Toxicological Review of Quinoline (CAS No. 91-22-5) (PDF)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A New Synthesis of 1-Benzyl-1,2,3,4-Tetrahydroisoquinoline
A NEW SYNTHESIS OF 1-BENZYL-1,2,3,4-TETRAHYDROISOQUINOLINE By L. W. DEADY,*N, H. PIRZADA,*R. D. TOPSOM,"and J. M. BOBBITT~ [Manuscript received 5 March 19731 Abstract The synthesis of N-(2-bromoethy1)-N-(1,2-diphenylethy1)ammoniumbromide and its aluminium chloride catalysed decomposition to 1-benzyl-1,2,3,4-tetrahydro- isoquinoline is described. We have recently reported convenient preparations of tetrahydroquinolinesl (m = 0, n = 3) and tetrahydroisoquinolines2 (m = 1, n = 2) by the cyclization of compounds of type (1). 1-Benzyl-1,2,3,4-tetrahydroisoquinolineis the parent compound of an impor- tant class of alkaloids3 and methods of synthesis of this system are of considerable interest. Normally, the system has been prepared by ring closure between C 1 of the incipient isoquinoline and the aromatic ring, the so-called Bischler-Napieralski rea~tion,~although several new methods have been described and ~ummarized.~In theory, the ring system can be prepared by closure of C4 (as an aldehyde or blocked aldehyde) to the aromatic ring by a variation of the Pomeranz-Fritsch synthe~is,~,~ but there are several difficulties with intramolecular ring closures6 and only one successful synthesis has been reported.' In any case, such a synthesis results in oxygenation at C4 or some type of unsaturation in the isoquinoline ring. In this paper, we report a synthesis which is an extension of our previous work2 and which gives the tetrahydroisoquinoline ring directly in reasonable yield. Deoxybenzoin was used as the starting material in the synthesis of the required intermediate (2). Though the synthesis of (2) involved three steps it was experi- * Organic Chemistry Department, La Trobe University, Bundoora, Vic. -

Synthesis of Condensed 1,2,4-Triazolo-Heterocycles
Chemistry SYNTHESIS OF CONDENSED 1,2,4-TRIAZOLO-HETEROCYCLES MOHAMMED A. E. SHABAN ADEL Z. NASR MAMDOUH A. M. TAHA SUMMARY: Cyclization of 2-hydrazino-1, 3-benzothiazole, 2-hydrozinoquioline, 2-hydrazinolepidine, and 2-hydrazino-pyridine with one-carbon cyclizing agents such as triethyl orthoformate, ethyl chlorofor- mate, urea, phenylthiourea, and carbon disulfide gave 3-substituted-1,2,4-triazolo (3,4, -b) 1, 3-benzothia- zoles, 3-substituted-1,2,4-triazolo (4,3-a) quinolines, 3-substituted-1,2,4-triazolo (4,3-a) quinolines, 3-substituted-1,2,4-triazolo (4,3-a) lepidines and 3-substituted-1,2,4-triazolo (4,3-a) pyridines respectively. Reactions with acetic acid and acetic anhydride gave the corresponding acetyl hydrazines which were cyclized to the 3-methyl 1,2,4-triazolo-heterocyles. Ring closure with phenyl isocyanate and phenyl isothio- cyanate, gave the intermediate 4-phenylsemicarbazides and 4-phenylthiosemicarbazides which, upon fusion, afforded the corresponding 3-oxo- and 3-thioxo-1,2,4-triazolo-heterocyles. The 3-oxo-compounds were also obtained when 2-chloroquinoloni or 2-chlorolepidine was fused with semicarbazide hydrochloride. Key Words: Synthesis, amidrazones, triazolo-heterocycles. INTRODUCTION The synthesis and biological activities of condensed In an attempt to prepare 3-methyl-1,2,4-triazolo (3,4-b) 1,2,4-triazolo (3,4-z) heterocyles have recently been 1,3-benzothiazole (5a) by heating 2-hydrazino-1, 3- reviewed (14). Several condendes 1,2,4-triazolo-hetero- benzothiazole (1a) with an excess of acetic acid or acetic cyles exhibit various biological activities such as fungicidal anhydride, 1,1,2-triacetyl-2-(1,3-benzothiazol-2-yl) hyd- (1,9) bactericidal (1,9) analgesic (4,7,10) anxiolytic (8) razine (3a) was obtained. -
) Synthesis of Quinoline and Derivatives1)
Faculty of Science Damietta University Chemistry Department An Essay on : Evaluation of the Synthesis, Reactions and Biological Activities of Quinolines _______________________________________________________________________ ____________________________________________________________ Presented BY MOHAMED ELNEKETY b.s.C student (special 2016 chemistry) Acknowledgment First my thank and gratitude to Allah I am greatly indebted to Prof.Dr : FAWZIA EL-ABLACK Professor of Organic Chemistry Chemistry Department Faculty of Science Damietta University To his supervision on my research. He taught me How to design a research plan and how to write it. I appreciate your help, guiding and encouragement. Again many thanks for what you have done for me. Fourth year Chemistry Department 2015 - 2016 Contents : Page Introduction..……………………………………..…………………….…..3 (1) Synthesis of Quinolines………………….………….…….…....5 1.1 Skraup reaction…………………………………………………..5 1.2 Combes quinoline synthesis…………………………….…….…6 1.3 Doebner reaction..………………………………..…….………..6 1.4 Doebner–Miller reaction …………………………….………….7 1.5 Knorr quinoline synthesis…………………………….…………7 1.6 Friedlaender Synthesis……………………………….………….8 1.7 Pfitzinger Synthesis………………………………….…………..8 1.8 Green preparation of quinolone……………………….……….9 1.9 Quinolines by Forming the N–C-2 Bond……………….……...11 1.10 From Aldehyde and Aniline……………………………………11 1.11 By condensation reaction of ortho-acylanilines and Alkenyl iodides…………………………………………….……12 1.12 By dehydrogenation of tetrahydroquinolines………….……..12 1.13 By cyclization of 2-ethynylanilines -

Nitroaromatic Antibiotics As Nitrogen Oxide Sources
Review biomolecules Nitroaromatic Antibiotics as Nitrogen Oxide Sources Review Allison M. Rice, Yueming Long and S. Bruce King * Nitroaromatic Antibiotics as Nitrogen Oxide Sources Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; Allison M. Rice , Yueming [email protected] and S. Bruce (A.M.R.); King [email protected] * (Y.L.) * Correspondence: [email protected]; Tel.: +1-336-702-1954 Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; [email protected]: Nitroaromatic (A.M.R.); [email protected] antibiotics (Y.L.) show activity against anaerobic bacteria and parasites, finding * Correspondence: [email protected]; Tel.: +1-336-702-1954 use in the treatment of Heliobacter pylori infections, tuberculosis, trichomoniasis, human African trypanosomiasis, Chagas disease and leishmaniasis. Despite this activity and a clear need for the Abstract: Nitroaromatic antibiotics show activity against anaerobic bacteria and parasites, finding usedevelopment in the treatment of new of Heliobacter treatments pylori forinfections, these conditio tuberculosis,ns, the trichomoniasis, associated toxicity human Africanand lack of clear trypanosomiasis,mechanisms of action Chagas have disease limited and their leishmaniasis. therapeutic Despite development. this activity Nitroaro and a clearmatic need antibiotics for require thereductive development bioactivation of new treatments for activity for theseand this conditions, reductive the associatedmetabolism toxicity can convert -

Electron Density Studies on Quinoline Analogs of N,N'-Dimcthy\-P- Phenylazoaniline
[CANCER RESEARCH 30, 2089-2090, August 1970] Electron Density Studies on Quinoline Analogs of N,N'-Dimcthy\-p- phenylazoaniline Ellis V. Brown and William H. Kipp Department of Chemistry, University of Kentucky, Lexington, Kentucky 40506 SUMMARY azobenzenes. The K for the addition of 1 proton to the quinolinium salt would be determined (designated pKfl). The This paper continues the study of the relationship between amino nitrogen of the quinolinium salt would be quater- electron density and carcinogenic activity for compounds nized, and then the K for the addition of a proton to the azo related to p-dimethylaminoazobenzene (Cancer Res., 29: nitrogen in the presence of 2 positive charges would be 1341-1344, 1969) and reports on the seven p-dimethyl- determined. It would then be possible to determine KT, aminophenylazoquinolines. A relationship was found pKam, and pKaz in the manner described in the previous between carcinogenic activity and the pKfl of the amino paper (Chart 1). nitrogen in these compounds, and in this new series a H relationship also was found for carcinogenic activity and the *;]-«•I pKa of the azo nitrogen. INTRODUCTION CH, C-H N -N=NC,H.N(CH,), ^=îiC_H,N - N' - "UC,H,N (CH, ) We have previously reported (2) on the resolution of KT y o o 4 J ¿ y o o 4 J ¿ into pKam and pKaz for a series of alkyl derivatives of AVV-dimethyl-p-phenylazoaniline. KT is the tautomerie a2 equilibrium between the aniline nitrogen and the azo nitro gens in 20% ethanol-sulfuric acid solution described by Isak's and Jaffe (5). -

UV Photolysis of Quinoline in Interstellar Ice Analogs
Meteoritics & Planetary Science 41, Nr 5, 785–796 (2006) Abstract available online at http://meteoritics.org UV photolysis of quinoline in interstellar ice analogs Jamie E. ELSILA1*, Matthew R. HAMMOND2, Max P. BERNSTEIN1, Scott A. SANDFORD1, and Richard N. ZARE2 1NASA Ames Research Center, MS 245-6, Moffett Field, California 94035–1000, USA 2Department of Chemistry, Stanford University, Stanford, California 94305–5080, USA *Corresponding author. E-mail: [email protected] (Received 16 November 2005; revision accepted 03 February 2006) Abstract–The polycyclic aromatic nitrogen heterocycle (PANH) quinoline (C9H7N) was frozen at 20 K in interstellar ice analogs containing either pure water or water mixed with methanol or methane and exposed to ultraviolet (UV) radiation. Upon warming, the photolysis products were analyzed by high-performance liquid chromatography and nanoscale liquid chromatography-electrospray ionization mass spectrometry. A suite of hydroxyquinolines, which were formed by the addition of oxygen atoms to quinoline, was observed as the primary product in all the ices. Quinoline N oxide was not formed, but five hydroxyquinoline isomers were produced with no clear dominance of one isomer. Reduction products, formed by hydrogen atom addition, were also created. Ices created at 20 K with H2O: quinoline ratios of 10:1 to 100:1 showed similar product distributions to those at 122 K, with no apparent temperature or concentration dependence. Increasing the UV dose led to a decrease in overall yield, indicating that quinoline and its products may be photo-destroyed. Methylquinolines were formed upon photolysis of the methanol- and methane-containing ices. In addition, possible methoxyquinolines or quinoline methylene alcohols were formed in the methanol- containing ice, while methylhydroxyquinolines were created in the methane-containing ice. -

Heterocyclic Chemistrychemistry
HeterocyclicHeterocyclic ChemistryChemistry Professor J. Stephen Clark Room C4-04 Email: [email protected] 2011 –2012 1 http://www.chem.gla.ac.uk/staff/stephenc/UndergraduateTeaching.html Recommended Reading • Heterocyclic Chemistry – J. A. Joule, K. Mills and G. F. Smith • Heterocyclic Chemistry (Oxford Primer Series) – T. Gilchrist • Aromatic Heterocyclic Chemistry – D. T. Davies 2 Course Summary Introduction • Definition of terms and classification of heterocycles • Functional group chemistry: imines, enamines, acetals, enols, and sulfur-containing groups Intermediates used for the construction of aromatic heterocycles • Synthesis of aromatic heterocycles • Carbon–heteroatom bond formation and choice of oxidation state • Examples of commonly used strategies for heterocycle synthesis Pyridines • General properties, electronic structure • Synthesis of pyridines • Electrophilic substitution of pyridines • Nucleophilic substitution of pyridines • Metallation of pyridines Pyridine derivatives • Structure and reactivity of oxy-pyridines, alkyl pyridines, pyridinium salts, and pyridine N-oxides Quinolines and isoquinolines • General properties and reactivity compared to pyridine • Electrophilic and nucleophilic substitution quinolines and isoquinolines 3 • General methods used for the synthesis of quinolines and isoquinolines Course Summary (cont) Five-membered aromatic heterocycles • General properties, structure and reactivity of pyrroles, furans and thiophenes • Methods and strategies for the synthesis of five-membered heteroaromatics -

Progressive Insights Into the Pharmacological Importance of Isoquinoline Derivatives in Modern Therapeutics
International Journal of Current Research and Review Review Article DOI: http://dx.doi.org/10.31782/IJCRR.2021.13421 Progressive Insights into the Pharmacological Importance of Isoquinoline Derivatives in Modern IJCRR Therapeutics Section: Healthcare ISI Impact Factor (2019-20): 1.628 1 1 1 IC Value (2019): 90.81 Kishor R. Danao , Pooja M. Malghade , Debarshi Kar Mahapatra , SJIF (2020) = 7.893 Meha N. Motiwala2, Ujwala N. Mahajan3 1 2 Copyright@IJCRR Department of Pharmaceutical Chemistry, Dadasaheb Balpande College of Pharmacy, Nagpur 440037, Maharashtra, India; Department of Pharmacognosy, Dadasaheb Balpande College of Pharmacy, Nagpur 440037, Maharashtra, India; 3Department of Quality Assurance, Dadasa- heb Balpande College of Pharmacy, Nagpur 440037, Maharashtra, India. ABSTRACT Isoquinoline (ISOQ) is a heterocyclic aromatic organic compound composed of a benzene ring fused to a pyridine ring, referred to as benzopyridines. The chemical formula is C9H7N with a molar mass of 129.162 g/mol. This ISOQ ring derives from the natural aromatic amino acid tyrosine. It is weak alkaline in nature but is more basic than quinoline. It appears as a yellowish oily liquid, having an unpleasant odour, hygroscopic when solid, has a density of 1.099 g/cm3, a melting point of 26°C to 28°C (79°F to 82°F), the boiling point of 242°C (468°F), and dipole moment of 2.49. In the preparation of this review article, a widespread examination of the published literature in varied pharmaceutical and medical databases such as PubMed, Google Scholar, etc. was fruitfully carried out and categorized consequently. The imperative review revealed the less known biological (anti-fungal, anti-Parkinsonism, anti-tubercular, anti-tumour, anti-glaucoma, anti-Alzheimer’s disease, anti-viral, anti-bacterial, anti-diabetic, anti-malarial, etc.) potentials of ISOQ (an important class of chemical compounds) and their synthetic derivatives. -

Searching for New Biologically Active Compounds Derived from Isoquinoline Alkaloids †
Proceeding Paper Searching for New Biologically Active Compounds Derived from Isoquinoline Alkaloids † Anna Kmieciak 1, Marta Ćwiklińska 1, Karolina Jeżak 1, Afef Shili 2 and Marek P. Krzemiński 1,* 1 Faculty of Chemistry, Nicolaus Copernicus University, 87-100 Toruń, Poland; [email protected] (A.K.); [email protected] (M.Ć.); [email protected] (K.J.) 2 Chemistry Department, Faculty of Sciences of Sfax, University of Sfax, Sfax 3029, Tunisia; [email protected] * Correspondence: [email protected] † Presented at the 24th International Electronic Conference on Synthetic Organic Chemistry, 15 November–15 December 2020; Available online: https://ecsoc-24.sciforum.net/. Abstract: Many isoquinoline alkaloids are biologically active compounds and successfully used as pharmaceuticals. Compounds belonging to the isoquinolines and tetrahydroisoquinolines (TIQs) can be used as anesthetics, antihypertensive drugs, antiviral agents, and vasodilators. In the presented studies, the search for new compounds and synthesis of tetrahydroisoquinoline alkaloid derivatives was undertaken. Several dihydroisoquinolines were synthesized by Bishler–Napieralski reaction from the corresponding amides. Dihydroisoquinolines were reduced with sodium borohydride to obtain racemic tetrahydroisoquinolines. Asymmetric reduction of selected 3,4-dihydroisoquinolines was attempted with borane in the presence of chiral terpene spiroboranes. Keywords: isoquinoline; alkaloids; biologically active compound Citation: Kmieciak, A.; Ćwiklińska, M.; Jeżak, K.; Shili, A.; Krzemiński, M.P. Searching for New Biologically 1. Introduction Active Compounds Derived from Isoquinoline Alkaloids. Chem. Proc. Isoquinoline and its derivatives are used as starting materials in the synthesis of 2021, 3, 97. https://doi.org/10.3390/ dyes, insecticides, and pharmaceuticals. Tetrahydroisoquinoline (TIQ) is one of many ecsoc-24-08417 representatives of N-heterocyclic compounds. -

Dissociation Constants of Organic Acids and Bases
DISSOCIATION CONSTANTS OF ORGANIC ACIDS AND BASES This table lists the dissociation (ionization) constants of over pKa + pKb = pKwater = 14.00 (at 25°C) 1070 organic acids, bases, and amphoteric compounds. All data apply to dilute aqueous solutions and are presented as values of Compounds are listed by molecular formula in Hill order. pKa, which is defined as the negative of the logarithm of the equi- librium constant K for the reaction a References HA H+ + A- 1. Perrin, D. D., Dissociation Constants of Organic Bases in Aqueous i.e., Solution, Butterworths, London, 1965; Supplement, 1972. 2. Serjeant, E. P., and Dempsey, B., Ionization Constants of Organic Acids + - Ka = [H ][A ]/[HA] in Aqueous Solution, Pergamon, Oxford, 1979. 3. Albert, A., “Ionization Constants of Heterocyclic Substances”, in where [H+], etc. represent the concentrations of the respective Katritzky, A. R., Ed., Physical Methods in Heterocyclic Chemistry, - species in mol/L. It follows that pKa = pH + log[HA] – log[A ], so Academic Press, New York, 1963. 4. Sober, H.A., Ed., CRC Handbook of Biochemistry, CRC Press, Boca that a solution with 50% dissociation has pH equal to the pKa of the acid. Raton, FL, 1968. 5. Perrin, D. D., Dempsey, B., and Serjeant, E. P., pK Prediction for Data for bases are presented as pK values for the conjugate acid, a a Organic Acids and Bases, Chapman and Hall, London, 1981. i.e., for the reaction 6. Albert, A., and Serjeant, E. P., The Determination of Ionization + + Constants, Third Edition, Chapman and Hall, London, 1984. BH H + B 7. Budavari, S., Ed., The Merck Index, Twelth Edition, Merck & Co., Whitehouse Station, NJ, 1996. -

Table II. EPCRA Section 313 Chemical List for Reporting Year 2007 (Including Toxic Chemical Categories)
Table II. EPCRA Section 313 Chemical List For Reporting Year 2007 (including Toxic Chemical Categories) Individually listed EPCRA Section 313 chemicals with CAS numbers are arranged alphabetically starting on page II-3. Following the alphabetical list, the EPCRA Section 313 chemicals are arranged in CAS number order. Covered chemical categories follow. Certain EPCRA Section 313 chemicals listed in Table II have parenthetic “qualifiers.” These qualifiers indicate that these EPCRA Section 313 chemicals are subject to the section 313 reporting requirements if manufactured, processed, or otherwise used in a specific form or when a certain activity is performed. The following chemicals are reportable only if they are manufactured, processed, or otherwise used in the specific form(s) listed below: Chemical CAS Number Qualifier Aluminum (fume or dust) 7429-90-5 Only if it is a fume or dust form. Aluminum oxide (fibrous forms) 1344-28-1 Only if it is a fibrous form. Ammonia (includes anhydrous ammonia and aqueous ammonia 7664-41-7 Only 10% of aqueous forms. 100% of from water dissociable ammonium salts and other sources; 10 anhydrous forms. percent of total aqueous ammonia is reportable under this listing) Asbestos (friable) 1332-21-4 Only if it is a friable form. Hydrochloric acid (acid aerosols including mists, vapors, gas, 7647-01-0 Only if it is an aerosol form as fog, and other airborne forms of any particle size) defined. Phosphorus (yellow or white) 7723-14-0 Only if it is a yellow or white form. Sulfuric acid (acid aerosols including mists, vapors, gas, fog, and 7664-93-9 Only if it is an aerosol form as other airborne forms of any particle size) defined. -
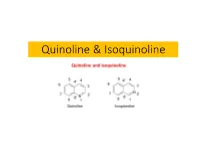
Quinoline & Isoquinoline
Quinoline & Isoquinoline It is a chemical reaction of 2-aminobenzaldehydes with ketones to form quinoline derivatives. It is named after German chemist Paul Friedländer (1857–1923). Two viable reaction mechanisms exist for this reaction. In the first mechanism 2-amino substituted carbonyl compound 1 and carbonyl compound 2 react in a rate-limiting step to aldol adduct 3. This intermediate loses water in an elimination reaction to unsaturated carbonyl compound 4 and then loses water again in imine formation to quinoline 7. In the second mechanism the first step is Schiff base formation to 5 followed by Aldol reaction to 6 and elimination to 7. KNORR QUINOLINE SYNTHESIS The Knorr quinoline synthesis is an intramolecular organic reaction converting a β-ketoanilide to a 2- hydroxyquinoline using sulfuric acid. This reaction was first described by Ludwig Knorr (1859–1921) in 1886. The reaction is a type of electrophilic aromatic substitution accompanied by elimination of water. A 1964 study found that with certain reaction conditions formation of a 4-hydroxyquinoline is a competing reaction. For instance, the compound benzoylacetanilide (1) forms the 2-hydroxyquinoline (2) in a large excess of polyphosphoric acid (PPA) but 4-hydroxyquinoline 3 when the amount of PPA is small. A reaction mechanism identified a N,O- dicationic intermediate A with excess acid capable of ring-closing and a monocationic intermediate B which fragments to aniline and (ultimately to) acetophenone. Aniline reacts with another equivalent of benzoylacetanilide before forming the 4-hydroxyquinoline. Formation of α-hydroxyquinolines from β-ketoesters and arylamines above 100°. The intermediate anilide undergoes cyclization by dehydration with concentrated sulfuric acid: DOEBNER-MILLER SYNTHESIS The Doebner–Miller reaction is the organic reaction of an aniline with α,β-unsaturated carbonyl compounds to form quinolines.