1 Human Genome-Edited Hematopoietic Stem Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Insights Towards FZ-CRD Folding and Therapeutic Landscape
Milhem and Ali Molecular Medicine (2020) 26:4 Molecular Medicine https://doi.org/10.1186/s10020-019-0129-7 REVIEW Open Access Disorders of FZ-CRD; insights towards FZ- CRD folding and therapeutic landscape Reham M. Milhem1* and Bassam R. Ali2,3 Abstract The ER is hub for protein folding. Proteins that harbor a Frizzled cysteine-rich domain (FZ-CRD) possess 10 conserved cysteine motifs held by a unique disulfide bridge pattern which attains a correct fold in the ER. Little is known about implications of disease-causing missense mutations within FZ-CRD families. Mutations in FZ-CRD of Frizzled class receptor 4 (FZD4) and Muscle, skeletal, receptor tyrosine kinase (MuSK) and Receptor tyrosine kinase- like orphan receptor 2 (ROR2) cause Familial Exudative Vitreoretinopathy (FEVR), Congenital Myasthenic Syndrome (CMS), and Robinow Syndrome (RS) respectively. We highlight reported pathogenic inherited missense mutations in FZ-CRD of FZD4, MuSK and ROR2 which misfold, and traffic abnormally in the ER, with ER-associated degradation (ERAD) as a common pathogenic mechanism for disease. Our review shows that all studied FZ-CRD mutants of RS, FEVR and CMS result in misfolded proteins and/or partially misfolded proteins with an ERAD fate, thus we coin them as “disorders of FZ-CRD”. Abnormal trafficking was demonstrated in 17 of 29 mutants studied; 16 mutants were within and/or surrounding the FZ-CRD with two mutants distant from FZ-CRD. These ER-retained mutants were improperly N-glycosylated confirming ER-localization. FZD4 and MuSK mutants were tagged with polyubiquitin chains confirming targeting for proteasomal degradation. Investigating the cellular and molecular mechanisms of these mutations is important since misfolded protein and ER-targeted therapies are in development. -

COA7 (C1orf163/RESA1) Mutations Associated With
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Apollo Mitochondrial genetics SHORT REPORT COA7 (C1orf163/RESA1) mutations associated with mitochondrial leukoencephalopathy and cytochrome c oxidase deficiency Anabel Martinez Lyons,1 Anna Ardissone,2 Aurelio Reyes,1 Alan J Robinson,1 Isabella Moroni,2 Daniele Ghezzi,3 Erika Fernandez-Vizarra,1 Massimo Zeviani1 1MRC-Mitochondrial Biology ABSTRACT mutations in mitochondrial DNA (mtDNA) or Unit, Cambridge, Background Assembly of cytochrome c oxidase (COX, nuclear DNA genes encoding structural COX subu- Cambridgeshire, UK 2Department of Child complex IV, cIV), the terminal component of the nits, but in most cases is due to recessive mutations Neurology, Milan, Italy mitochondrial respiratory chain, is assisted by several in nuclear genes encoding factors involved in COX 3Unit of Molecular factors, most of which are conserved from yeast to biogenesis.5 COA7 is a putative COX assembly Neurogenetics of the humans. However, some of them, including COA7, are factor containing five Sel1-like repeat domains Fondazione Istituto found in humans but not in yeast. COA7 is a 231aa- (Interpro IPR006597), is conserved in animals, but Neurologico “Carlo Besta”, Milan, Italy long mitochondrial protein present in animals, containing neither in plants nor in fungi, and has been five Sel1-like tetratricopeptide repeat sequences, which reported to localise in the mitochondrial IMS.6 Correspondence to are likely to interact with partner proteins. Here, we describe the first -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Blueprint Genetics Leukodystrophy and Leukoencephalopathy Panel
Leukodystrophy and Leukoencephalopathy Panel Test code: NE2001 Is a 118 gene panel that includes assessment of non-coding variants. In addition, it also includes the maternally inherited mitochondrial genome. Is ideal for patients with a clinical suspicion of leukodystrophy or leukoencephalopathy. The genes on this panel are included on the Comprehensive Epilepsy Panel. About Leukodystrophy and Leukoencephalopathy Leukodystrophies are heritable myelin disorders affecting the white matter of the central nervous system with or without peripheral nervous system myelin involvement. Leukodystrophies with an identified genetic cause may be inherited in an autosomal dominant, an autosomal recessive or an X-linked recessive manner. Genetic leukoencephalopathy is heritable and results in white matter abnormalities but does not necessarily meet the strict criteria of a leukodystrophy (PubMed: 25649058). The mainstay of diagnosis of leukodystrophy and leukoencephalopathy is neuroimaging. However, the exact diagnosis is difficult as phenotypes are variable and distinct clinical presentation can be present within the same family. Genetic testing is leading to an expansion of the phenotypic spectrum of the leukodystrophies/encephalopathies. These findings underscore the critical importance of genetic testing for establishing a clinical and pathological diagnosis. Availability 4 weeks Gene Set Description Genes in the Leukodystrophy and Leukoencephalopathy Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ABCD1* -

Identification of Genomic Targets of Krüppel-Like Factor 9 in Mouse Hippocampal
Identification of Genomic Targets of Krüppel-like Factor 9 in Mouse Hippocampal Neurons: Evidence for a role in modulating peripheral circadian clocks by Joseph R. Knoedler A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Neuroscience) in the University of Michigan 2016 Doctoral Committee: Professor Robert J. Denver, Chair Professor Daniel Goldman Professor Diane Robins Professor Audrey Seasholtz Associate Professor Bing Ye ©Joseph R. Knoedler All Rights Reserved 2016 To my parents, who never once questioned my decision to become the other kind of doctor, And to Lucy, who has pushed me to be a better person from day one. ii Acknowledgements I have a huge number of people to thank for having made it to this point, so in no particular order: -I would like to thank my adviser, Dr. Robert J. Denver, for his guidance, encouragement, and patience over the last seven years; his mentorship has been indispensable for my growth as a scientist -I would also like to thank my committee members, Drs. Audrey Seasholtz, Dan Goldman, Diane Robins and Bing Ye, for their constructive feedback and their willingness to meet in a frequently cold, windowless room across campus from where they work -I am hugely indebted to Pia Bagamasbad and Yasuhiro Kyono for teaching me almost everything I know about molecular biology and bioinformatics, and to Arasakumar Subramani for his tireless work during the home stretch to my dissertation -I am grateful for the Neuroscience Program leadership and staff, in particular -

Mitochondrial Structure and Bioenergetics in Normal and Disease Conditions
International Journal of Molecular Sciences Review Mitochondrial Structure and Bioenergetics in Normal and Disease Conditions Margherita Protasoni 1 and Massimo Zeviani 1,2,* 1 Mitochondrial Biology Unit, The MRC and University of Cambridge, Cambridge CB2 0XY, UK; [email protected] 2 Department of Neurosciences, University of Padova, 35128 Padova, Italy * Correspondence: [email protected] Abstract: Mitochondria are ubiquitous intracellular organelles found in almost all eukaryotes and involved in various aspects of cellular life, with a primary role in energy production. The interest in this organelle has grown stronger with the discovery of their link to various pathologies, including cancer, aging and neurodegenerative diseases. Indeed, dysfunctional mitochondria cannot provide the required energy to tissues with a high-energy demand, such as heart, brain and muscles, leading to a large spectrum of clinical phenotypes. Mitochondrial defects are at the origin of a group of clinically heterogeneous pathologies, called mitochondrial diseases, with an incidence of 1 in 5000 live births. Primary mitochondrial diseases are associated with genetic mutations both in nuclear and mitochondrial DNA (mtDNA), affecting genes involved in every aspect of the organelle function. As a consequence, it is difficult to find a common cause for mitochondrial diseases and, subsequently, to offer a precise clinical definition of the pathology. Moreover, the complexity of this condition makes it challenging to identify possible therapies or drug targets. Keywords: ATP production; biogenesis of the respiratory chain; mitochondrial disease; mi-tochondrial electrochemical gradient; mitochondrial potential; mitochondrial proton pumping; mitochondrial respiratory chain; oxidative phosphorylation; respiratory complex; respiratory supercomplex Citation: Protasoni, M.; Zeviani, M. -

Cytochrome C Oxidase Deficiency
Cytochrome c oxidase deficiency Description Cytochrome c oxidase deficiency is a genetic condition that can affect several parts of the body, including the muscles used for movement (skeletal muscles), the heart, the brain, or the liver. Signs and symptoms of cytochrome c oxidase deficiency usually begin before age 2 but can appear later in mildly affected individuals. The severity of cytochrome c oxidase deficiency varies widely among affected individuals, even among those in the same family. People who are mildly affected tend to have muscle weakness (myopathy) and poor muscle tone (hypotonia) with no other related health problems. More severely affected people have problems in multiple body systems, often including severe brain dysfunction (encephalomyopathy). Approximately one-quarter of individuals with cytochrome c oxidase deficiency have a type of heart disease that enlarges and weakens the heart muscle (hypertrophic cardiomyopathy). Another possible feature of this condition is an enlarged liver (hepatomegaly), which may lead to liver failure. Most individuals with cytochrome c oxidase deficiency have a buildup of a chemical called lactic acid in the body (lactic acidosis), which can cause nausea and an irregular heart rate, and can be life-threatening. Many people with cytochrome c oxidase deficiency have a specific group of features known as Leigh syndrome. The signs and symptoms of Leigh syndrome include loss of mental function, movement problems, hypertrophic cardiomyopathy, eating difficulties, and brain abnormalities. Cytochrome c oxidase deficiency is one of the many causes of Leigh syndrome. Many individuals with cytochrome c oxidase deficiency do not survive past childhood, although some individuals with mild signs and symptoms live into adolescence or adulthood. -

Skeletal Muscle Mitochondrial Oxidative
PhD Programme in Biomedical Sciences and Biotechnology XXXII Cycle PhD THESIS SKELETAL MUSCLE MITOCHONDRIAL OXIDATIVE PHOSPHORYLATION PLASTICITY IN TWO STUDIES ON HUMANS: EXERCISE TRAINING EFFECT IN OBESE SUBJECTS AND BED REST EFFECT IN HEALTHY SUBJECTS PhD Student: Supervisor: Benedetta Magnesa Prof. Bruno Grassi Co-supervisor: Dott.ssa Marina Comelli Year 2020 La misura dell’intelligenza è data dalla capacità di cambiare quando è necessario (Albert Einstein). ABSTRACT Mitochondrion is an important organelle for cells survival being involved in many cellular processes such as energy metabolism and homeostasis, cell division and differentiation, regulation of apoptosis and autophagy, etc. Mitochondrion, due to this role, is able to respond and adapt itself quickly to any perturbation and change of conditions in the different tissues of the human body including skeletal muscle. Thus, mitochondrial plasticity is one of the mechanisms that controls modification due to different physiological conditions such as weight loss or weight gain, exercise and physical inactivity/immobility in skeletal muscle; moreover it represents the capacity of a biologic system to respond to metabolic conditions in relation to the needs of the respective tissues. In this frame, this PhD Thesis investigated the role and adaptations of mitochondria in two different skeletal muscle pathophysiological models. Exercise is a fundamental tool known to trigger adaptations in mitochondria of skeletal muscle fibres in terms of both of exercise training and of reduced activity/immobility. The present PhD work evaluated the adaptations to exercise, or to the lack of exercise, at the level of mitochondrial oxidative phosphorylation in two conditions particularly relevant for the development of diseases. -

Functions of Cytochrome C Oxidase Assembly Factors
International Journal of Molecular Sciences Review Functions of Cytochrome c Oxidase Assembly Factors Shane A. Watson and Gavin P. McStay * Department of Biological Sciences, Faculty of School of Life Sciences and Education, Staffordshire University, Science Centre, Leek Road, Stoke-on-Trent ST4 2DF, UK; [email protected]ffs.ac.uk * Correspondence: gavin.mcstay@staffs.ac.uk; Tel.: +44-01782-295741 Received: 17 September 2020; Accepted: 23 September 2020; Published: 30 September 2020 Abstract: Cytochrome c oxidase is the terminal complex of eukaryotic oxidative phosphorylation in mitochondria. This process couples the reduction of electron carriers during metabolism to the reduction of molecular oxygen to water and translocation of protons from the internal mitochondrial matrix to the inter-membrane space. The electrochemical gradient formed is used to generate chemical energy in the form of adenosine triphosphate to power vital cellular processes. Cytochrome c oxidase and most oxidative phosphorylation complexes are the product of the nuclear and mitochondrial genomes. This poses a series of topological and temporal steps that must be completed to ensure efficient assembly of the functional enzyme. Many assembly factors have evolved to perform these steps for insertion of protein into the inner mitochondrial membrane, maturation of the polypeptide, incorporation of co-factors and prosthetic groups and to regulate this process. Much of the information about each of these assembly factors has been gleaned from use of the single cell eukaryote Saccharomyces cerevisiae and also mutations responsible for human disease. This review will focus on the assembly factors of cytochrome c oxidase to highlight some of the outstanding questions in the assembly of this vital enzyme complex. -
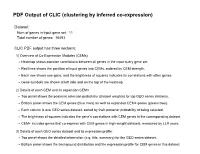
PDF Output of CLIC (Clustering by Inferred Co-Expression)
PDF Output of CLIC (clustering by inferred co-expression) Dataset: Num of genes in input gene set: 11 Total number of genes: 16493 CLIC PDF output has three sections: 1) Overview of Co-Expression Modules (CEMs) Heatmap shows pairwise correlations between all genes in the input query gene set. Red lines shows the partition of input genes into CEMs, ordered by CEM strength. Each row shows one gene, and the brightness of squares indicates its correlations with other genes. Gene symbols are shown at left side and on the top of the heatmap. 2) Details of each CEM and its expansion CEM+ Top panel shows the posterior selection probability (dataset weights) for top GEO series datasets. Bottom panel shows the CEM genes (blue rows) as well as expanded CEM+ genes (green rows). Each column is one GEO series dataset, sorted by their posterior probability of being selected. The brightness of squares indicates the gene's correlations with CEM genes in the corresponding dataset. CEM+ includes genes that co-express with CEM genes in high-weight datasets, measured by LLR score. 3) Details of each GEO series dataset and its expression profile: Top panel shows the detailed information (e.g. title, summary) for the GEO series dataset. Bottom panel shows the background distribution and the expression profile for CEM genes in this dataset. Overview of Co-Expression Modules (CEMs) with Dataset Weighting Scale of average Pearson correlations Num of Genes in Query Geneset: 11. Num of CEMs: 1. 0.0 0.2 0.4 0.6 0.8 1.0 Snrpf Snrpd3 Snrpb Snrnp25 Ybx1 Prkrip1 Toe1 -

Mitochondrial Dysfunction and Its Role in Tissue-Specific Cellular Stress
Review www.cell-stress.com Mitochondrial dysfunction and its role in tissue-specific cellular stress David Pacheu-Grau1,*, Robert Rucktäschel1 and Markus Deckers1,* 1 Department of Cellular Biochemistry, University Medical Center Göttingen, Germany. * Corresponding Authors: David Pacheu-Grau, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-394571; E-mail: [email protected]; Markus Deckers, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-395983; E-mail: [email protected] ABSTRACT Mitochondrial bioenergetics require the coordination of two dif- ferent and independent genomes. Mutations in either genome will affect mi- Received originally: 26.04.2018 tochondrial functionality and produce different sources of cellular stress. De- in revised form: 13.06.2018, Accepted 14.06.2018, pending on the kind of defect and stress, different tissues and organs will be Published 13.07.2018. affected, leading to diverse pathological conditions. There is no curative ther- apy for mitochondrial diseases, nevertheless, there are strategies described that fight the various stress forms caused by the malfunctioning organelles. Keywords: mitochondrial dysfunction, Here, we will revise the main kinds of stress generated by mutations in mito- cellular stress, mitochondrial chondrial genes and outline several ways of fighting this stress. pathology, therapy. Abbreviations: ADOA – autosomal dominant optic atrophy, AROA – autosomal recessive optic atrophy, ARS – aminoacyl-tRNA synthetase, CL – cardiolipin, CRISPR – clustered regularly interspaced short palindromic repeats, LHON – Leber’s hereditary optic neuropathy, mt - mitochondrial OXPHOS – oxidative phosphorylation, ROS – reactive oxygen species. MITOCHONDRIA AND CELL METABOLISM like superoxide and hydrogen peroxide.