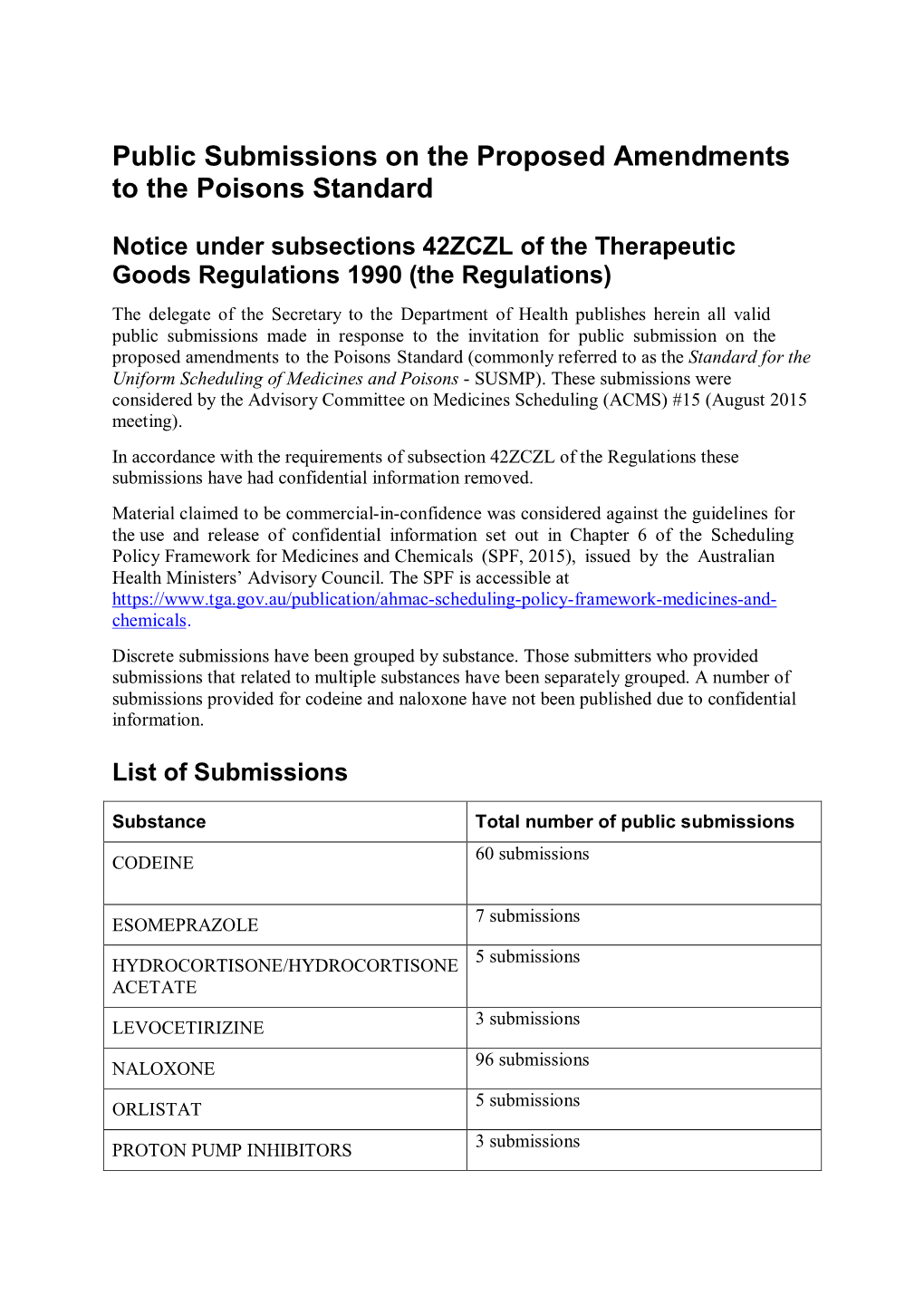
Public Submissions on Scheduling Matters Referred to the ACMS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CHRONIC NON PALLIATIVE PAIN (> 6 Months)
CHRONIC NON PALLIATIVE PAIN (> 6 months) IN ADULTS – Primary Care Treatment Pathway Please note that this pathway is currently under review following publication of NICE guideline [NG193] - Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain (April 2021): https://www.nice.org.uk/guidance/ng193. Initial Assessment • Exclude serious pathology / red flags (investigate / refer as necessary). • Investigate and manage any underlying condition. • Determine pain type - nociceptive, mixed, neuropathic. Typical features of neuropathic pain: burning, shooting, allodynia, hyperalgesia, unpredictable, abnormal sensations. • Determine baseline severity of pain & functional impact. Use visual analogue or numerical rating scales (pain scales available from the British Pain Society). • If musculoskeletal pain offer manual therapy in addition to or instead of analgesics if appropriate. • Explore use of non-drug options e.g. psychological therapy and physical intervention therapies. Consider early specialis t referral • Where pain is severe or not responding to management. • Patients considered at increased risk of poor outcomes. For back pain consider use of Keele STarT Back Tool. Before prescribing • Determine use of over-the-counter (OTC) treatments / complemen tary therapies. • Offer British Pain Society leaflet https://www.britishpainsociety.org/static/upload s/resources/files/patient_pub_otc.pdf • Agree and document achievable pain goal e.g. 50% reduction in pain, improved function. • Advise on risks/benefits of medication, regime and target dose . • Avoid effervescent preparations, particularly with hypertension (due to salt content). • Prescribe single-constituent analgesics where appropriate, to allow independent titration of each drug. • Avoid low dose compound analgesics (e.g. co-codamol 8/500 mg and co-dydramol 10/500 mg). -

Analgesic Policy
AMG 4pp cvr print 09 8/4/10 12:21 AM Page 1 Mid-Western Regional Hospitals Complex St. Camillus and St. Ita’s Hospitals ANALGESIC POLICY First Edition Issued 2009 AMG 4pp cvr print 09 8/4/10 12:21 AM Page 2 Pain is what the patient says it is AMG-Ch1 P3005 3/11/09 3:55 PM Page 1 CONTENTS page INTRODUCTION 3 1. ANALGESIA AND ADULT ACUTE AND CHRONIC PAIN 4 2. ANALGESIA AND PAEDIATRIC PAIN 31 3. ANALGESIA AND CANCER PAIN 57 4. ANALGESIA IN THE ELDERLY 67 5. ANALGESIA AND RENAL FAILURE 69 6. ANALGESIA AND LIVER FAILURE 76 1 AMG-Ch1 P3005 3/11/09 3:55 PM Page 2 CONTACTS Professor Dominic Harmon (Pain Medicine Consultant), bleep 236, ext 2774. Pain Medicine Registrar contact ext 2591 for bleep number. CNS in Pain bleep 330 or 428. Palliative Care Medical Team *7569 (Milford Hospice). CNS in Palliative Care bleeps 168, 167, 254. Pharmacy ext 2337. 2 AMG-Ch1 P3005 3/11/09 3:55 PM Page 3 INTRODUCTION ANALGESIC POLICY ‘Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ [IASP Definition]. Tolerance to pain varies between individuals and can be affected by a number of factors. Factors that lower pain tolerance include insomnia, anxiety, fear, isolation, depression and boredom. Treatment of pain is dependent on its cause, type (musculoskeletal, visceral or neuropathic), duration (acute or chronic) and severity. Acute pain which is poorly managed initially can degenerate into chronic pain which is often more difficult to manage. -

Compound Analgesic)
Bex (compound analgesic) Bex was a strong compound analgesic which was popular in Australia for much of the twentieth century. It came in the form of APC (aspirinâ“phenacetinâ“caffeine) tablets or powder, containing 42% aspirin, 42% phenacetin, plus caffeine. Bex was a product of Beckers Pty Ltd., originally based at Pym Street, Dudley Park, South Australia, but which relocated to Sydney in the 1960s. It was advertised with the phrase, "Stressful Day? What you need is a cup of tea, a Bex and a good lie down". Bex was a strong compound analgesic which was popular in Australia for much of the twentieth century. It came in the form of APC tablets or powder, containing 42% aspirin, 42% phenacetin, plus caffeine.[1]. For faster navigation, this Iframe is preloading the Wikiwand page for Bex (compound analgesic). Home. News. Bex (compound analgesic) Bex was a strong compound analgesic which was popular in Australia for much of the twentieth century. It came in the form of APC (aspirinâ“phenacetinâ“caffeine) tablets or powder, containing 42% aspirin, 42% phenacetin, plus caffeine.[1] Bex was a product of Beckers Pty Ltd., originally based at Pym Street, Dudley Park, South Australia,[2] but which relocated to Sydney in the 1960s.[3] It was advertised with the phrase, "Stressful Day? What you need is a cup of tea, a Bex and a good lie. Compound analgesics are those with multiple active ingredients; they include many of the stronger prescription analgesics. Active ingredients that have been commonly used in compound analgesics include: aspirin or ibuprofen. -

Central Nervous System 4.1 Hypnotics and Anxiolytics
BNF CHAPTER 4: CENTRAL NERVOUS SYSTEM Link to: CWP Mental Health Formulary 4.1 HYPNOTICS AND ANXIOLYTICS Benzodiazepine prescribing guidelines Benzodiazepines must not be prescribed routinely. Benzodiazepines must not be prescribed for more than 10 nights as a hypnotic or as an anxiolytic for more than 4 weeks. Apart from chronic users, patients should generally not be discharged from hospital taking a benzodiazepine. An example of where it may be appropriate includes patients receiving palliative care. Can be difficult to withdraw benzodiazepines if they have been taken regularly for more than a few weeks. 4.1.1 HYPNOTICS Temazepam 10mg tablets 10mg/5mL elixir Temazepam for ward stock must be ordered using the Controlled Drug order book. Zopiclone 3.75mg, 7.5mg tablets Hypnotics should only be prescribed for short term use. Patients requiring hypnotics in hospital should have them prescribed on the PRN side of the prescription chart. Such patients will not have hypnotics prescribed to them on discharge. It is recommended that, because of the lack of compelling evidence to distinguish between zopiclone or the shorter acting benzodiazepine hypnotics, the drug with the lowest purchase cost (taking into account daily required dose and product price per dose) should be prescribed. (NICE Technology Appraisal No 77). Temazepam is therefore the preferred option for all patients on the basis of cost. However, in the Trust, zopiclone may be considered for first line use as it is not subject to internal controlled drug restrictions. Joint -

Cobrotoxin-Containing Analgesic Compound to Treat Chronic
1077-1084 6/10/06 16:33 Page 1077 ONCOLOGY REPORTS 16: 1077-1084, 2006 Cobrotoxin-containing analgesic compound to treat chronic moderate to severe cancer pain: Results from a randomized, double-blind, cross-over study and from an open-label study J.M. XU1, S.T. SONG1, F.Y. FENG2, F.L. HUANG3, Y. YANG4, G.R. XIE5, L.G. XU6, C.Z. ZHANG7, M. BRUNO8 and A. PARADISO8 1Beijing 307 Hospital Cancer Center; 2Cancer Hospital, Chinese Academy of Medical Sciences, Beijing; 3Jiangsu Province Cancer Hospital, Nanjing; 4Kunming the PLA General Hospital, Kunming; 5Tianjin Cancer Hospital, Tianjin; 6Cancer Hospital, Fudan University, Shanghai; 7The Third Teaching Hospital, Kunming Medical University, Kunming, P.R. China; 8National Cancer Institute, Bari, Italy Received June 5, 2006; Accepted July 19, 2006 Abstract. Cobrotoxin produces intense analgesia but it has satisfactory pain relief. Pain response was classified as CR, an onset of response of 1-3 h which hampers its clinical use PR and NC. CR was defined as 100% pain relief, with a pain in cancer pain. Recently, a compound analgesic formulation score of 0 on a 0-10 VAS. PR was defined as decreased to combining cobrotoxin, tramadol hydrochloride and ibuprofen mild pain, with a pain score of no more than 4 on a 0-10 VAS. (Compound Keluoqu, CKLQ) has become available in China. NC was defined as pain that either remained unchanged or The aim of this study was to evaluate the clinical efficacy of that was reduced from severe to moderate at baseline, with a CKLQ for moderate to severe cancer pain. -

Wemerec Stopping Codeine
Online content Stopping compound medications containing codeine __________________________________________________________________________________________________ Numerous compound analgesic preparations combine a ‘weak’ opioid (codeine or dihydrocodeine) with a non- opioid (paracetamol or a nonsteroidal anti-inflammatory drug [NSAID]). As with other compound products, these can be convenient but “reduce the scope for effective titration of individual components.”1 Using compound analgesics reduces flexibility when managing pain of varying intensity and can complicate the management of adverse effects and overdose. Prescription products that deliver a ‘full dose’ of both non-opioid and opioid (e.g. 60 mg of codeine) are effective analgesics for mild to moderate pain, but are associated with the full range of opioid-related adverse effects.1 Codeine is a prodrug, whose principal metabolite is morphine. There is some concern that variations in genetic factors can influence the metabolism of codeine and, therefore, the predictability of its effects.2 Furthermore, the dose of opioid that causes toxicity varies between individuals and may be dependent on other factors, including medical co-morbidity (particularly hepatic and renal impairment) and concomitant medication (including over-the-counter [OTC] medications and illicit drugs).1,3 Many patients who become dependent§ on prescription codeine medicines supplement their use with OTC codeine-containing products. This puts them at even greater risk of adverse effects and overdose from both the opioid and non-opioid components.4 Combination products that utilise a low dose of opioid (e.g. 8 mg codeine) have not been shown to be more effective than non-opioids alone5 and may still cause adverse opioid effects. These products are available both with and without a prescription. -

The Pharmacological Management of Adults with Chronic Non-Cancer Pain
The Pharmacological Management of Adults with Chronic Non-Cancer Pain Please also refer to: ELHE Managed Opioid Reduction Pathway Faculty of Pain Medicine - Dose equivalents and changing opioids Original author: Susan McKernan Midlands and Lancashire CSU May 2018 (Review date Autumn 2019) VERSION CONTROL. Please access via the LMMG website to ensure that the correct version is in use. Version Date Amendments made Number 1.0 14/5/15 First version approved 1.1 14/7/15 Updated to include information about renal safety of fentanyl and Fentanyl: oral morphine equivalence changed to 60-90mg 2.0 17/01/17 Appendix 5 added. AG. 3.0 25/04/18 Appendix 3 updated including use of buprenorphine 15mcg/hr patches and information added about source of dose conversion ratios. 3.1 16/07/19 Reference to prescribing >120mg morphine removed pending update to new guidance Autumn 2019. 3.2 4/12/20 Appendix 5 removed – opioid tapering and withdrawal guidance Contents 1. INTRODUCTION ......................................................................................................................3 2. PURPOSE AND SUMMARY....................................................................................................3 3. SCOPE ................................................................................................................................ 3 4. GUIDANCE ...............................................................................................................................3 4.1 Summary of Chronic Non- Cancer Pain Management. 1,4,5,8,18 -

Tissue Hypoxia, Oxidative Stress and Topical Analgesics in the Treatment of Complex Regional Pain Syndrome and Peripheral Neuropathic Pain
Tissue hypoxia, oxidative stress and topical analgesics in the treatment of complex regional pain syndrome and peripheral neuropathic pain Oli Abate Fulas Integrated Program in Neuroscience Faculty of Medicine McGill University August 2020 A thesis submitted to McGill University in partial fulfillment of the requirements of the degree of Doctor of Philosophy © Oli Abate Fulas, 2020 ABSTRACT Peripheral neuropathic pain (PNP) and complex regional pain syndrome (CRPS) are chronic pain conditions whose pharmacological treatments are partial in efficacy and cause adverse systemic effects. This work is aimed at developing more effective and better-tolerated analgesics for PNP and CRPS through the targeting of peripheral tissue hypoxia and oxidative stress using topical agents. Both are processes that are prominent inducers of peripheral sensitization and can be directly impacted by topically administered treatments whose systemic effects are minimal. Initial studies assessed the analgesic effect of a new topical formulation made by combining the vasoactive agent meldonium and the antioxidant N-acetyl cysteine. The treatment alleviated mechanical hypersensitivity in rat models of PNP and CRPS by enhancing nitric oxide- mediated tissue oxygenation. Thus, topical treatment reversed the reduction in tissue oxygenation observed by percutaneous oxygen saturation measurements on the hind paws of chronic post- ischemic pain (CPIP) rat models of CRPS. The anti-allodynic dose of topical meldonium-NAC also produced a significant increase in the nitric oxide levels of plantar muscle of rats with CPIP. In line with this, pre-treatment with a nitric oxide synthase inhibitor attenuated the topical anti- allodynic effects of meldonium-NAC. In subsequent studies, the repertoire of similarly acting topical combinations was expanded and the method of formulating the combinations refined with the goal of simplifying the drugs’ development and hastening clinical translation. -

Chronic Pain: Supporting Safer Prescribing of Analgesics
Chronic pain: supporting safer prescribing of analgesics March 2017 British Medical Association bma.org.uk British Medical Association Chronic pain: supporting safer prescribing of analgesics 1 Contents 1 Background ............................................................................................................................................................2 2 Introduction ...........................................................................................................................................................3 2.1 Defining chronic pain ................................................................................................................................3 2.2 Prevalence of chronic pain .....................................................................................................................3 2.3 Analgesic drugs ...........................................................................................................................................4 3 Analgesic use for chronic pain .......................................................................................................................5 3.1 Analgesic prescribing for chronic pain: UK trends...................................................................... 5 3.2 Analgesic use in chronic pain – exploring the evidence ...........................................................7 3.3 Potential harms associated with long-term analgesic use in chronic pain ...................11 4 Supporting the management of patients with chronic -

Phytochemistry and Natural Products Cpph403
PHYTOCHEMISTRY AND NATURAL PRODUCTS CPPH403 Dr. Dima MUHAMMAD 2018-2019 1 -Trease and Evans Pharmacognosy, William C. Evans, Saunders Elsevier, 2009, sixteenth edition., ISBN 978-0 -7020 -2934 9 2- Textbook of pharmacognosy & phytochemistry, Biren Shah & A.K. Seth, Elsevier, 2010, 1st edition, ISBN: 978-81- 312-2298-0 3-Medicinal Natural Products: A Biosynthetic Approach. Paul M Dewick, John Wiley & Sons, 2009,3rd edition, ISBN 978-0-470-74168-9. 4- Pharmacognosy. Phytochemistry, medicinal plants. Bruneton Jean, Lavoisier; 2009 4th edition; ISBN 978- 2743011888. 1 Dr. Dima MUHAMMAD PHYTOCHEMISTRY & NATURAL PRODUCTS PRIMARY AND SECONDARY METABOLISM All organisms need to transform and interconvert a vast number of organic compounds to enable them to live, grow, and reproduce. They need to provide themselves with energy in the form of ATP, and a supply of building blocks to construct their own tissues. An integrated network of enzyme-mediated and carefully regulated chemical reactions is used for this purpose, collectively referred to as intermediary metabolism, and the pathways involved are termed metabolic pathways. Despite the extremely varied characteristics of living organisms, the pathways for generally modifying and synthesizing carbohydrates, proteins, fats, and nucleic acids are found to be essentially the same in all organisms, apart from minor variations. These processes demonstrate the fundamental unity of all living matter, and are collectively described as primary metabolism. In contrast to these primary metabolic pathways, which synthesize, degrade, and generally interconvert compounds commonly encountered in all organisms, there also exists an area of metabolism concerned with compounds which have a much more limited distribution in nature. -
149I. Non-Neuropathic Pain
149 | January 2017 | 2.3 Community Interest Company Management of non-neuropathic pain Current spend on analgesia across England and Wales is over £136.5 million (ePACT April to June 2016). This breaks down to over £18.7 million on simple analgesics, £32.9 million on weak opioids, £86.8 million on strong opioids and £15.9 million on NSAIDs. Medicines optimisation projects in this area are aimed at reviewing pain pathways and facilitating the appropriate primary care management of pain, in all patients aged 18 years and over suffering from chronic pain. This document does not cover the specific management of pain associated with cancer. This project should be used in conjunction with other PrescQIPP projects: Oxycodone MR https://www.prescqipp.info/oxycodone-mr/category/61-oxycodone-mr NSAIDs https://www.prescqipp.info/nsaids/category/175-nsaids Opioid patches https://www.prescqipp.info/opioid-patches/category/120-opioid-patches Oxycodone/Naloxone prolonged release tablets https://www.prescqipp.info/-oxycodone/naloxone- prolonged-release-tablets/category/105-oxycodone-naloxone-prolonged-release-targinact-tablets Tramacet® https://www.prescqipp.info/-tramacet/category/59-tramacet Further resources available with this bulletin: Briefing, pain pathway, patient agreement, patient information of adverse effects with inappropriate use, community pharmacist support letter, audit, slide set. Recommendations • Use medication for pain only as part of a wider management plan aimed at reducing disability and improving quality of life. Patients should be informed that analgesia will only offer a 30-50% reduction in pain relief.1,2 • Consider non opioid interventions (paracetamol +/-NSAIDs and non-pharmacological interventions) before opioid therapy.1-3 See attachment 1: Treatment pathway for non cancer pain in adults. -

NDPSC Record of Reasons February 2007
National Drugs and Poisons Schedule Committee Record of Reasons 49th Meeting 20-22 February 2007 National Drugs and Poisons Schedule Committee Record of Reasons of Meeting 49 – 20-22 February 2007 i TABLE OF CONTENTS GLOSSARY................................................................................................................................................ IV 1. PRELIMINARY MATTERS..............................................................................................................8 1.7 PROCEDURAL MATTERS........................................................................................................8 1.7.1 Operations/Policies of the Committee .....................................................................................8 1.7.1.1 [Item Deleted] .............................................................................................................................. 8 1.7.1.2 Guidelines for confidential information - Medicines ................................................................... 8 1.7.1.3 Derivative Usage in the SUSDP................................................................................................. 13 1.8 NDPSC WORKING PARTIES ..................................................................................................17 1.8.1 Trans-Tasman Harmonisation Working Party ......................................................................17 1.8.1.1 Foreshadowed harmonisation proposals – hyaluronidase and methyl salicylate........................ 17 1.8.1.2 Deferred harmonisation