SJH Procedures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

The Differences Between ICD-9 and ICD-10
Preparing for the ICD-10 Code Set: Fact Sheet 2 October 1, 2015 Compliance Date Get the Facts to be Compliant Alert: The new ICD-10 compliance date is October 1, 2015. The Differences Between ICD-9 and ICD-10 This is the second fact sheet in a series and is focused on the differences between the ICD-9 and ICD-10 code sets. Collectively, the fact sheets will provide information, guidance, and checklists to assist you with understanding what you need to do to implement the ICD-10 code set. The ICD-10 code sets are not a simple update of the ICD-9 code set. The ICD-10 code sets have fundamental changes in structure and concepts that make them very different from ICD-9. Because of these differences, it is important to develop a preliminary understanding of the changes from ICD-9 to ICD-10. This basic understanding of the differences will then identify more detailed training that will be needed to appropriately use the ICD-10 code sets. In addition, seeing the differences between the code sets will raise awareness of the complexities of converting to the ICD-10 codes. Overall Comparisons of ICD-9 to ICD-10 Issues today with the ICD-9 diagnosis and procedure code sets are addressed in ICD-10. One concern today with ICD-9 is the lack of specificity of the information conveyed in the codes. For example, if a patient is seen for treatment of a burn on the right arm, the ICD-9 diagnosis code does not distinguish that the burn is on the right arm. -

Burns, Surgical Treatment
Philippine College of Surgeons Dear PCS Fellows, We at the PCS Committee on HMO, RVS, & PHIC & The PCS Board of Regents are pleased to announce the Adoption of PAHMOC of our new & revised RVS. We are currently under negotiations with them with regard to the multiplier to be used to arrive at our final professional Fees. Rest assured that we will have a graduated & staggered increase of PF thru the years from what we are currently receiving due to the proposed yearly increments in the multiplier. To those Fellows who haven’t signed the USA (Universal Service Agreement found here in our PCS website) please be reminded to sign and submit to the PCS Secretariat, as only those who did and are in good standing (updated annual dues) will be eligible to avail of the benefits of the new RVS scale. Indeed, we are hoping & looking forward to a merrier 2020 Christmas for our Fellows. Yours truly, FERNANDO L. LOPEZ, MD, FPCS Chairman Noted by: JOSELITO M. MENDOZA, MD, FPCS Regent-in-Charge JOSE ANTONIO M. SALUD, MD, FPCS President For many years now the PCS Committee on HMO & RUV has been compiling, with the assistance of the different surgical subspecialties, a new updated list of RUV for each procedure to replace the existing manual of 2009. This new version not only has a more complete listing of cases but also includes the newly developed procedures particularly for all types of minimally invasive operations. Sometime last year, the Department of Health released Circular 2019-0558 on the Public Access to the Price Information by all Health Providers as required by Section 28.16 of the IRR of the Universal Health Care Act. -
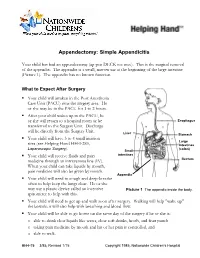
Appendectomy: Simple Appendicitis
Appendectomy: Simple Appendicitis Your child has had an appendectomy (ap pen DECK toe mee). This is the surgical removal of the appendix. The appendix is a small, narrow sac at the beginning of the large intestine (Picture 1). The appendix has no known function. What to Expect After Surgery . Your child will awaken in the Post Anesthesia Care Unit (PACU) near the surgery area. He or she may be in the PACU for 1 to 2 hours. After your child wakes up in the PACU, he or she will return to a hospital room or be Esophagus transferred to the Surgery Unit. Discharge will be directly from the Surgery Unit. Liver Stomach . Your child will have 3 to 4 small incision Large sites (see Helping Hand HH-I-283, Intestines Laparoscopic Surgery (colon) ). Small . Your child will receive fluids and pain intestines medicine through an intravenous line (IV). Rectum When your child can take liquids by mouth, pain medicine will also be given by mouth. Appendix . Your child will need to cough and deep-breathe often to help keep the lungs clear. He or she may use a plastic device called an incentive Picture 1 The appendix inside the body. spirometer to help with this. Your child will need to get up and walk soon after surgery. Walking will help "wake up" the bowels; it will also help with breathing and blood flow. Your child will be able to go home on the same day of the surgery if he or she is: o able to drink clear liquids like water, clear soft drinks, broth, and fruit punch o taking pain medicine by mouth and his or her pain is controlled, and o able to walk. -

About Liver Resection
ABOUT LIVER RESECTION Surgical removal of part of the liver A guide for patients and relatives This booklet has been written to provide information about the operation called a liver resection. This is a major operation and involves removal of a part of the liver. Information about the benefits and risks will help you make an informed decision about the operation. It is important to remember that each person is different. This booklet cannot replace the professional advice and expertise of a doctor who is familiar with your condition. If you have questions that this booklet does not cover, please discuss them with your surgeon or cancer nurse specialist. page 2 What is the liver? The liver is a large organ which lies on the right side of the upper abdomen, under the rib cage. It has many functions related to body metabolism (chemical processes within the body) and is very important to health. One of its functions is to produce yellow-green fluid called bile. Bile flows down a tube called the bile duct to the intestine, where it mixes with food and helps digestion. The gall bladder is a small sac attached to the side of the bile duct. The gall bladder stores excess bile and pushes it down the bile duct in to the intestine, ready for when it is needed for digestion. The liver has right and left lobes (sections). An artery (hepatic artery) and a vein (portal vein) carry blood to the liver. Blood from the liver flows through the hepatic veins back to the heart. -
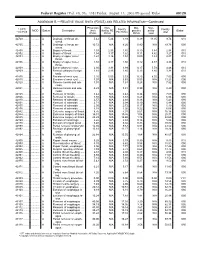
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

Incidental Drainage of a Periappendicular Abscess During Colonoscopy
UCTN – Unusual cases and technical notes E175 Incidental drainage of a periappendicular abscess during colonoscopy A 50-year-old man was referred to the of oral metronidazole and ciprofloxacin. A P. Figueiredo, V. Fernandes, J. Freitas outpatient colonoscopy clinic after a posi- computed tomography (CT) scan 1 week Department of Gastroenterology, tive fecal occult blood test during screen- after the procedure revealed no abnormal Hospital Garcia de Orta, Almada, Portugal ing for colorectal cancer. Colonoscopy, findings and the patient remained asymp- which was performed with the patient tomatic. sedated, revealed a 12-mm tumor covered Acute appendicitis is the most frequent References by normal, smooth mucosa at the site of acute abdominal emergency seen in de- 1 Oliak D, Yamini D, Udani VM et al. Can per- forated appendicitis be diagnosed preopera- the appendicular orifice. A biopsy was veloped countries. Its most common com- tively based on admission factors? J Gastro- taken, but this led to an immediate puru- plication is perforation and this may be intest Surg 2000; 4: 470–474 lent discharge occurring from the lesion followed by abscess formation [1]. Colo- 2 Ohtaka M, Asakawa A, Kashiwagi A et al. (●" Video 1). Therefore, a diagnosis of a noscopic diagnosis and treatment of a Pericecal appendiceal abscess with drainage periappendicular abscess was incidentally periappendicular abscess is rare [2]. In during colonoscopy. Gastrointest Endosc 1999; 49: 107–109 established. this case a periappendicular abscess was 3 Antevil J, Brown C. Percutaneous drainage After the patient had recovered from the incidentally discovered and drained dur- and interval appendectomy. In: Scott-Turner sedation, he was specifically questioned ing a colonoscopy. -

IPEG's 25Th Annual Congress Forendosurgery in Children
IPEG’s 25th Annual Congress for Endosurgery in Children Held in conjunction with JSPS, AAPS, and WOFAPS May 24-28, 2016 Fukuoka, Japan HELD AT THE HILTON FUKUOKA SEA HAWK FINAL PROGRAM 2016 LY 3m ON m s ® s e d’ a rl le o r W YOU ASKED… JustRight Surgical delivered W r o e r l ld p ’s ta O s NL mm Y classic 5 IPEG…. Now it’s your turn RIGHT Come try these instruments in the Hands-On Lab: SIZE. High Fidelity Neonatal Course RIGHT for the Advanced Learner Tuesday May 24, 2016 FIT. 2:00pm - 6:00pm RIGHT 357 S. McCaslin, #120 | Louisville, CO 80027 CHOICE. 720-287-7130 | 866-683-1743 | www.justrightsurgical.com th IPEG’s 25 Annual Congress Welcome Message for Endosurgery in Children Dear Colleagues, May 24-28, 2016 Fukuoka, Japan On behalf of our IPEG family, I have the privilege to welcome you all to the 25th Congress of the THE HILTON FUKUOKA SEA HAWK International Pediatric Endosurgery Group (IPEG) in 810-8650, Fukuoka-shi, 2-2-3 Jigyohama, Fukuoka, Japan in May of 2016. Chuo-ku, Japan T: +81-92-844 8111 F: +81-92-844 7887 This will be a special Congress for IPEG. We have paired up with the Pacific Association of Pediatric Surgeons International Pediatric Endosurgery Group (IPEG) and the Japanese Society of Pediatric Surgeons to hold 11300 W. Olympic Blvd, Suite 600 a combined meeting that will add to our always-exciting Los Angeles, CA 90064 IPEG sessions a fantastic opportunity to interact and T: +1 310.437.0553 F: +1 310.437.0585 learn from the members of those two surgical societies. -

Liver Resections Combined with Closure of Loop Ileostomies: a Retrospective Analysis
Hindawi Publishing Corporation HPB Surgery Volume 2008, Article ID 501397, 5 pages doi:10.1155/2008/501397 Research Article Liver Resections Combined with Closure of Loop Ileostomies: A Retrospective Analysis Jeffrey T. Lordan, Angela T. Riga, and Nariman D. Karanjia Regional Hepato-Pancreatico-Biliary Unit for Surrey and Sussex, The Royal Surrey County Hospital, Egerton Road, Guildford, Surrey GU2 7XX, UK Correspondence should be addressed to Jeffrey T. Lordan, dr [email protected] Received 6 August 2008; Accepted 30 October 2008 Recommended by Olivier Farges Background. The management of patients with colorectal liver metastases and loop ileostomies remains controversial. This study was performed to assess the outcome of combined liver resection and loop ileostomy closure. Methods. Analysis of prospectively collected perioperative data, including morbidity and mortality, of 283 consecutive hepatectomies for colorectal liver metastases was undertaken. Consecutive liver resections were performed from 1996 to 2006 in one centre by a single surgeon (NDK). Fourteen of these patients had combined liver resection and ileostomy closure. Case-matched analysis was undertaken. Results.Six(2.2%) patients died in the hepatectomy only group and none died in the combined group. There was no difference in operative blood loss between the two groups (0.09). Perioperative morbidity was 36% in the combined group and 23% in the hepatectomy alone group (P = 0.33). Mean hospital stay was 14 days in the combined group and 11 days in the hepatectomy only group (P = 0.046). Case-matched analysis showed a significant increase in hospital stay (P = 0.03) and complications (P = 0.049) in the combined group. -

The Short Esophagus—Lengthening Techniques
10 Review Article Page 1 of 10 The short esophagus—lengthening techniques Reginald C. W. Bell, Katherine Freeman Institute of Esophageal and Reflux Surgery, Englewood, CO, USA Contributions: (I) Conception and design: RCW Bell; (II) Administrative support: RCW Bell; (III) Provision of the article study materials or patients: RCW Bell; (IV) Collection and assembly of data: RCW Bell; (V) Data analysis and interpretation: RCW Bell; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Reginald C. W. Bell. Institute of Esophageal and Reflux Surgery, 499 E Hampden Ave., Suite 400, Englewood, CO 80113, USA. Email: [email protected]. Abstract: Conditions resulting in esophageal damage and hiatal hernia may pull the esophagogastric junction up into the mediastinum. During surgery to treat gastroesophageal reflux or hiatal hernia, routine mobilization of the esophagus may not bring the esophagogastric junction sufficiently below the diaphragm to provide adequate repair of the hernia or to enable adequate control of gastroesophageal reflux. This ‘short esophagus’ was first described in 1900, gained attention in the 1950 where various methods to treat it were developed, and remains a potential challenge for the contemporary foregut surgeon. Despite frequent discussion in current literature of the need to obtain ‘3 or more centimeters of intra-abdominal esophageal length’, the normal anatomy of the phrenoesophageal membrane, the manner in which length of the mobilized esophagus is measured, as well as the degree to which additional length is required by the bulk of an antireflux procedure are rarely discussed. Understanding of these issues as well as the extent to which esophageal shortening is due to factors such as congenital abnormality, transmural fibrosis, fibrosis limited to the esophageal adventitia, and mediastinal fixation are needed to apply precise surgical technique. -

Quality and Health Outcomes Committee AGENDA
Oregon Health Authority Quality and Health Outcomes Committee AGENDA MEETING INFORMATION Meeting Date: March 13, 2017 Location: HSB Building Room 137A‐D, Salem, OR Parking: Map ◦ Phone: 503‐378‐5090 x0 Call in information: Toll free dial‐in: 888‐278‐0296 Participant Code: 310477 All meeting materials are posted on the QHOC website. Clinical Director Workgroup Time Topic Owner Materials -Speaker’s Contact Sheet (2) Welcome / -January Meeting Notes (2 – 12) 9:00 a.m. Mark Bradshaw Announcements -PH Update (13 – 14) -BH Directors Meeting Minutes (15 – 17) 9:10 a.m. Legislative Update Brian Nieubuurt -CCO and OHP Bills (18 – 20) Safina Koreishi 9:20 a.m. PH Modernization -Presentation (21 – 27) Cara Biddlecom 9:40 a.m. QHOC Planning Mark Bradshaw -Charter (28 – 29) 10:00 a.m. HERC Update Cat Livingston -HERC Materials (30 – 78) -Letter to FFS Providers re: Back Line Changes (79 – LARC and Back 80) 10:30 a.m. Implementation Check- Kim Wentz -Tapering Resource Guide (81 – 82) in -LARC Letter to Hospitals (83 – 84) -LARC Billing Tips (85) 10:45 a.m. BREAK Learning Collaborative -Agenda (86) -Panelist Bios (87) 11:00 a.m. OHIT: EDIE/PreManage -Presentations (88 – 114) -BH Care Coordination Process (115) 12:30 p.m. LUNCH Quality and Performance Improvement Session Jennifer QPI Update – 1:00 p.m. Johnstun Lisa Introductions Bui -Pre-Survey (116 - 118) 1:10 p.m. Measurement Training Colleen Reuland -Presentation (117 – 143) Transition to Small 2:10 p.m. All Table exercise 2:15 p.m. Small table Exercise All 2:45 p.m. -

Breast Cancer Screening and Chemoprevention
Management of Breast Diseases Ismail Jatoi Manfred Kaufmann (Eds.) Management of Breast Diseases Dr. Ismail Jatoi Prof. Dr. Manfred Kaufmann Head, Breast Care Center Breast Unit National Naval Medical Center Director, Women’s Hospital Uniformed Services University University of Frankfurt of the Health Sciences Theodor-Stern-Kai 7 4301 Jones Bridge Rd. 60590 Frankfurt Bethesda, MD 20814 Germany USA [email protected] [email protected] ISBN: 978-3-540-69742-8 e-ISBN: 978-3-540-69743-5 DOI: 10.1007/978-3-540-69743-5 Springer Heidelberg Dordrecht London New York Library of Congress Control Number: 2009934509 © Springer-Verlag Berlin Heidelberg 2010 This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lm or in any other way, and storage in data banks. Duplication of this publication or parts thereof is permitted only under the provisions of the German Copyright Law of September 9, 1965, in its current version, and permission for use must always be obtained from Springer. Violations are liable to prosecution under the German Copyright Law. The use of general descriptive names, registered names, trademarks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. Product liability: The publishers cannot guarantee the accuracy of any information about dosage and appli- cation contained in this book.