Peripheral Nerve Entrapment and Their Surgical Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Median Nerve Compression at Pronator Teres
1 Median Nerve Compression at Pronator Teres Surgical Indications and Considerations Anatomical Considerations: The median nerve and brachial artery travel together down the arm. Therefore, one must be very careful not to interfere with either the median nerve or the brachial artery, especially when conducting surgical procedures. In the area of the pronator teres, there are many tendons as well. It is important to identify, as much as possible, the correct site of compression. Pathogenesis: The median nerve can get entrapped or compressed by several structures in the arm. The pronator teres muscle is the most common. Others entrapment sites include the flexor digitorum superficialis arch, the lacertus fibrosis (bicipital aponeurosis), and ligament of Struthers (frequency occurs in that order). For compression of the median nerve at the pronator teres and flexor digitorum superficialis, the cause is almost always due to hypertrophy of the respected muscle. This hypertrophy is from quick, forceful and repeated movements to the involved muscle. Examples include a carpenter or a baseball batter. As the muscle hypertrophies, the signal from the median nerve is diminished resulting in paresthesias in the median nerve distribution (lateral arm and hand) distal to the site of compression. Pain in the volar part of the forearm, often aggravated by repetitive supination and pronation, is a common symptom of pronator involvement. Another indicator is forearm pain with the compression of muscle such as pain in the volar part of the forearm implicating pronator teres. Onset is typically insidious and diagnosis is usually delayed 9 months to 2 years. Epidemiology: Pronator teres syndrome is the second most common cause of median nerve compression behind carpal tunnel syndrome. -

Piriformis Syndrome: the Literal “Pain in My Butt” Chelsea Smith, PTA
Piriformis Syndrome: the literal “pain in my butt” Chelsea Smith, PTA Aside from the monotony of day-to-day pains and annoyances, piriformis syndrome is the literal “pain in my butt” that may not go away with sending the kids to grandmas and often takes the form of sciatica. Many individuals with pain in the buttock that radiates down the leg are experiencing a form of sciatica caused by irritation of the spinal nerves in or near the lumbar spine (1). Other times though, the nerve irritation is not in the spine but further down the leg due to a pesky muscle called the piriformis, hence “piriformis syndrome”. The piriformis muscle is a flat, pyramidal-shaped muscle that originates from the front surface of the sacrum and the joint capsule of the sacroiliac joint (SI joint) and is located deep in the gluteal tissue (2). The piriformis travels through the greater sciatic foramen and attaches to the upper surface of the greater trochanter (or top of the hip bone) while the sciatic nerve runs under (and sometimes through) the piriformis muscle as it exits the pelvis. Due to this close proximity between the piriformis muscle and the sciatic nerve, if there is excessive tension (tightness), spasm, or inflammation of the piriformis muscle this can cause irritation to the sciatic nerve leading to symptoms of sciatica (pain down the leg) (1). Activities like sitting on hard surfaces, crouching down, walking or running for long distances, and climbing stairs can all increase symptoms (2) with the most common symptom being tenderness along the piriformis muscle (deep in the gluteal region) upon palpation. -

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -

Ulnar Claw-Hand Related Neglected Post-Traumatic Anterior Shoulder Joint Dislocation
Open Access Library Journal 2017, Volume 4, e3454 ISSN Online: 2333-9721 ISSN Print: 2333-9705 Ulnar Claw-Hand Related Neglected Post-Traumatic Anterior Shoulder Joint Dislocation Hermawan Nagar Rasyid Department of Orthopaedics and Traumatology, Faculty of Medicine, Universitas Padjadjaran, Dr. Hasan Sadikin Teaching Hospital, Bandung, Indonesia How to cite this paper: Rasyid, H.N. Abstract (2017) Ulnar Claw-Hand Related Neglected Post-Traumatic Anterior Shoulder Joint Shoulder joint is the most frequently dislocated joint. Humeral head disloca- Dislocation. Open Access Library Journal, tion pushed the nerve toward medial side. Neglected shoulder dislocation is 4: e3454. difficult to manage and requires extensive procedures to obtain good func- https://doi.org/10.4236/oalib.1103454 tional outcome. In the case of negligence, it is often found loss of the anterior Received: February 13, 2017 capsule due to absorption of the capsule. Nerve lesions, in particular the ulnar Accepted: March 17, 2017 nerve, often do not receive attention. Clinically, it often occurred from neura- Published: March 20, 2017 praxia to severe condition like claw-hand deformity. In my experience of a Copyright © 2017 by author and Open neglected case, there was a 53-year-old woman who presented to the ortho- Access Library Inc. paedic clinic with a left anterior shoulder fracture dislocation following a fall This work is licensed under the Creative onto the right shoulder and upper right arm. She had treated herself at home Commons Attribution International for around six months before visiting the clinic. She also complained of some License (CC BY 4.0). http://creativecommons.org/licenses/by/4.0/ deformities on her ring and little fingers, known as ulnar claw-hand. -

Neuropathy, Radiculopathy & Myelopathy
Neuropathy, Radiculopathy & Myelopathy Jean D. Francois, MD Neurology & Neurophysiology Purpose and Objectives PURPOSE Avoid Confusing Certain Key Neurologic Concepts OBJECTIVES • Objective 1: Define & Identify certain types of Neuropathies • Objective 2: Define & Identify Radiculopathy & its causes • Objective 3: Define & Identify Myelopathy FINANCIAL NONE DISCLOSURE Basics What is Neuropathy? • The term 'neuropathy' is used to describe a problem with the nerves, usually the 'peripheral nerves' as opposed to the 'central nervous system' (the brain and spinal cord). It refers to Peripheral neuropathy • It covers a wide area and many nerves, but the problem it causes depends on the type of nerves that are affected: • Sensory nerves (the nerves that control sensation>skin) causing cause tingling, pain, numbness, or weakness in the feet and hands • Motor nerves (the nerves that allow power and movement>muscles) causing weakness in the feet and hands • Autonomic nerves (the nerves that control the systems of the body eg gut, bladder>internal organs) causing changes in the heart rate and blood pressure or sweating • It May produce Numbness, tingling,(loss of sensation) along with weakness. It can also cause pain. • It can affect a single nerve (mononeuropathy) or multiple nerves (polyneuropathy) Neuropathy • Symptoms usually start in the longest nerves in the body: Feet & later on the hands (“Stocking-glove” pattern) • Symptoms usually spread slowly and evenly up the legs and arms. Other body parts may also be affected. • Peripheral Neuropathy can affect people of any age. But mostly people over age 55 • CAUSES: Neuropathy has a variety of forms and causes. (an injury systemic illness, an infection, an inherited disorder) some of the causes are still unknown. -

Hereditary Spastic Paraparesis: a Review of New Developments
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.69.2.150 on 1 August 2000. Downloaded from 150 J Neurol Neurosurg Psychiatry 2000;69:150–160 REVIEW Hereditary spastic paraparesis: a review of new developments CJ McDermott, K White, K Bushby, PJ Shaw Hereditary spastic paraparesis (HSP) or the reditary spastic paraparesis will no doubt Strümpell-Lorrain syndrome is the name given provide a more useful and relevant classifi- to a heterogeneous group of inherited disorders cation. in which the main clinical feature is progressive lower limb spasticity. Before the advent of Epidemiology molecular genetic studies into these disorders, The prevalence of HSP varies in diVerent several classifications had been proposed, studies. Such variation is probably due to a based on the mode of inheritance, the age of combination of diVering diagnostic criteria, onset of symptoms, and the presence or other- variable epidemiological methodology, and wise of additional clinical features. Families geographical factors. Some studies in which with autosomal dominant, autosomal recessive, similar criteria and methods were employed and X-linked inheritance have been described. found the prevalance of HSP/100 000 to be 2.7 in Molise Italy, 4.3 in Valle d’Aosta Italy, and 10–12 Historical aspects 2.0 in Portugal. These studies employed the In 1880 Strümpell published what is consid- diagnostic criteria suggested by Harding and ered to be the first clear description of HSP.He utilised all health institutions and various reported a family in which two brothers were health care professionals in ascertaining cases aVected by spastic paraplegia. The father was from the specific region. -
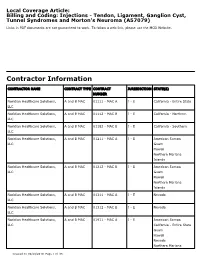
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Cubital Tunnel Syndrome)
DISEASES & CONDITIONS Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome) Ulnar nerve entrapment occurs when the ulnar nerve in the arm becomes compressed or irritated. The ulnar nerve is one of the three main nerves in your arm. It travels from your neck down into your hand, and can be constricted in several places along the way, such as beneath the collarbone or at the wrist. The most common place for compression of the nerve is behind the inside part of the elbow. Ulnar nerve compression at the elbow is called "cubital tunnel syndrome." Numbness and tingling in the hand and fingers are common symptoms of cubital tunnel syndrome. In most cases, symptoms can be managed with conservative treatments like changes in activities and bracing. If conservative methods do not improve your symptoms, or if the nerve compression is causing muscle weakness or damage in your hand, your doctor may recommend surgery. This illustration of the bones in the shoulder, arm, and hand shows the path of the ulnar nerve. Reproduced from Mundanthanam GJ, Anderson RB, Day C: Ulnar nerve palsy. Orthopaedic Knowledge Online 2009. Accessed August 2011. Anatomy At the elbow, the ulnar nerve travels through a tunnel of tissue (the cubital tunnel) that runs under a bump of bone at the inside of your elbow. This bony bump is called the medial epicondyle. The spot where the nerve runs under the medial epicondyle is commonly referred to as the "funny bone." At the funny bone the nerve is close to your skin, and bumping it causes a shock-like feeling. -

Focal Entrapment Neuropathies in Diabetes
Reviews/Commentaries/Position Statements REVIEW ARTICLE Focal Entrapment Neuropathies in Diabetes 1 1 AARON VINIK, MD, PHD LAWRENCE COLEN, MD millimeters]) is a risk factor (8,9). It used 1 2 ANAHIT MEHRABYAN, MD ANDREW BOULTON, MD to be associated with work-related injury, but now seems to be common in people in sedentary positions and is probably re- lated to the use of keyboards and type- MONONEURITIS AND because the treatment may be surgical (2) writers (dentists are particularly prone) ENTRAPMENT SYNDROMES — (Table 1). (10). As a corollary, recent data (3) in 514 Peripheral neuropathies in diabetes are a patients with CTS suggest that there is a diverse group of syndromes, not all of CARPAL TUNNEL threefold risk of having diabetes com- which are the common distal symmetric SYNDROME — Carpal tunnel syn- pared with a normal control group. If rec- polyneuropathy. The focal and multifocal drome (CTS) is the most common entrap- ognized, the diagnosis can be confirmed neuropathies are confined to the distribu- ment neuropathy encountered in diabetic by electrophysiological studies. Therapy tion of single or multiple peripheral patients and occurs as a result of median is simple, with diuretics, splints, local ste- nerves and their involvement is referred nerve compression under the transverse roids, and rest or ultimately surgical re- to as mononeuropathy or mononeuritis carpal ligament. It occurs thrice as fre- lease (11). The unaware physician seldom multiplex. quently in a diabetic population com- realizes that symptoms may spread to the Mononeuropathies are due to vasculitis pared with a normal healthy population whole hand or arm in CTS, and the signs and subsequent ischemia or infarction of (3,4). -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -

Physical Therapy Improved Hand Function in a Patient with Traumatic Peripheral Lesion: a Case Study
American Medical Journal 3 (2): 161-168, 2012 ISSN 1949-0070 © 2012 Science Publications Physical Therapy Improved Hand Function in a Patient with Traumatic Peripheral Lesion: A Case Study 1,2 Marco Orsini, 2,3 Julio Guilherme Silva, 3Clynton Lourenco Correa, 4Diego Rogrigues, 5Acary Bulle Oliveira, 4Valeria Marques Coelho, 4Debora Gollo, 1Antonio Marcos da Silva Catharino, 6Dionis Machado, 6Victor Hugo do Vale Bastos, 1Marco Antonio Araujo Leite, 7Gabriela Guerra Leal Souza, 1Carlos Henrique Melo Reis and 2Sara Lucia Silveira de Menezes 1Departament of Neurology, Nova Iguacu University, Hospital Geral de Nova Iguacu, Nova Iguacu, RJ, Brazil 2Master’s Program in Science of Rehabilitation, Augusto Motta University Centre (UNISUAM), Rio de Janeiro, RJ, Brazil 3Department of Medical Clinic, Faculty of Medicine, School of Physiotherapy, Federal University of Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil 4Fluminense Rehabilitation Association, Niteroi, RJ, Brazil 5Department of the, Neuromuscular Disease Federal University of Sao Paulo (UNIFESP), Vila Mariana, Sao Paulo, Brazil 6Department of the Physical Therapy Federal University of Piaui (UFPI), Parnaiba, Piaui, Brazil 7Department of Biological Sciences, Federal University of Ouro Preto (UFOP), Ouro Preto, MG, Brazil Abstract: Problem statement: Nerves are frequently injured by traumatic lesions, such as crushing, compression (entrapment), stretching, partial and total extraction, resulting in damages to the transmission of nerve impulses and to the reduction or loss of sensitivity, to the motility and to the reflexes of the innervated area. The objective of this study was to evaluate the results of a rehabilitation program that lasted three months in the process of traumatic injury recovery of the median and ulnar nerves in a 52 year-old patient. -

An Unusual Cause of Pseudomedian Nerve Palsy
Hindawi Publishing Corporation Case Reports in Neurological Medicine Volume 2011, Article ID 474271, 3 pages doi:10.1155/2011/474271 Case Report An Unusual Cause of Pseudomedian Nerve Palsy Zina-Mary Manjaly, Andreas R. Luft, and Hakan Sarikaya Department of Neurology, University Hospital Zurich, Frauenklinikstraße 26, 8091 Zurich,¨ Switzerland Correspondence should be addressed to Zina-Mary Manjaly, [email protected] Received 20 July 2011; Accepted 9 August 2011 Academic Editors: J. L. Gonzalez-Guti´ errez,´ V. Rajajee, and Y. Wakabayashi Copyright © 2011 Zina-Mary Manjaly et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We describe a patient who presented with an acute paresis of her distal right hand suggesting a peripheral median nerve lesion. However, on clinical examination a peripheral origin could not be verified, prompting further investigation. Diffusion-weighted magnetic resonance imaging revealed an acute ischaemic lesion in the hand knob area of the motor cortex. Isolated hand palsy in association with cerebral infarction has been reported occasionally. However, previously reported cases presented predominantly as ulnar or radial palsy. In this case report, we present a rather rare finding of an acute cerebral infarction mimicking median never palsy. 1. Case median nerve, which was normal (Figure 1(c)). Magnetic resonance imaging (MRI) on the same day revealed a small A 60-year-old woman presented to the emergency depart- diffusion restriction in a part of the left precentral gyrus that ffi ment with di culty in moving the thumb, index, and middle is known as “the hand knob” area (Figure 1(d))[2].