous solubility is the major problem encountered with formulation development of new chemical entities. Solid dispersion method has been widely employed to improve the dissolution rate, solubility and oral absorption of poorly water soluble drugs. Solid dispersion technology is the science of dispersing one or more active ingredients in an inert matrix in the solid stage in order to achieve increased dissolution rate.The present work is on study of solubility parameters of eslicarbazepine acetate and evaluate its dissolution rate. Key words: Inert matrix, Plasma concentrations, Solubility, Solid dispersion, Eslicarbazepine acetate. Corresponding Author: QR code P.Sravani, Department of Pharmaceutics, Nalanda College of Pharmacy, Nalgonda, Telangana. Email:[email protected] Please cite this article in press P.Sravani et al., Preparation and Characterization of Eslicarbazepine Acetate Solid Dispersion, Indo Am. -

Non-Insulin Antidiabetic Agents
NON-INSULIN ANTIDIABETIC AGENTS Slow onset of action Varied duration of action in different individuals Little flexibility, difficult to titrate in-house Long action (frequently 24 hour duration) } *** NOTE : many of the contraindications develop unexpectedly during acute illness. For this reason, general recommendation is to discontinue oral agents during hospitalization Non-insulin agents can be continued in stable patients, with normal nutritional intake, adequate BG control, stable renal and cardiac function. Generic and Class Brand name Contraindications/ Cautions side effects sulfonylureas Glimepiride Amaryl Contraindications: DKA, NPO status. Hypoglycemia, Glipizide Glucotrol Cautions: Risk of prolonged/ severe hypoglycemia if caloric intake weight gain, is reduced. Long action with varied duration of action in different potential Glyburide Diabeta individuals.Increased risk of hypoglycemia in renal or hepatic increased risk of Micronase impairment and elderly. Greatest benefit achieved at half maximum cardiovascular Glynase dose. Dose modification required with glimepiride and glyburide mortality due to renal elimination. Less pronounced effect with glipizide. Biguanides Metformin Glucophage Contraindications: 1) serum creatinine levels >1.5 mg/dL (males), GI symptoms Fortamet >1.4 mg/dL (females) 2) metabolic acidosis, including DKA. 3) For common: Glumetza studies involving iodinated contrast materials, discontinue at the diarrhea, Riomet (liquid time of or prior to the procedure, and withhold for 48 hours after nausea, formulation the procedure. Cautions: advanced age, excessive alcohol intake, flatulence, hepatic disease, hypoxemia, surgery. indigestion Thiazolidinediones (TZD’s) Pioglitazone Actos Contraindications: Heart failure NYHA Class III or IV. Cautions: Weight gain, Rosiglitazone Avandia Can increase intravascular volume, worsening edema or edema. See exacerbating HF. Do not use if baseline ALT >2.5X upper limit of literature re: risk normal or active liver disease. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.