Iatrogenic Ocular Surface Diseases Occurring During And/Or After Different Treatments for Ocular Tumours
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Powerpoint Slides
AANP Teaching Rounds: Fausto J. Rodriguez MD Director, Clinical Neuropathology Service Professor of Pathology, Oncology and Ophthalmology Johns Hopkins University School of Medicine Disclosures • I have no relevant financial relationships to disclose Learning Objectives • Learning Objective #1: Outline the differential diagnosis of tumors of the ocular surface • Learning Objective #2: Recognize the spectrum of ocular infections relevant to ophthalmic pathology • Learning Objective #3: Recognize the morphologic features of the most common keratopathies and dystrophies Case 1 • 60-year-old woman with past medical history of hypertension, GERD, Atrial fibrillation and DVT • Autopsy: acute pulmonary hemorrhage, aortopulmonary fistula, and aortic dissection • No clinical history of eye disease Findings • Fuchs Dystrophy • Fuchs Adenoma Case 1 Fuchs Endothelial Corneal Dystrophy • Most common corneal dystrophy in the US • Corneal edema in ~5th-6th decade of life • Primary defect in corneal endothelium • Relatively easy clinical and pathologic diagnosis • PAS stain very useful in equivocal cases Fuchs adenoma • Benign tumor possibly developing from non-pigmented ciliary epithelium • Age related • Typically incidental at autopsy, but may rarely cause iris protrusion, shallowing of anterior chamber or glaucoma Case 2 • 54-year-old man with visual loss Masson Trichrome PAS Congo Red Case 2 Granular Corneal Dystrophy • Visual loss late in life • May recur in grafts after transplantation • Autosomal dominant inheritance • Transforming growth factor -

Optic Nerve Invasion of Uveal Melanoma: Clinical Characteristics and Metastatic Pattern
Optic Nerve Invasion of Uveal Melanoma: Clinical Characteristics and Metastatic Pattern Jens Lindegaard,1,2 Peter Isager,3,4 Jan Ulrik Prause,1,2 and Steffen Heegaard1 PURPOSE. To determine the frequency of optic nerve invasion in present independently of decreased visual acuity and tumor uveal melanoma, to identify clinical factors associated with location. (Invest Ophthalmol Vis Sci. 2006;47:3268–3275) optic nerve invasion, and to analyze the metastatic pattern and DOI:10.1167/iovs.05-1435 the association with survival. METHODS. All iris, ciliary body, and choroidal melanomas (N ϭ veal melanoma is the most frequent primary intraocular 2758) examined between 1942 and 2001 at the Eye Pathology Umalignant tumor in adults; in Scandinavia, the incidence 1–4 Institute, University of Copenhagen, Denmark, and the Insti- rate is 5.3 to 8.7 per million person-years. The tumor has a tute of Pathology, Aarhus University Hospital, Aarhus, Den- great propensity to metastasize and to affect the liver in par- 3,5,6 mark, were reviewed. Cases with optic nerve invasion were ticular. Local spread occurs through the overlying Bruch identified and subdivided into prelaminar or laminar invasion membrane, giving access to the subretinal space, or toward the and postlaminar invasion. Clinical characteristics were com- orbit (through the sclera, most often along ciliary vessels and pared with those from 85 cases randomly drawn from all ciliary nerves). Uveal melanoma infiltrates the optic nerve in only body and choroidal melanomas without optic nerve invasion 0.6% to 5% of patients and has been associated with high intraocular pressure, non–spindle cell type, juxtapapillary lo- from the same period. -

The Role of Combined Therapy in the Treatment of Retinopathy and Optic Neuropathy Due to Radiotherapy in the Uveal Melanoma
Published online: 2020-01-16 THIEME Original Article 1 The Role of Combined Therapy in the Treatment of Retinopathy and Optic Neuropathy Due to Radiotherapy in the Uveal Melanoma Yasemin Benderli Cihan1 1Department of Radiation Oncology, Kayseri Education and Address for correspondence Yasemin Benderli Cihan, MD, Department Research Hospital, Kayseri, Turkey of Radiation Oncology, Kayseri Education and Research Hospital, Sanayi District, Ataturk Boulevard, Hastane Street, No 78, 38010 Kocasinan, Kayseri, Turkey (e-mail: [email protected]). Asian J Oncol 2020;6:1–2 Abstract Introduction Uveal melanoma has a relatively low incidence. Transpupillary thermo- therapy (TTT), hypofractioned stereotactic radiotherapy (RT), stereotactic radiosur- gery, plaque brachytherapy, charged particle radiation therapy, local tumor resection, enucleation, and exantation are applied in the treatment. Methods The importance given to radiotherapy has increased to get more satisfac- tory results while treating the patient. However, it is the treatment of radiation reti- nopathy and optic neuropathy from complications. Results Radiation retinopathy and optic neuropathy are the most important compli- Keywords cations related to radiotherapy in the treatment of uveal melanoma. In recent years, ► uveal melanoma many studies have been performed on the treatment of radiation retinopathy and ► radiotherapy optic neuropathy. ► retinopathy Conclusion The consecutive use of triamcinolone in combination with anti-VEGF ► optic neuropathy supports that it may be a future therapeutic agent in the treatment of complications. Introduction was found to be 81.6%.2 The 2-, 5-, and 10-year metastasis rates were reported to be 10%, 25%, and 34%, respectively, regardless Uveal melanoma is the most common primary intraocular of tumor size.3 tumor in adults. -

Icare Eye Hospital Rate List 2015
ICARE EYE HOSPITAL & POST GRADUATE INSTITUTE E-3A, Sector – 26, Noida – 201301 Tel:- 0120-2477600 / 02, Counselor: 0120-2477621 Fax: 0120-2556389 / Appointments: 9811880015 Email: [email protected] / Web: www.icarehospital.org ICARE EYE HOSPITAL RATE LIST 2015 S No. PARTICULAR TARIFF (₹) I CONSULTATION NEW PATIENT VALID FOR 7 DAYS (FIRST TIME CONSULTATION : REGISTRATION + 1 ₹ 600/- CONSULTATION) 2 REVIEW CONSULTATION VALID FOR 7 DAYS ₹ 500/- 3 EMERGENCY CONSULTATION FOR 7 DAYS ₹ 800/- 4 LOW VISUAL AIDS ASSESSMENT CHARGES ₹ 600/- 5 VISION THERAPY CHARGES FOR PER SITTING ₹ 200/- 6 COST OF VISION THERAPY SOFTWARE (CD) ₹ 6,000/- 7 AMBLYOPIA (CD) ₹ 4,000/- II INVESTIGATIONS 1 Digital F.F.A (Fundus Fluoroscein Angiography)(Inclusive of Fundus photo) ₹ 2,500/- 2 Colour Fundus Photo - Digital ₹ 600/- 3 Colour Slit-lamp photo ₹ 600/- 4 Duplicate color prints (FFA/OCT/CLINICAL PHOTO) ₹ 300/- 5 Orthoptic ₹ 250/- 6 OCT (Optical Coherence Tomography) ₹ 2,500/- A Repeat OCT (within 2 months) with printout ₹ 800/- B Anterior Segment OCT ₹ 2,500/- 7 Ultrasonography (U/S) A A Scan – Single Eye ₹ 600/- B B Scan – Single Eye ₹ 1,000/- C UBM - Single Eye ₹ 1,500/- 8 Computerized field analysis A Humphrey Visual Fields (HVF) both eyes ₹ 1,500/- B Humphrey Visual Fields (HVF) One eye ₹ 750/- 9 Diurnal Variation of Tension (Day DVT ) A 5 times tension (Done in both eyes)] ₹ 500/- Page 1 10 Pachymetry (Both eyes) A Ultrasound (Central Corneal Thickness- CST) ₹ 600/- B Optical ₹ 600/- 11 Corneal Topography A Single Eye ₹ 1,000/- B Both Eyes ₹ 2,000/- 12 -

Local Coverage Determination (LCD): Diagnostic Evaluation and Medical Management of Moderate-Severe Dry Eye Disease (DED) (L36232)
Local Coverage Determination (LCD): Diagnostic Evaluation and Medical Management of Moderate-Severe Dry Eye Disease (DED) (L36232) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT NUMBER JURISDICTION STATE(S) First Coast Service Options, Inc. A and B MAC 09101 - MAC A J - N Florida First Coast Service Options, Inc. A and B MAC 09102 - MAC B J - N Florida First Coast Service Options, Inc. A and B MAC 09201 - MAC A J - N Puerto Rico Virgin Islands First Coast Service Options, Inc. A and B MAC 09202 - MAC B J - N Puerto Rico First Coast Service Options, Inc. A and B MAC 09302 - MAC B J - N Virgin Islands LCD Information Document Information LCD ID Original Effective Date L36232 For services performed on or after 11/22/2015 LCD Title Revision Effective Date Diagnostic Evaluation and Medical Management of For services performed on or after 01/08/2019 Moderate-Severe Dry Eye Disease (DED) Revision Ending Date Proposed LCD in Comment Period N/A N/A Retirement Date Source Proposed LCD N/A DL36232 Notice Period Start Date AMA CPT / ADA CDT / AHA NUBC Copyright 10/08/2015 Statement CPT codes, descriptions and other data only are Notice Period End Date copyright 2019 American Medical Association. All Rights 11/22/2015 Reserved. Applicable FARS/HHSARS apply. Current Dental Terminology © 2019 American Dental Association. All rights reserved. Copyright © 2019, the American Hospital Association, Created on 01/02/2020. Page 1 of 12 Chicago, Illinois. -

Small Choroidal Melanoma with All Eight Risk Factors for Growth
RETINAL ONCOLOGY CASE REPORTS IN OCULAR ONCOLOGY SECTION EDITOR: CAROL L. SHIELDS, MD Small Choroidal Melanoma With All Eight Risk Factors for Growth BY FELINA V. ZOLOTAREV, BA; KIRAN TURAKA, MD; AND CAROL L. SHIELDS, MD veal melanoma prognosis is A B C dependent on several factors including tumor size, location, U configuration, extraocular extension, cell type, and cytogenetic abnormalities. In general, the smaller the tumor, the better the prognosis.1 In a recent publication on 8,033 eyes with DE uveal melanoma, it was documented that increasing thickness of uveal melanoma was associated with greater risk for metastasis and ultimate death.1 Patients with uveal melanoma measuring 2.5 mm Figure 1. Features of small choroidal melanoma. A pigmented choroidal tumor thickness showed metastasis in 12% at 10 superior to the macula displays orange pigment, seen on autofluorescence (A, years as compared with 26% for those at B), hollowness on ultrasonography (C), and subretinal fluid, depicted on opti- 4.5 mm thickness.1 Hence, early detection cal coherence tomography (D, E). Note the lack of drusen or halo.These fea- of uveal melanoma is important. tures are most consistent with melanoma. The dilemma of early recognition cen- ters on the difficulty in differentiating a benign melanoma display two or three of these factors.2 In this choroidal nevus from a small malignant melanoma. Risk case presentation, we describe a small melanoma with factors for identification of small melanoma, when it all eight risk factors and discuss the importance of early might resemble choroidal nevus, have been identified detection of uveal melanoma. -

The Uveo-Meningeal Syndromes
ORIGINAL ARTICLE The Uveo-Meningeal Syndromes Paul W. Brazis, MD,* Michael Stewart, MD,* and Andrew G. Lee, MD† main clinical features being a meningitis or meningoenceph- Background: The uveo-meningeal syndromes are a group of disorders that share involvement of the uvea, retina, and meninges. alitis associated with uveitis. The meningeal involvement is Review Summary: We review the clinical manifestations of uveitis often chronic and may cause cranial neuropathies, polyra- and describe the infectious, inflammatory, and neoplastic conditions diculopathies, and hydrocephalus. In this review we define associated with the uveo-meningeal syndrome. and describe the clinical manifestations of different types of Conclusions: Inflammatory or autoimmune diseases are probably uveitis and discuss the individual entities most often associ- the most common clinically recognized causes of true uveo-menin- ated with the uveo-meningeal syndrome. We review the geal syndromes. These entities often cause inflammation of various distinctive signs in specific causes for uveo-meningeal dis- tissues in the body, including ocular structures and the meninges (eg, ease and discuss our evaluation of these patients. Wegener granulomatosis, sarcoidosis, Behc¸et disease, Vogt-Koy- anagi-Harada syndrome, and acute posterior multifocal placoid pig- ment epitheliopathy). The association of an infectious uveitis with an acute or chronic meningoencephalitis is unusual but occasionally the eye examination may suggest an infectious etiology or even a The uveo-meningeal syndromes are a specific organism responsible for a meningeal syndrome. One should consider the diagnosis of primary ocular-CNS lymphoma in heterogeneous group of disorders that share patients 40 years of age or older with bilateral uveitis, especially involvement of the uvea, retina, and meninges. -
Case Report Comment
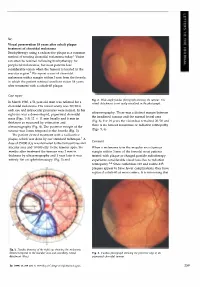
Sir, Visual preservation 18 years after cobalt plaque treatment of choroidal melanoma Brachytherapy using a radioactive plaque is a common method of treating choroidal melanoma today.l Vision can often be retained following brachytherapy for peripheral melanomas, but most patients lose considerable vision when the tumour is located in the macular region.2 We report a case of choroidal melanoma with a margin within 3 mm from the foveola in which the patient retained excellent vision 18 years after treatment with a cobalt-60 plaque. Case report Fig. 2. Wide-angle fundus photograph showing the tumour. The In March 1980, a 51-year-old man was referred for a retinal detachment is not easily visualised in the photograph. choroidal melanoma. His visual acuity was 20/20 in each eye and intraocular pressures were normal. In his ultrasonography. There was a distinct margin between right eye was a dome-shaped, pigmented choroidal the irradiated tumour and the normal foveal area mass (Figs. 1-3) 12 X 11 mm basally and 6 mm in (Fig. 6). For 18 years the vision has remained 20/20 and thickness as measured by estimation and there is no tumour recurrence or radiation retinopathy ultrasonography (Fig. 4). The posterior margin of the (Figs. 5, 6). tumour was 3 mm temporal to the foveola (Fig. 3). The patient elected treatment with a radioactive plaque, which was done by our standard technique. 1 A Comment dose of 35 000 cGy was delivered to the tumour base and macular area and 10 000 cGy to the tumour apex. Six When a melanoma is in the macular area (tumour months after treatment the tumour was 2 mm in margin within 3 mm of the foveola) most patients thickness by ultrasonography and 1 year later it was treated with plaque or charged particle radiotherapy entirely flat on ophthalmoscopy (Fig. -

Ocular Involvement in AIDS
Eye (1988) 2,496-505 Ocular Involvement in AIDS ALLAN E. KREIGER, and GARY N. HOLLAND, Los Angeles, USA The acquired immunodeficiency syndrome roaneurysms, and intraretinal microvascular (AIDS) is no longer a rare disease afflicting abnormalities. Autopsy studies of AIDS only a small segment of the world popula patients indicate that capillary changes in the tion. It has been recognised to occur in most retina are almost always present. These countries of the world; and, as of October, include swelling of endothelial cells, thicken 1987, there had been over 1000 cases ing of the basal lamina, degeneration and loss reported in the United Kingdom. I Despite of pericytes, and narrowing of capillary scientific determination of the causitive lumens. IS The pathogenetic mechanisms agent, better understanding of the behind these changes are not known, how pathogenesis of the clinical disease, and ever HIV has recently been shown to be pre clarification of the risk factors involved, the sent in retinal tissue. IS Viral (HIV-l) antigen epidemic continues to spread. As physicians, was found in the internal and external nuc we are destined to have to deal with the rav lear layers and the external plexiform layer as ages of AIDS increasingly in the future. well as in the capillary endothelial cells. Pos The first case reports of what became sibly, the endothelial infection results in known as AIDS appeared in 1981.2 Ophthal capillary alterations and occlusions. Another mic lesions were noted in the UCLA patients possibility is the deposition of circulating from the very beginning; they were reported immune complexes, which have arisen from by Holland and his associates in 1982.3 Since systemic infections, in the retinal capillaries. -

Uveal Melanoma-Derived Extracellular Vesicles Display Transforming Potential and Carry Protein Cargo Involved in Metastatic Niche Preparation
cancers Article Uveal Melanoma-Derived Extracellular Vesicles Display Transforming Potential and Carry Protein Cargo Involved in Metastatic Niche Preparation Thupten Tsering 1, Alexander Laskaris 1, Mohamed Abdouh 1 , Prisca Bustamante 1 , Sabrina Parent 1 , Eva Jin 1, Sarah Tadhg Ferrier 1, Goffredo Arena 1,2,3 and Julia V. Burnier 1,4,* 1 Cancer Research Program, Research Institute of the McGill University Health Centre, 1001 Decarie Blvd, Montreal, QC H4A 3J1, Canada; [email protected] (T.T.); [email protected] (A.L.); [email protected] (M.A.); [email protected] (P.B.); [email protected] (S.P.); [email protected] (E.J.); [email protected] (S.T.F.); goff[email protected] (G.A.) 2 Ospedale Giuseppe Giglio Fondazione San Raffaele Cefalu Sicily, 90015 Cefalu, Italy 3 Mediterranean Institute of Oncology, 95029 Viagrande, Italy 4 Experimental Pathology Unit, Department of Pathology, McGill University, QC H3A 2B4, Canada * Correspondence: [email protected]; Tel.: +1-514-934-1934 (ext. 76307) Received: 13 September 2020; Accepted: 7 October 2020; Published: 11 October 2020 Simple Summary: Uveal melanoma is a rare but deadly cancer that shows remarkable metastatic tropism to the liver. Extracellular vesicles (EVs) are nanometer-sized, lipid bilayer-membraned particles that are released from cells. In our study we used EVs derived from primary normal choroidal melanocytes and matched primary and metastatic uveal melanoma cell lines from a patient. Analysis of these EVs revealed important protein signatures that may be involved in tumorigenesis and metastatic dissemination. We have established a model to study EV functions and phenotypes which can be used in EV-based liquid biopsy. -

Cataract Surgery
Cataract surgery From Wikipedia, the free encyclopedia Jump to: navigation, search This article includes a list of references, related reading or external links, but its sources remain unclear because it lacks inline citations. Please improve this article by introducing more precise citations. (May 2011) Cataract surgery Intervention Cataract in Human Eye- Magnified view seen on examination with a slit lamp ICD-9-CM 13.19 MeSH D002387 Cataract surgery is the removal of the natural lens of the eye (also called "crystalline lens") that has developed an opacification, which is referred to as a cataract. Metabolic changes of the crystalline lens fibers over time lead to the development of the cataract and loss of transparency, causing impairment or loss of vision. Many patients' first symptoms are strong glare from lights and small light sources at night, along with reduced acuity at low light levels. During cataract surgery, a patient's cloudy natural lens is removed and replaced with a synthetic lens to restore the lens's transparency.[1] Following surgical removal of the natural lens, an artificial intraocular lens implant is inserted (eye surgeons say that the lens is "implanted"). Cataract surgery is generally performed by an ophthalmologist (eye surgeon) in an ambulatory (rather than inpatient) setting, in a surgical center or hospital, using local anesthesia (either topical, peribulbar, or retrobulbar), usually causing little or no discomfort to the patient. Well over 90% of operations are successful in restoring useful vision, with a low complication rate.[2] Day care, high volume, minimally invasive, small incision phacoemulsification with quick post-op recovery has become the standard of care in cataract surgery all over the world. -

Fixing Patients' Problems
CAN TABLETS WORK FOR EMR? P. 12 • CODING TIPS FOR CROSS-LINKING P. 16 A FRESH ANGLE ON RESIDENT TRAINING P. 68 • SIXTH CRANIAL NERVE DYSFUNCTION IN KIDS P. 72 Review of Ophthalmology Vol. XXIV, No. 4 • April 2017 • Fighting for Patient Care • Avoiding Problems Using OCT • Managing Refractive Surprises Problems • Optical Biometry Roundup Care • Avoiding No. 4 • April 2017 • Fighting for Patient Review of Ophthalmology Vol. XXIV, STEM THE TIDE OF EXCESSIVE TEARING P. 76 • POST-INJECTION IOP SPIKES P. 96 April 2017 reviewofophthalmology.com Fixing Patients’ Problems Expert surgeons give you the tools you need to succeed. ALSO INSIDE: Sizing Up Optical Biometers P. 58 001_rp0417_fc-WB.indd 1 3/24/17 12:52 PM VISIT US AT ASCRS BOOTH #1022 It’s all in CHOOSE A SYSTEM THAT EMPOWERS YOUR EVERY MOVE. Technique is more than just the motions. Purposefully engineered for exceptional versatility and high-quality performance, the WHITESTAR SIGNATURE® PRO Phacoemulsification System gives you the clinical flexibility, confidence and control to free your focus for what matters most in each procedure. How do you phaco? Join the conversation at WWW.ABBOTTPHACO.COM Rx Only INDICATIONS: The WHITESTAR SIGNATURE® PRO System is a modular ophthalmic microsurgical system that facilitates anterior segment (cataract) surgery. The modular design allows the users to configure the system to meet their surgical requirements. IMPORTANT SAFETY INFORMATION: Risks and complications of cataract surgery may include broken ocular capsule or corneal burn. This device is only to be used by a trained, licensed physician. ATTENTION: Reference the labeling for a complete listing of Indications and Important Safety Information.