Epidemiological Studies on Long Distance Cross-Country Skiers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Russians Are the Fastest in Marathon Cross-Country Skiing: the (Engadin Ski Marathon)
Hindawi BioMed Research International Volume 2017, Article ID 9821757, 7 pages https://doi.org/10.1155/2017/9821757 Research Article The Russians Are the Fastest in Marathon Cross-Country Skiing: The (Engadin Ski Marathon) Pantelis Theodoros Nikolaidis,1,2 Jan Heller,3 and Beat Knechtle4,5 1 Exercise Physiology Laboratory, Nikaia, Greece 2Faculty of Health Sciences, Metropolitan College, Athens, Greece 3Faculty of Physical Education and Sport, Charles University, Prague, Czech Republic 4Gesundheitszentrum St. Gallen, St. Gallen, Switzerland 5Institute of Primary Care, University of Zurich, Zurich, Switzerland Correspondence should be addressed to Beat Knechtle; [email protected] Received 20 April 2017; Accepted 17 July 2017; Published 21 August 2017 Academic Editor: Laura Guidetti Copyright © 2017 Pantelis Theodoros Nikolaidis et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. It is well known that athletes from a specific region or country are dominating certain sports disciplines such as marathon running or Ironman triathlon; however, little relevant information exists on cross-country skiing. Therefore, the aim of the present study was to investigate the aspect of region and nationality in one of the largest cross-country skiing marathons in Europe, the “Engadin Ski Marathon.” All athletes ( = 197,125) who finished the “Engadin Ski Marathon” between 1998 and 2016 were considered. More than two-thirds of the finishers (72.5% in women and 69.6% in men) were Swiss skiers, followed by German, Italian, and French athletes in both sexes. Most of the Swiss finishers were from Canton of Zurich (20.5%), Grisons (19.2%), and Berne (10.3%). -

37. Forum Nordicum 3 Deine Belohnung
3 7. Forum Nordicum 11. – 14.10.2016 www.lahti2017.fi/en/de Biathlon-König Martin Fourcade bei der Ehrung durch Rolf Arne Odiin. Rolf-Arne Odin honors Biathlon-King Martin Fourcade. (Foto: FN) Dein Sport. Deine Belohnung. 100% Leistung. 100% Regeneration. Durch das enthaltene wertvolle Vitamin B12 wird der Energiestoffwechsel, die Blutbildung und das Immunsystem gefördert sowie die Müdigkeit verringert. Eine abwechslungsreiche und ausgewogene Ernährung sowie eine gesunde Lebensweise sind wichtig! GREEtiNG Dein Sport. Janne Leskinen CEO, Secretary General Lahti2017 FiS Nordic World 37. Forum Nordicum 3 Deine Belohnung. Ski Championships Lahti will host the Nordic World Ski Championships in 2017 for a historic seventh time. We are extremely proud to be the first city to achieve this record. To celebrate our unique history, we decided to name the event the Centenary Championships. The Centenary Championships are both an exciting and carefully prepared world-class sports event and one of the festivities that celebrate the centenary of Finland’s independence. A rare occasion for us Finns – and hopefully for our international guests. Lahti offers an optimal setting for record-breaking performances. The traditional venue has undergone extensive renovation and is now a fully functioning stadium that meets today’s requirements. We are also proud to have Vierumäki Olympic Training Center as our athlete’s village that allows the athletes to unwind and focus all their energy on performing at their best. We hope that the 2017 World Championships will leave their mark on future decades of sports events in Lahti and in Finland. The event has gained a great deal of popularity among young people, and we will soon have a new generation of volunteers for sports events. -

Birkebeinerrennet Dag Har Start Vært På Sykkel Avlyses Pga
THANK YOU SHARE KNOWLEGDE ONE FAMILY OF SKIING LILLEHAMMER = VINTERSPORTS NATURAL – HISTORY - PASSION - EXPERIENCE THE DREAM AND GOAL OF THE REGION 3. TIME WINTER OLYMIC GAMES IN GENERAL SUCCSESS IN SPORTEVENTS GOOD SPORT GOOD EVENT STRUCTURE AND IMPLEMENTATION GOOD EXPERIENCE FOR ALL CLIENT GROUPS THE REGION WISHES WELCOME SO EASY…. BIRKEN – FOR EVERYONE – from 6 - 93 Utfordringer og opplevelser for alle Hovedpunkter: • Organisation • History • Events • Focus • Sponsors • Brand • Success criteria Utfordringer og opplevelser for alle Birken AS VISION • ”Birken – CHALLENGE AND EXPERIENCE FOR ALL VALUES • HAPINESS • QUALITY • TOGETHER Birken AS • OWNERS – LILLEHAMMER SKIKLUB – LILLEHAMMER CYCLE CLUB – RENA SPORTS CLUB • 25 EVENTS EVERY YEAR • 50.000 TAKE PART EVERY YEAR • 15 EMPOYEES • 50 KEY VOULENTEERS • 6000 VOULENTEERS • TURNOVER 80 000 000 NOK • MEMBER IN WORLDLOPPET AND CO-OWNER IN SKICLASSICS DL Jo Gunnar Informasjonsansvarlig Randi B Sportssjef Arena og logistikksjef Administrasjon og Markedssjef økonomisjef Sølvi Tor Liv Olaf Kunde ansvarlig Arr. Koordinator/ Camilla Lager Controller Ansv Magasin lederstøtte Rena Leif Tony Frøydis Terje Randi K Kunde koordinator Redaktør Arr. Koordinator/ Nina kontoransvarlig Logistikk medarbeider Øk medarbeider 70% Elise Lillehammer XX Berit 80% Christin Sponsor ansvarlig Ingunn Magasin Irene IKT ansvarlig Anne Lise Markedskoordinator Kjersti Prosjekt utlendinger Jean Utfordringer og opplevelser for alle History THE YEAR 1205 ON SKIS TWO BIRKEBEINERE, SOLDIERS, BRINGS THE KINGS CHILD FROM LILLEHAMMER TO RENA, OVER THE MOUNTAIN, INTO SAFENESS, IN STORMY WEATHER. THE CHILD, HÅKON HÅKONSSØN, WILL LATER BE THE MOST IMPORTANT KING IN THE HISTORY OF NORWAY. THE BIRKEBEINERE CREATED HISTORY – ON SKIS THE IDEA TO BIRKEBENERRENNET AND THE OTHER EVENTS ARE BASED ON THIS HEROIC FEAT FROM 155 MEN TO A MOVEMENT FROM LOCAL TO INTERNATIONAL Utfordringer og opplevelser for alle FROM 1932 - 2016 1991 2008 1948 Fra 1991 og frem til i FredagsBirken Birkebeinerrennet dag har start vært på sykkel avlyses pga. -

Climate Change Sensitivity and Adaptation of Cross-Country Skiing in Northern Europe
UNIVERSITY OF COPENHAGEN FACULTY OF SCIENCE Photo: Magnus Östh, Visma Ski Classics MSc in Climate Change Erik Söderström Climate Change sensitivity and adaptation of cross-country skiing in Northern Europe Main supervisor Anne Busk Gravholt and co-supervisor Nina Lintzén Submitted: 08/08/2016 Institute: Faculty of Science Name of department: Department of Geosciences and Natural Resource Management Author: Erik Söderström Title: Climate Chance sensitivity and adaptation of cross-country skiing in Northern Europe Description: A survey-based study investigating how climate change has affected and will affect cross-country skiing among ski areas in Northern Europe. Main supervisor: Anne Busk Gravholt Co-supervisor: Nina Lintzén Submitted: 08/08/2016 2 Abstract ............................................................................................................................................... 4 Abbreviations .................................................................................................................................... 4 Introduction ........................................................................................................................................ 4 Background ........................................................................................................................................ 5 Importance of winter sport in general ............................................................................ 5 Importance of cross-country skiing ................................................................................. -

PF 2021 Lipně Na Míru
zima 2020/21 Catering na PF 2021 Lipně na míru. To je Relax! zahradní party svatební catering grilování & barbecue rodinné oslavy firemní akce mikrocatering degustace Vážení a milí čtenáři, přečkali jsme druhou vlnu koronavirové pan- Je před námi zimní sezóna a je pravda, že demie. Život se s námi nemazlí, ale běží dál. A i to, nikdo z nás neví, co a kdy nám přinese třetí vlna že držíte v rukou tento další díl časopisu Lipensko, koronavirové epidemie. Ale ať už přinese cokoli, je toho důkazem. Běžíme dál a pořád nás to baví. my tady budeme i po ní. Proto více než kdy jindy Baví nás dělat vám radost, baví nás, když vás vám všem přeji krásné Vánoce v kruhu rodinném, bavíme, baví nás, když se necháváte inspirovat šťastný Nový rok 2021 a pevné zdraví v celém našimi stránkami, naší lipenskou přírodou, naší roce 2021. nabídkou pro trávení volného času, pro čerpání A víte co? Tím správným krokem ke zdraví zážitků a skvělých pocitů. v roce 2021 může být třeba otužování v Lipně. Ve Zimní Lipensko je tu pro vás, pro běžkaře, skvělé partě kamarádů v ledové vodě s kulichem na výletníky, sjezdaře, bruslaře, gurmány a požitkáře. hlavě a s horkým nápojem v ruce. I o tom se dočtete Ale především pro lipenské obyvatele, protože v tomto časopise. Ale pozor! I nadále nás sledujte, Lipensko je skvělá adresa pro život. protože něco, o čem ještě nepíšeme, se chystá… Za celou redakci a Turistický spolek Lipenska Jiří Mánek Dolní Vltavice 44, 382 26 Černá v Pošumaví www.HotelResortRelax.cz +420 601 367 508 [email protected] hrr_lipensko_175x250.indd 1 -

2019 Results Birken Ski Festival Download
Birken_A4_Skifestival_5mm_utfallende.pdf 1 16.11.2018 10.21 RESULTATER 2019 s mar . 16 - . 09 PROGRAM 09.03 INGALÅMI 5, 15 og 30 km 10.03 BARNEBIRKEN SKI 1, 2,5 og 3,5 km UNGDOMSBIRKEN SKI 15 km 15.03 TURBIRKEN SKI 27 km TURBIRKEN SKI 54 km SKØYTEBIRKEN SKI 54 km STAFETTBIRKEN SKI 4 x 7,5 km 16.03 BIRKEBEINERRENNET 54 km For tr eningstips, mer informasjon og påmelding: www.birkebeiner.no STATISTIKK Birkebeinerrennet 2019 Birkebeinerrennet 2019 Puljevis Klasse Påmeldt Startet % Fullført % Merker % SMK GMK SST Krus GST FAT 25 MED 30 FAT 35 FAT 40 FAT 45 Klasse Påmeldt Startet % Fullført % Merker % SMK GMK SST Krus GST FAT 25 MED 30 FAT 35 FAT 40 FAT 45 Kvinner funksj.h. 3 2 67 % 2 100 % 2 100 % 1 0 0 0 0 0 0 0 0 0 Elite kvinner 117 106 91 % 103 103 24 9 3 1 0 0 0 0 0 0 Elite kvinner 117 106 91 % 103 97 % 103 100 % 24 9 3 1 0 0 0 0 0 0 Elite Menn 293 272 93 % 264 264 47 34 4 5 1 0 0 0 0 0 Kvinner 16-17 år 33 30 91 % 30 100 % 19 63 % 15 0 0 0 0 0 0 0 0 0 1 239 222 93 % 220 99 % 220 100 % 28 16 8 5 1 0 2 0 0 0 Kvinner 18-19 år 48 46 96 % 45 98 % 32 71 % 18 0 0 0 0 0 0 0 0 0 101 ( menn 70 år+, Kvinner 20-24 år 136 125 92 % 122 98 % 49 40 % 23 7 0 0 0 0 0 0 0 0 kvinner 65 år+ og FH) 387 333 86 % 320 96 % 132 41 % 19 2 2 5 1 4 3 5 1 1 Kvinner 25-29 år 267 253 95 % 246 97 % 95 39 % 39 5 0 0 0 0 0 0 0 0 2 356 344 97 % 341 99 % 337 99 % 47 23 10 7 6 0 3 0 0 0 Kvinner 30-34 år 173 158 91 % 155 98 % 52 34 % 20 4 0 0 0 0 0 0 0 0 Pulje 2-KE2 124 118 95 % 116 98 % 115 99 % 28 7 1 2 0 0 0 0 0 0 Kvinner 35-39 år 117 107 91 % 106 99 % 41 39 % 17 2 0 0 0 -

Cross Country Marathon Calender 2018 / 2019 Date Race Location Country Distance Additionals Serie Homepage
Cross Country Marathon Calender 2018 / 2019 date race location country distance additionals serie homepage Sa. 24.11.18 Kiilopäähiihto Saariselkä / Kiilopää FIN 50 / 20 CL www.suomenlatu.fi/tapahtumia/kiilopaahiihto/uutiset.html Sa. 01.12.18 Sgambeda Livigno ITA 30 FT www.lasgambeda.it So. 16.12.18 Kannelberglauf Hermsdorf D 20 CL www.sportverein-hermsdorf.de Sa. 29.12.18 Rymmarloppet Arvidsjaur SWE 40 CL www.skidor.com Mo. 31.12.18 Silvesterlanglauf Kössen AUT 22 FT www.nordic-center.com So. 30.12.18 Risouxloppet St. Lupicin / Jura FRA 25 / 10 FT www.skiclub-saintlupicin.jimdo.com Fr. 04.01.18 China Vasalauf Changchun CHN 50 / 25 CL 1 www.vasaloppetchina.com Fr. 04.01.19 Bedrichovska Night LM Bedrichov / Liberec CZE 30 / 17 FT www.ski-tour.cz Sa. 05.01.19 Bedrichovska Night LM Bedrichov / Liberec CZE 30 / 17 CL www.ski-tour.cz Sa. 05.01.19 Budorrennet Loten NOR 46 CL www.kondis.no Sa. 05.01.19 Nordic Ski Marathon Bruksvallarna SWE 42 / 21 CL www.skidor.com So. 06.01.19 Attraverso Campra Olivione CH 21 FT 10 www.swissloppet.com So. 06.01.19 Base Tuono Marathon Passo Coe / Folgaria ITA 30 FT www.gronlait.it So. 06.01.19 La Ronde des Cimes Les Fourgs / Jura FRA 30 / 10 FT www.marathonskitour.fr So. 06.01.19 Alpe D'Huez Marathon Alpe D'Huez Oisans FRA 30 FT www.ffs.fr So. 06.01.19 AXA Skimarathon Sagmyra SWE 42 / 21 CL www.skidor.com Fr./So. 11.-13.1.19 Tour de Ramsau Ramsau / Dachstein AUT Sa. -

The Effect of Sex and Performance Level on Pacing in Cross-Country Skiers: Vasaloppet 2004‐2017
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2018 The effect of sex and performance level on pacing in cross-country skiers: Vasaloppet 2004‐2017 Nikolaidis, Pantelis Theodoros ; Villiger, Elias ; Knechtle, Beat Abstract: Background Pacing, defined as percentage changes of speed between successive splits, hasbeen extensively studied in running and cycling endurance sports; however, less information about the trends in change of speed during cross-country (XC) ski racing is available. Therefore, the aim of the present study was to examine the effect of performance (quartiles of race time (Q), with Q1 the fastest andQ4 the slowest) level on pacing in the Vasaloppet ski race, the largest XC skiing race in the world. Methods For this purpose, we analyzed female (n = 19,465) and male (n = 164,454) finishers in the Vasaloppet ski race from 2004 to 2017 using a 1-way (2 gender) analysis of variance with repeated measures to examine percentage changes of speed between 2 successive splits. Overall, the race consisted of 8 splits. Results The race speed of Q1, Q2, Q3, and Q4 was 13.6 ± 1.8, 10.6 ± 0.5, 9.2 ± 0.3, and 8.1 ± 0.4km/h, respectively, among females and 16.7 ± 1.7, 13.1 ± 0.7, 10.9 ± 0.6, and 8.9 ± 0.7km/h, respectively, among males. The overall pacing strategy of finishers was variable. A small sex × split interaction on speed was observed (2 = 0.016, p < 0.001), with speed difference between sexes ranging from 14.9% (Split 7) to 27.0% (Split 1) and larger changes in speed between 2 successive splits being shown for females (p < 0.001, 2 = 0.004). -
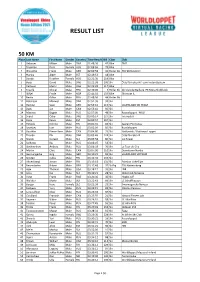
Home Edition 2021 Result List.Xlsx
RESULT LIST 50 KM Place Last Name First Name Gender Country Time Result BIB Class Club 1 Gebauer Mikael Male SWE 01:48:36 47 Bike TMT 2 Trueman Doris Female AUS 02:08:04 79 Bike 3 Wünsche Frank Male GER 02:09:58 41 Roller Ski TSV 90 Neukirch 4 Närska Alger Male EST 02:19:53 18 Bike 5 Bundy Heather Female AUS 02:22:30 119 Bike 6 Boija David Male SWE 02:22:38 100 Ski Österfärnebo IF/Team InstantSystem 7 Carlsson Martin Male SWE 02:23:28 117 Bike 8 Traullé Olivier Male FRA 02:40:00 9 Roller Ski Ski Club de Beille & IFK Mora Skidklubb 9 Stifjell Frode Male NOR 02:44:02 103 Bike Skorovas IL 10 Bertin Gilles Male FRA 02:48:56 44 Roller Ski 11 Robinson Maxwell Male SWE 02:51:36 39 Ski 12 Herling Sven Male GER 02:53:16 115 Ski SAUERLAND SKI TEAM 13 Basta Jan Male CAN 02:53:44 92 Ski 14 Маслов Вадим Male RUS 02:57:00 48 Ski Russialoppet - MSU 15 Svärd Oskar Male SWE 03:00:14 127 Ski Tvärreds IF 16 Kiple Kaivo Male EST 03:00:57 107 Ski 17 Pohjola Kimmo Male FIN 03:01:31 82 Ski Saaren Ponnistus 18 Savelyev Ivan Male RUS 03:02:09 85 Ski Russialoppet 19 Gauthier Pierre-Yves Male CAN 03:04:00 25 Ski Nakkertok / Gatineau Loppet 20 Thorén Pär Male SWE 03:05:46 124 Ski Österfärnebo IF 21 Slivnik Gorazd Male SLO 03:05:58 86 Ski Ice Power 22 Soldatov Ilya Male RUS 03:06:07 54 Ski 23 Ovchinnikov Andrey Male RUS 03:06:39 76 Ski Le Tour de Chiz 24 Martin Chris Male CAN 03:07:00 110 Ski Downtown Nordic 25 Gerstengarbe Jörg Male GER 03:10:21 93 Ski SAUERLAND SKITEAM 26 Sjösten Jukka Male FIN 03:12:40 135 Ski 27 Ahvenlampi Anton Male FIN 03:13:18 131 Ski Paimion -

Prediction of Performance in Vasaloppet Through Long Lasting Ski-Ergometer and Roller-Ski Tests in Cross-Country Skiers
Mygind et al. Int J Sports Exerc Med 2015, 1:4 ISSN: 2469-5718 International Journal of Sports and Exercise Medicine Original Article: Open Access Prediction of Performance in Vasaloppet through Long Lasting Ski- Ergometer and Rollerski Tests in Cross-Country Skiers Erik Mygind1*, Kristian Wulff1, Mads Rosenkilde Larsen2 and Jørn Wulff Helge2 1Department of Nutrition, Exercise and Sports, University of Copenhagen, Denmark 2Department of Biomedical Sciences, University of Copenhagen, Denmark *Corresponding author: Erik Mygind, Associate Professor, Department of Nutrition, Exercise and Sports, University of Copenhagen, Nørre Alle 51, 2200, Copenhagen N, Denmark, Tel: +45 28 75 08 94, E-mail: [email protected] • The distance in ski-ergometer tests improved significantly Abstract from 18.0 ± 0.6 to 19.2 ± 0.7 km/h from pre to post after three The main purpose was to investigate if long lasting cross-country months training (c-c) test procedures could predict performance time in ‘Vasaloppet’ • A long lasting (120 minutes) Rollerski test was significantly and secondly the effect of a 16 weeks training period on a 90 min double poling performance test. 24 moderate trained c-c skiers associated with racing time in Vasaloppet pre (r = 0.78) and participated in the study and completed Vasaloppet. All skiers post (r = 0.82) three months training period carried out pre and post training tests in a 90 minutes ski-ergometer • The total body fat percentage was significantly reduced, while double poling test and a 120 minutes rollerski field test on a closed paved circuit. 19 skiers provided detailed training logs that could trunk and total lean body mass increased significantly (P < 0.05). -

Combi Package with the Finlandia Hiihto and the Vasaloppet
Combi package with the Finlandia Hiihto and the Vasaloppet 25.02.-08.03.2021 With Full guiding by the Team of Sandoz Concept The Worldloppet calendar for 2021 provides you with the possibility of combing two legendary races in one trip! You can sign up to do the Finlandia Hiihto in Finland and then the Vasaloppet in Sweden. The trip starts in the city of Lahti 100 km to the north of Helsinki. Even today, it is considered a paradise for sports, in particular cross-country skiing and ski jumping. Since 1926, Lahti has wel- comed seven world cross-country ski championships. It is exactly in its world famous stadium at the foot of the three legendary ski jumps that the start and the finish of the largest marathon in Finland occurs every winter. In 2021 they Nordic skiiers will compete on the 27th and 28th of Feb- ruary. The first part of the marathon course is the most difficult because the course is the same course used for the cross-country world championships. The second part of the course is flatter (but of course this term is quite subjective), before the race finishes in the stadium surrounded by the three ski jumps. You have the possibility of either a 65 km, 32 km or 20 km classic race on Saturday and a 65 km, 32 km and 20 km skating race on Sunday. More than 6,000 skiers will participate in the two courses over the two days. The trip follows to Sweden with the most popular and oldest cross-country ski course in the his- tory of classic Nordic skiing: the Vasaloppet. -

2016 Resultat Birken Skifestival Last
RESULTATER 2016 • Birkebeinerrennet 19. mars • FredagsBirken ski 18. mars • StafettBirken 18. mars • HalvBirken ski 13. mars • UngdomsBirken ski 13. mars • Ingalåmi 15 km 12. mars • Ingalåmi 30 km 12. mars FRedAgSBIRKen SKI KLASSE PÅMELDT STARTET FULLFØRT Kvinner 16-39 år 116 108 104 Kvinner 40 år -> 201 184 172 Menn 16-39 år 223 206 203 Menn 40 år -> 588 537 517 Uten tid 30 26 26 SUM 1158 1061 1022 Resultathefte for Birken skifestival FRedAgSBIRKen SKI - pUljevIS PULJE PÅMELDT STARTET FULLFØRT 2016 1 317 284 279 2 309 293 282 3 264 233 227 Utgiver: 4 268 250 233 Birkebeinerrennet AS SUM 1158 1060 1021 Tlf. 41 77 29 00 Opplag: Distribueres elektronisk StafeTTBIRKen SKI Produksjon: KLASSE PÅMELDT STARTET FULLFØRT Masse Media AS Stafett funksjonshemmet 6 6 5 Stafett Kvinner 18 18 18 Alle foto: Stafett Menn 117 114 109 Geir Olsen Stafett Mix 78 70 70 SUM 219 208 202 STATISTIKK BIRKeBeIneRRenneT 2016 BIRKeBeIneRRenneT - pUljevIS KLASSE PÅMELDT STARTET FULLFØRT MERKER SMK GMK SST KRUS GST FAT 25 MED 30 FAT 35 FAT 40 FAT 45 KLASSE PÅMELDT STARTET FULLFØRT MERKER SMK GML SST KRUS GST FAT 25 MED 30 FAT 35 FAT 40 FAT 45 Kvinner FH 4 4 3 3 1 0 0 0 0 0 0 0 0 0 101 ( menn 70 år+, Elite kvinner 80 72 71 71 23 6 1 1 1 0 0 0 0 0 kvinner 65 år+ og FH) 387 310 294 158 15 4 7 4 6 5 9 1 1 1 Kvinner 16-17 år 48 45 44 38 32 0 0 0 0 0 0 0 0 0 Elite kvinner 80 72 71 71 23 6 1 1 1 0 0 0 0 0 Kvinner 18-19 år 43 39 38 25 14 0 0 0 0 0 0 0 0 0 Elite Menn 211 191 184 184 41 10 1 1 0 0 0 0 0 0 Kvinner 20-24 år 147 132 124 66 25 3 0 0 0 0 0 0 0 0 1 261 246 241 239