Japanese Hepatitis C Market Forecast: Methodology and Implications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
UNO Template
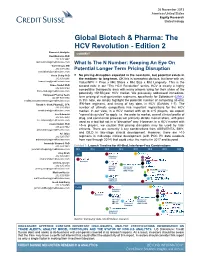
26 November 2013 Americas/United States Equity Research Biotechnology Global Biotech & Pharma: The HCV Revolution - Edition 2 Research Analysts COMMENT Ravi Mehrotra PhD 212 325 3487 [email protected] What Is The N Number: Keeping An Eye On Vamil Divan, MD 212 538 5394 Potential Longer Term Pricing Disruption [email protected] Koon Ching PhD ■ No pricing disruption expected in the near-term, but potential exists in 212 325 6286 the medium- to long-term. OK this is somewhat obvious, but bear with us: [email protected] Value/NPV = Price x Mkt Share x Mkt Size x Mkt Longevity. This is the Bruce Nudell PhD second note in our "The HCV Revolution" series. HCV is clearly a highly 212 325 9122 competitive therapeutic area with many players vying for their share of the [email protected] potentially >$15B/year HCV market. We previously addressed immediate- European Pharma Team 44 207 888 0304 term pricing of next-generation regimens, specifically for Sofosbuvir (LINK). [email protected] In this note, we simply highlight the potential number of competing all-oral, Ronak H. Shah, Pharm.D., CFA IFN-free regimens, and timing of key data, in HCV (Exhibits 1-7). The 212 325 9799 number of ultimate competitors has important implications for the HCV [email protected] market. In our view, in a HCV market with up to 4−5 players, we expect Lee Kalowski "normal drug rules" to apply: i.e. the order to market, overall clinical profile of 212 325 9683 drug, and commercial prowess will primarily dictate market share, with price [email protected] used as a tool but not in a "disruptive" way. -
IPI Template @Std Layout
立妥威 TM 膠囊 100 毫克 RETROVIR TM Capsules 100 mg 衛署藥輸字第 016120 號 立妥威 TM 膠囊 250 毫克 RETROVIR TM Capsules 250 mg 衛署藥輸字第 021443 號 TM 立妥威 溶液劑 RETROVIR TM Syrup 衛署藥輸字第 022014 號 定性與定量組成 膠囊含 100 毫克或 250 毫克 zidovudine - 為一有白色不透明膠囊帽,和中央有一深藍色條紋膠囊體之硬膠囊劑,其上印有 "Wellcome","100" 和 "Y9C" 字樣。 - 為一有白色不透明膠囊帽,和中央有一深藍色條紋膠囊體之硬膠囊劑,其上印有 "Wellcome","250" 和 "H2F" 字樣。 立妥威溶液劑 清澈,微黃色,草莓香味,不含糖的內服液劑,每 5 ml 含 zidovudine 50 mg。包裝內附 有一支 10 ml 口服劑量唧筒,使用前應將其安裝在藥瓶上,並用所附之瓶蓋蓋緊。 劑型 硬膠囊劑 口服溶液劑 臨床特性 【適應症】 後天性免疫缺乏症候群(AIDS)或與其有關之症狀(ARC, AIDS related complex);受到人類 3 免疫缺乏病毒(HIV)感染沒有症狀或只有初期輕度症狀而 CD4T 淋巴球數目小於 500/mm 病人的治療。 【說明】 RETROVIR 口服製劑適用於治療遭受人體免疫缺乏病毒(HIV)感染,卻沒有症狀,或具有 早期 HIV 相關症狀的患者。 RETROVIR 口服製劑亦適用於治療惡化 HIV 疾病患者,諸如患有後天性免疫缺乏症候群 (AIDS)或與 AIDS 相關的症狀(ARC)。 RETROVIR 口服製劑適用於治療遭受人體免疫缺乏病毒(HIV)感染,具有 HIV 相關症狀; 或無症狀,但標記卻顯示有顯著 HIV 相關免疫抑制現象的兒童。 以現有的資料為基礎,來評估用藥的利弊顯示,早期治療是有必要的。 惡化 HIV 感染的合併療法 治療惡化 HIV 感染(CD4+細胞數目< 300/mm3)時,可考慮併用 HIVID。RETROVIR 單一 療法仍適合作為符合核准適應症的 HIV 感染成人患者的起始治療。 【劑量與用法】 本藥須由醫師處方使用 宜由治療 HIV 感染有經驗的醫師,進行 RETROVIR 治療。 成人 雖然曾被使用的劑量範圍很寬廣,但一般使用劑量為一天 500 或 600 mg,分 3-5 次服用。 此外,一天 1000 mg,分 2 (或 4)次服用也有效。低劑量用於治療或預防與 HIV 相關的神 經官能異常及惡性病之有效性仍未知。 惡化 HIV 感染之合併療法劑量 每隔 8 小時同時服用 RETROVIR 200 mg 以及 HIVID 0.75 mg (RETROVIR 的每日總劑量為 600 mg,HIVID 的每日總劑量為 2.25 mg)。 兒童 三個月以上兒童的建議起始劑量為每隔 6 小時服用 180 mg/m2 體表面積(每日 720 mg/m2)。最大劑量不可超過每 6 小時 200 mg。 最適當的劑量仍待確定,且因人而異。劑量範圍一般為每 6 小時給予 120-180 mg/m2 體表 面積(即每日 480-720 mg/m2)。低劑量用於治療或預防與 HIV 相關的神經官能異常及惡性 病之有效性仍未知。對兒童而言,少次給藥的有效性仍待確立。 發生血液不良反應患者之劑量調整 發生血液不良反應患者可能需要調整劑量。在治療前已有骨髓儲存不良的患者,尤其是 有惡化 HIV 疾病的患者較容易出現血液不良反應。如果血紅素值降至 7.5-9 g/dl (4.65-5.59 mmol/l),或嗜中性白血球數降至 -

Annex I Summary of Product Characteristics
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 4 1. NAME OF THE MEDICINAL PRODUCT VISTIDE 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains cidofovir equivalent to 375 mg/5 ml (75 mg/ml) cidofovir anhydrous. The formulation is adjusted to pH 7.4. 3. PHARMACEUTICAL FORM Concentrate for solution for infusion 4. CLINICAL PARTICULARS 4.1 Therapeutic Indication Cidofovir is indicated for the treatment of CMV retinitis in patients with acquired immunodeficiency syndrome (AIDS) and without renal dysfunction. Until further experience is gained, cidofovir should be used only when other agents are considered unsuitable. 4.2 Posology and Method of Administration Before each administration of cidofovir, serum creatinine and urine protein levels should be investigated. The recommended dosage, frequency, or infusion rate must not be exceeded. Cidofovir must be diluted in 100 milliliters 0.9% (normal) saline prior to administration. To minimise potential nephrotoxicity, oral probenecid and intravenous saline prehydration must be administered with each cidofovir infusion. Dosage in Adults • Induction Treatment. The recommended dose of cidofovir is 5 mg/kg body weight (given as an intravenous infusion at a constant rate over 1 hr) administered once weekly for two consecutive weeks. • Maintenance Treatment. Beginning two weeks after the completion of induction treatment, the recommended maintenance dose of cidofovir is 5 mg/kg body weight (given as an intravenous infusion at a constant rate over 1 hr) administered once every two weeks. Cidofovir therapy should be discontinued and intravenous hydration is advised if serum creatinine increases by = 44 µmol/L (= 0.5 mg/dl), or if persistent proteinuria = 2+ develops. • Probenecid. -

HCV Eradication with Direct Acting Antivirals (Daas)?
HCV eradication with direct acting antivirals (DAAs)? Emilie Estrabaud Service d’Hépatologie et INSERM UMR1149, AP-HP Hôpital Beaujon, Paris, France. [email protected] HCV eradication with direct acting antivirals (DAAs)? HCV replication HCV genome and DAAs targets NS3 inhibitors NS5A inhibitors NS5B inhibitors Take home messages HCV viral cycle Asselah et al. Liver Int. 2015;35 S1:56-64. Direct acting antivirals 5’NTR Structural proteins Nonstructural proteins 3’NTR Metalloprotease Envelope Serine protease Glycoproteins RNA Capsid RNA helicase Cofactors Polymerase C E1 E2 NS1 NS2 NS3 NS4A NS4B NS5A NS5B Protease Inhibitors NS5A Inhibitors Polymerase Inhibitors Telaprevir Daclatasvir Nucs Non-Nucs Boceprevir Ledipasvir Simeprevir ABT-267 Sofosbuvir ABT-333 Faldaprevir GS-5816 VX-135 Deleobuvir Asunaprevir Direct Acting Antivirals: 2015 Asselah et al. Liver Int. 2015;35 S1:56-64. Genetic barrier for HCV direct acting antivirals High Nucleos(t)ide 1 mutation= high cost to Analog Inhibitors fitness, 2-3 additional mutations to increase fitness 2 st generation Protease Inhibitors n Non Nucleos(t)ide Analog Inhibitors : NS5 A Inhibitors 1 st generation Protease Inhibitors 1 mutation= low cost to fitness Low Halfon et al. J Hepatol 2011. Vol 55(1):192-206. HCV protease inhibitors (PI) Inhibit NS3/NS4A serine protease responsible for the processing of the polyprotein 1st generation 1st generation, 2nd wave 2nd generation Resistance low low high barrier Genotype activity 1: 1 a< 1b All except 3 all Drug drug Important Less Less interaction Drugs Boceprevir Simeprevir (Janssen) MK-5172 Telaprevir Faldaprevir (BI) ACH-2684 Paritaprevir (ABT-450)/r (AbbVie) Vedroprevir (Gilead) Vaniprevir (Merck) Sovaprevir (Achillion) Asunaprevir (BMS) NS3/NS4A structure Repositioning of helicase domain Self cleavage Lipid Bilayer Inactive Insertion of the Active carboxy-terminal tail Bartenschlager et al. -

Diapositiva 1
Resistencias & Epidemiología Eva Poveda Division of Clinical Virology INIBIC-Complexo Hospitalario Universitario de A Coruña Rapid Evolution of HCV Regimens: Easier to take/tolerate, Short Duration, Pangenotypic, Higher SVR, Eventually Oral for all patients SVR: 70-80% ≥ 90% ≥ 90% 2013 2014 2015 Genotype 2&3 Genotype 2 Genotypes 1-6 P/R SOF+RBV 12 weeks SOF+LPV ± RBV Genotypes 1 Genotype 3 ABT-450+ABT-267+ Telaprevir + P/R SOF+RBV 24 weeks ABT- 333 +RBV Boceprevir + P/R Genotypes 1-4 DCV+ASU SOF+ P/R SOF+DCV Genotypes 1&4 SMV+ P/R HCV Resistance to DAA During DAA-based treatment: ■ Rapid selection of resistance mutation may occur, eventually leading to viral break-through. Kieffer et al. Hepatology 2007; 46:631-9 Pilot-Matias et al. 46th EASL 2011, Abs1107 ■ Several changes at different positions at the NS3 protease, NS5B polymerase, and NS5A protein have been associated with loss of susceptibility to DAAs. Sarrazin et al. Gastroenterology 2010;138:447-62 MainTable 2. Main characteristics characteristics of the genotype of theactivity genotypeand resistance of DAA activity classes. and resistance of DAA classes. Genotype activity Resistance Key resistance mutations NS3 ■ First PI generation: genotypes 1 (1b >1a) Low genetic barrier First PI generation: protease (Telaprevir & Boceprevir) High cross-resistance G1a: R155K, V36M inhibitors G1b: V36M, T54A/S, A156T ■ Second wave and second PI generation: across all but genotype 3 (D168Q) Second wave and second PI generation: (Simeprevir, faldaprevir, vaniprevir, F43S, Q80K, R155K, D168A/E/H/T/V asunaprevir, sovaprevir, MK-5172, ACH-2684) NS5 Across all genotypes High genetic barrier Sofosbuvir*: nucleos(ti)de High cross-resistance G1a: S282T+(I434M) Sofosbuvir displays less antiviral activity G1b: S282T analogues againts genotypes 3 (treatment duration 24 G2a: S282T+(T179A, M289L, I293L, inhibitors weeks of sofosbuvir+RBV). -

Twelve-Week Ravidasvir Plus Ritonavir-Boosted Danoprevir And
bs_bs_banner doi:10.1111/jgh.14096 HEPATOLOGY Twelve-week ravidasvir plus ritonavir-boosted danoprevir and ribavirin for non-cirrhotic HCV genotype 1 patients: A phase 2 study Jia-Horng Kao,* Min-Lung Yu,† Chi-Yi Chen,‡ Cheng-Yuan Peng,§ Ming-Yao Chen,¶ Huoling Tang,** Qiaoqiao Chen** and Jinzi J Wu** *Graduate Institute of Clinical Medicine and Hepatitis Research Center, National Taiwan University College of Medicine and Hospital, ¶Division of Gastroenterology, Department of Internal Medicine, Taipei Medical University Shuang Ho Hospital, Taipei, †Division of Hepatobiliary, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung, ‡Division of Gastroenterology, Department of Internal Medicine, Chia-Yi Christian Hospital, Chiayi, and §Division of Hepatogastroenterology, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan; and **Ascletis BioScience Co., Ltd., Hangzhou, China Key words Abstract danoprevir, efficacy, hepatitis C, interferon free, ravidasvir. Background and Aim: The need for all-oral hepatitis C virus (HCV) treatments with higher response rates, improved tolerability, and lower pill burden compared with Accepted for publication 9 January 2018. interferon-inclusive regimen has led to the development of new direct-acting antiviral agents. Ravidasvir (RDV) is a second-generation, pan-genotypic NS5A inhibitor with high Correspondence barrier to resistance. The aim of this phase 2 study (EVEREST study) was to assess the ef- Jia-Horng Kao, Graduate Institute of Clinical ficacy and safety of interferon-free, 12-week RDV plus ritonavir-boosted danoprevir Medicine and Hepatitis Research Center, (DNVr) and ribavirin (RBV) regimen for treatment-naïve Asian HCV genotype 1 (GT1) National Taiwan University College of Medicine patients without cirrhosis. and Hospital, 7 Chung-Shan South Road, Taipei Methods: A total of 38 treatment-naïve, non-cirrhotic adult HCV GT1 patients were en- 10002, Taiwan. -

Egfr and the Risk of Community-Acquired Infections
CJASN ePress. Published on August 17, 2017 as doi: 10.2215/CJN.00250117 Article eGFR and the Risk of Community-Acquired Infections | | Hong Xu,*† Alessandro Gasparini,†‡ Junichi Ishigami,§ Khaled Mzayen, Guobin Su, ¶ Peter Barany,† Johan A¨rnlo¨v,**†† Bengt Lindholm,† Carl Gustaf Elinder,† Kunihiro Matsushita,§ and Juan Jesu´s Carrero*† Abstract Background and objectives Community-acquired infections are common, contributing to adverse outcomes and increased health care costs. We hypothesized that, with lower eGFR, the incidence of community-acquired infections increases, whereas the pattern of site-specific infections varies. Departments of 6 *Medical Epidemiology Design,setting, participants,&measurementsAmong 1,139,470health careusers(meanage =52 18 years old, 53% and Biostatistics and | women) from the Stockholm CREAtinine Measurements Project, we quantified the associations of eGFR with the Public Health † risk of infections, overall and major types, over 12 months. Sciences and Division of Renal Medicine and Baxter Novum, ResultsA total of 106,807 counts of infections were recorded throughout 1,128,313 person-years. The incidence rate Department of Clinical of all infections increased with lower eGFR from 74/1000 person-years for individuals with eGFR=90–104 ml/min Science, Intervention per 1.73 m2 to 419/1000 person-years for individuals with eGFR,30 ml/min per 1.73 m2.ComparedwitheGFRof and Technology, 90–104 ml/min per 1.73 m2, the adjusted incidence rate ratios of community-acquired infections were 1.08 (95% Karolinska Institutet, fi – 2 fi Stockholm, Sweden; con dence interval, 1.01 to 1.14) for eGFR of 30 59 ml/min per 1.73 m and 1.53 (95% con dence interval, 1.39 to ‡Department of Health , 2 1.69) for eGFR 30 ml/min per 1.73 m . -

Caracterización Molecular Del Perfil De Resistencias Del Virus De La
ADVERTIMENT. Lʼaccés als continguts dʼaquesta tesi queda condicionat a lʼacceptació de les condicions dʼús establertes per la següent llicència Creative Commons: http://cat.creativecommons.org/?page_id=184 ADVERTENCIA. El acceso a los contenidos de esta tesis queda condicionado a la aceptación de las condiciones de uso establecidas por la siguiente licencia Creative Commons: http://es.creativecommons.org/blog/licencias/ WARNING. The access to the contents of this doctoral thesis it is limited to the acceptance of the use conditions set by the following Creative Commons license: https://creativecommons.org/licenses/?lang=en Programa de doctorado en Medicina Departamento de Medicina Facultad de Medicina Universidad Autónoma de Barcelona TESIS DOCTORAL Caracterización molecular del perfil de resistencias del virus de la hepatitis C después del fallo terapéutico a antivirales de acción directa mediante secuenciación masiva Tesis para optar al grado de doctor de Qian Chen Directores de la Tesis Dr. Josep Quer Sivila Dra. Celia Perales Viejo Dr. Josep Gregori i Font Laboratorio de Enfermedades Hepáticas - Hepatitis Víricas Vall d’Hebron Institut de Recerca (VHIR) Barcelona, 2018 ABREVIACIONES Abreviaciones ADN: Ácido desoxirribonucleico AK: Adenosina quinasa ALT: Alanina aminotransferasa ARN: Ácido ribonucleico ASV: Asunaprevir BOC: Boceprevir CCD: Charge Coupled Device CLDN1: Claudina-1 CHC: Carcinoma hepatocelular DAA: Antiviral de acción directa DC-SIGN: Dendritic cell-specific ICAM-3 grabbing non-integrin DCV: Daclatasvir DSV: Dasabuvir -

Stamp-V3 1..249
23 March 2016 Volume 23 Supplement 1 S1 Volume 23 Volume Supplement 1 P ages A1–A262 ages EUROPEAN JOURNAL OF HOSPITAL PHARMACY OF HOSPITAL JOURNAL EUROPEAN ABSTRACT BOOK 21st Congress of the EAHP 16-18 March 2016 Vienna, Austria March 2016 March Contents Volume 23 Supplement 1 | EJHP March 2016 Abstracts from the EAHP 2016 Congress A1 Clinical pharmacy A172 Other hospital pharmacy topics A104 Drug distribution A178 Pharmacokinetics and pharmacodynamics A118 Drug information and pharmacotherapy A195 Production and preparation A158 General management A214 Patient safety and risk management A167 International posters A250 Author index POSTER AWARD NOMINEES Presentations on Wednesday, 16 March, 14:00–15:30, Room 93 Time Poster number Poster nominee oral presentations Author 14:00 DD-021 Medicine supply chain of a central pharmacy: risk mapping F Charra shortage 14:10 PP-001 Contamination with cytotoxic drugs in the workplace – E Korczowska ESOP pilot study 14:20 PP-039 Double checking manipulations for complex and/or high A Alcobia Martins risk preparations 14:30 CP-055 The clinical pharmacist resolves medication related E Tudela-Lopez problems in cranio, maxillofacial and oral surgery patients 14:40 CP-085 The impact of pharmacist interventions on safety M Tovar Pozo and cost savings 14:50 CP-219 Effectiveness and safety of switching to dual antiretroviral J Luis Revuelta therapy in a treatment experienced HIV cohort 15:00 DD-027 Implementation and evaluation of an appointment based F J Alvarez Manceñido model for outpatients attended in -

Synthesis and Evaluation of New HCV NS3/4A Protease Inhibitors
Synthesis and Evaluation of New HCV NS3/4A Protease Inhibitors A Major Qualifying Project Report: Submitted to the Faculty Of WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of the requirements for the Degree of Bachelor of Science By: ______________________ Evangelos Koumbaros Advisor Destin Heilman In Cooperation with Akbar Ali, Ph.D. UMass Medical School Table of Contents Acknowledgments ..................................................................................................................................... 4 Abstract ..................................................................................................................................................... 5 Background ............................................................................................................................................... 6 Protease Inhibitors ................................................................................................................................ 8 Telaprevir .............................................................................................................................................. 8 Boceprevir ............................................................................................................................................. 9 MK-5172 ............................................................................................................................................... 9 Methods ................................................................................................................................................. -

A Randomized, Double-Blind, Multiple-Dose Study of the Pan-Genotypic NS5A Inhibitor Samatasvir in Patients Infected with Hepatitis C Virus Genotype 1, 2, 3 Or 4
Accepted Manuscript A randomized, double-blind, multiple-dose study of the pan-genotypic NS5A inhibitor samatasvir in patients infected with hepatitis C virus genotype 1, 2, 3 or 4 Bradley Vince, John M. Hill, Eric J. Lawitz, William O’Riordan, Lynn R. Webster, Daniel M. Gruener, Ricky S. Mofsen, Abel Murillo, Eileen Donovan, Jie Chen, Joseph F. McCarville, John Z. Sullivan-Bólyai, Douglas Mayers, Xiao-Jian Zhou PII: S0168-8278(14)00014-2 DOI: http://dx.doi.org/10.1016/j.jhep.2014.01.003 Reference: JHEPAT 4997 To appear in: Journal of Hepatology Received Date: 8 October 2013 Revised Date: 29 December 2013 Accepted Date: 6 January 2014 Please cite this article as: Vince, B., Hill, J.M., Lawitz, E.J., O’Riordan, W., Webster, L.R., Gruener, D.M., Mofsen, R.S., Murillo, A., Donovan, E., Chen, J., McCarville, J.F., Sullivan-Bólyai, J.Z., Mayers, D., Zhou, X-J., A randomized, double-blind, multiple-dose study of the pan-genotypic NS5A inhibitor samatasvir in patients infected with hepatitis C virus genotype 1, 2, 3 or 4, Journal of Hepatology (2014), doi: http://dx.doi.org/10.1016/j.jhep. 2014.01.003 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. -

ABT-450/R (Abbott) – GS-9451 (Gilead) • Second Generation (Pan-Genotype, High Barrier to Resistance) – MK-5172 (Merck) – ACH-2684 (Achillion)
Paris Hepatitis Conference New Therapeutic Strategies Second Generation Protease inhibitors David R Nelson MD Professor and Associate Dean Director, Clinical and Translational Science Institute University of Florida Gainesville, USA Outline • HCV protease structure and drug targeting • First generation PIs – Major step forward – Major limitations • PIs in development – Second wave – Second generation • Clinical trial data – IFN-containing PI regimens – IFN-free PI containing regimens • Timelines and treatment paradigms NS3 protease targeting active site “catalytic triad” NS4A TARGETING . Substrate- and product analogs . Tri-peptides . Serine-trap inhibitors subdomain . Ketoamides (boceprevir, telaprevir) boundary . Macrocyclic inhibitors (e.g. Simeprevir, Danoprevir, Vaniprevir, etc.) zinc-finger . NS4A inhibitors Lorenz et al., Nature 2006 Kronenberger et al., Clin Liver Dis 2008 Welsch et al. Gut in press A Major Step Forward: First Generation PIs PegIFN/RBV BOC or TVR + pegIFN/RBV 100 69-83 80 63-75 40-59 60 38-44 29-40 SVR SVR (%) 40 24-29 20 7-15 5 0 Naive[1,2] Relapsers[3,4] Partial Null Responders[3,4] Responders[3,4] 1. Poordad F, et al. N Engl J Med. 2011;364:1195-1206. 2. Jacobson IM, et al. N Engl J Med. 2011;364:2405-2416. 3. Bacon BR, et al. N Engl J Med. 2011;364:1207-1217. 4. Zeuzem S, et al. N Engl J Med. 2011;364:2417-2428. 3. Bronowicki JP, et al. EASL 2012. Abstract 11. Limitations of First Generation PI-Based Therapy • Efficacy – Very dependent on the IFN response – Limited to gen 1 (1b>1a) • Low genetic barrier to