Androgens and Androgen Receptor Actions on Bone Health and Disease: from Androgen Deficiency to Androgen Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Androgen Receptor: a Complex Therapeutic Target for Breast Cancer
cancers Review Androgen Receptor: A Complex Therapeutic Target for Breast Cancer Ramesh Narayanan 1 and James T. Dalton 2,* 1 Department of Medicine, University of Tennessee Health Science Center, Memphis, TN 38103, USA; [email protected] 2 College of Pharmacy, University of Michigan, Ann Arbor, MI 48109, USA * Correspondence: [email protected] Academic Editor: Emmanuel S. Antonarakis Received: 28 September 2016; Accepted: 23 November 2016; Published: 2 December 2016 Abstract: Molecular and histopathological profiling have classified breast cancer into multiple sub-types empowering precision treatment. Although estrogen receptor (ER) and human epidermal growth factor receptor (HER2) are the mainstay therapeutic targets in breast cancer, the androgen receptor (AR) is evolving as a molecular target for cancers that have developed resistance to conventional treatments. The high expression of AR in breast cancer and recent discovery and development of new nonsteroidal drugs targeting the AR provide a strong rationale for exploring it again as a therapeutic target in this disease. Ironically, both nonsteroidal agonists and antagonists for the AR are undergoing clinical trials, making AR a complicated target to understand in breast cancer. This review provides a detailed account of AR’s therapeutic role in breast cancer. Keywords: androgen receptor; breast cancer; selective androgen receptor modulator (SARM); estrogen receptor; triple-negative breast cancer (TNBC) 1. Introduction Over 240,000 women will develop breast cancer and ~40,000 will die from the disease in the United States in 2016 [1]. Globally, about 1.7 million women were diagnosed with breast cancer in 2012, emphasizing the urgent need for effective and safe therapeutic approaches [2]. -

Sex Hormones Related Ocular Dryness in Breast Cancer Women
Journal of Clinical Medicine Review Sex Hormones Related Ocular Dryness in Breast Cancer Women Antonella Grasso 1, Antonio Di Zazzo 2,* , Giuseppe Giannaccare 3 , Jaemyoung Sung 4 , Takenori Inomata 4 , Kendrick Co Shih 5 , Alessandra Micera 6, Daniele Gaudenzi 2, Sara Spelta 2 , Maria Angela Romeo 7, Paolo Orsaria 1, Marco Coassin 2 and Vittorio Altomare 1 1 Breast Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (A.G.); [email protected] (P.O.); [email protected] (V.A.) 2 Ophthalmology Operative Complex Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (D.G.); [email protected] (S.S.); [email protected] (M.C.) 3 Department of Ophthalmology, University Magna Graecia of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of Ophthalmology, School of Medicine, Juntendo University, 1130033 Tokyo, Japan; [email protected] (J.S.); [email protected] (T.I.) 5 Department of Ophthalmology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; [email protected] 6 Research and Development Laboratory for Biochemical, Molecular and Cellular Applications in Ophthalmological Sciences, IRCCS–Fondazione Bietti, 00198 Rome, Italy; [email protected] 7 School of Medicine, Humanitas University, 20089 Milan, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-06225418893; Fax: +39-9622541456 Abstract: Background: Dry eye syndrome (DES) is strictly connected to systemic and topical sex hor- mones. Breast cancer treatment, the subsequent hormonal therapy, the subsequent hyperandrogenism and the early sudden menopause, may be responsible for ocular surface system failure and its clinical Citation: Grasso, A.; Di Zazzo, A.; manifestation as dry eye disease. -
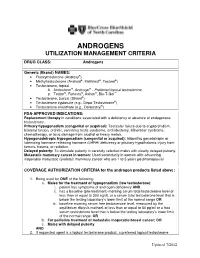
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

Background Briefing Document from the Consortium of Sponsors for The
BRIEFING BOOK FOR Pediatric Advisory Committee (PAC) Prepared by Alan Rogol, M.D., Ph.D. Prepared for Consortium of Sponsors Meeting Date: April 8th, 2019 TABLE OF CONTENTS LIST OF FIGURES ................................................... ERROR! BOOKMARK NOT DEFINED. LIST OF TABLES ...........................................................................................................................4 1. INTRODUCTION AND BACKGROUND FOR THE MEETING .............................6 1.1. INDICATION AND USAGE .......................................................................................6 2. SPONSOR CONSORTIUM PARTICIPANTS ............................................................6 2.1. TIMELINE FOR SPONSOR ENGAGEMENT FOR PEDIATRIC ADVISORY COMMITTEE (PAC): ............................................................................6 3. BACKGROUND AND RATIONALE .........................................................................7 3.1. INTRODUCTION ........................................................................................................7 3.2. PHYSICAL CHANGES OF PUBERTY ......................................................................7 3.2.1. Boys ..............................................................................................................................7 3.2.2. Growth and Pubertal Development ..............................................................................8 3.3. AGE AT ONSET OF PUBERTY.................................................................................9 3.4. -

Serum Androgen Profiles in Women with Premature Ovarian Insufficiency: a Systematic Review and Meta-Analysis
Menopause: The Journal of The North American Menopause Society Vol. 26, No. 1, pp. 78-93 DOI: 10.1097/GME.0000000000001161 ß 2018 The Author(s). Published by Wolters Kluwer Health, Inc. on behalf of The North American Menopause Society. Serum androgen profiles in women with premature ovarian insufficiency: a systematic review and meta-analysis Midhun Soman, MS,1 Li-Cong Huang, MD,1 Wen-Hui Cai, MS,1 Jun-Bi Xu, MS,1 Jun-Yao Chen, MD,1 Ren-Ke He, MS,1 Heng-Chao Ruan, MS,1,2,3 Xiang-Rong Xu, MD,1,2,3 Zhi-Da Qian, MD,1,2,3,4 and Xiao-Ming Zhu, MD, PhD1,2,3 Abstract Objective: This meta-analysis aims to investigate serum androgen profiles (testosterone, dehydroepiandroster- one sulfate, androstenedione, and sex hormone-binding globulin) in women with premature ovarian failure and to establish if there is evidence of diminished androgen levels in these women. Methods: Various Internet sources of PubMed, Cochrane library, and Medline were searched systematically until February, 2018. Out of a pool of 2,461 studies, after applying the inclusion/exclusion criterion, 14, 8, 10, and 9 studies were chosen for testosterone, dehydroepiandrosterone sulfate, androstenedione, and sex hormone-binding globulin, respectively, for this meta-analysis. The effect measure was the standardized mean difference with 95% confidence interval (95% CI) in a random-effects model. Results: The testosterone concentrations in premature ovarian insufficiency were compared with fertile controls: stamdard mean difference (IV, random, 95% CI) À0.73 [À0.99, À0.46], P value < 0.05. The dehydroepiandrosterone sulfate concentrations in premature ovarian insufficiency compared to fertile controls: standard mean difference (IV, random, 95% CI) À0.65 [À0.92, À0.37], P value < 0.05. -

Cancer Palliative Care and Anabolic Therapies
Cancer Palliative Care and Anabolic Therapies Aminah Jatoi, M.D. Professor of Oncology Mayo Clinic, Rochester, Minnesota USA • 2 Androgens • Creatine • Comments von Haehling S, et al, 2017 Oxandrolone: androgen that causes less virilization oxandrolone RANDOMIZE megestrol acetate #1: Oxandrolone (Lesser, et al, ASCO abstract 9513; 2008) • N=155 patients receiving chemotherapy • oxandrolone (10 mg twice a day x 12 weeks) versus megestrol acetate (800 mg/day x 12 weeks) • oxandrolone led to – a non-statistically significant increase in lean body mass (bioelectrical impedance) at 12 weeks (2.67 versus 0.82 pounds with megestrol acetate, p = 0.12), but – a decrease in overall weight as compared with megestrol acetate (-3.3 versus +5.8 pounds, respectively). • more oxandrolone patients dropped out prior to completing 12 weeks (63% versus 39 %). #2: Oxandrolone (von Roenn, et al, ASCO, 2003) • N=131 • Single arm • 81% of patients gained/maintained weight • Safe (PRIMARY ENDPOINT): 19% edema; 18% dyspnea; mild liver function test abnormalities #3: Oxandrolone: placebo controlled trial • results unknown SUMMARY OF OXANDROLONE: • Multiple studies (not yet peer-reviewed) • Hints of augmentation of lean tissue • High drop out in the phase 3 oxandrolone arm raises concern Enobosarm: selective androgen receptor modulator (less virilizing) ENOBOSARM RANDOMIZE* PLACEBO *All patients had non-small cell lung cancer, and chemotherapy was given concomittantly. percentage of subjects at day 84 with stair climb power change >=10% from their baseline value percentage of subjects at day 84 with lean body mass change >=0% from their baseline value SUMMARY OF ENOBOSARM: • Leads to incremental lean body mass, but functionality not demonstrated • Pivotal registration trial (not yet peer- reviewed (but FDA-reviewed….)) • 2 Androgens • Creatine • Comments Creatine: an amino acid derivative This study was funded by R21CA098477 and the Alliance for Clinical Trials NCORP grant. -

Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’S Time to Sound the Alarm
Review Article Health promotion, disease prevention, and lifestyle pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health 2020 Jul 38(3): 323-337 https://doi.org/10.5534/wjmh.200012 Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’s Time to Sound the Alarm Abdulmaged M. Traish Department of Urology, Boston University School of Medicine, Boston, MA, USA 5α-dihydrotestosterone (5α-DHT) is the most potent natural androgen. 5α-DHT elicits a multitude of physiological actions, in a host of tissues, including prostate, seminal vesicles, hair follicles, skin, kidney, and lacrimal and meibomian glands. How- ever, the physiological role of 5α-DHT in human physiology, remains questionable and, at best, poorly appreciated. Recent emerging literature supports a role for 5α-DHT in the physiological function of liver, pancreatic β-cell function and survival, ocular function and prevention of dry eye disease and kidney physiological function. Thus, inhibition of 5α-reductases with finasteride or dutasteride to reduce 5α-DHT biosynthesis in the course of treatment of benign prostatic hyperplasia (BPH) or male pattern hair loss, known as androgenetic alopecia (AGA) my induces a novel form of tissue specific androgen deficien- cy and contributes to a host of pathophysiological conditions, that are yet to be fully recognized. Here, we advance the con- cept that blockade of 5α-reductases by finasteride or dutasteride in a mechanism-based, irreversible, inhabitation of 5α-DHT biosynthesis results in a novel state of androgen deficiency, independent of circulating testosterone levels. Finasteride and dutasteride are frequently prescribed for long-term treatment of lower urinary tract symptoms in men with BPH and in men with AGA. -
Mice Subjected to Ap2-Cre Mediated Ablation of Microsomal Triglyceride Transfer Protein Are Resistant to High Fat Diet Induced Obesity Ahmed Bakillah1,2* and M
Bakillah and Hussain Nutrition & Metabolism (2016) 13:1 DOI 10.1186/s12986-016-0061-6 RESEARCH Open Access Mice subjected to aP2-Cre mediated ablation of microsomal triglyceride transfer protein are resistant to high fat diet induced obesity Ahmed Bakillah1,2* and M. Mahmood Hussain1,2,3 Abstract Background: Microsomal triglyceride transfer protein (MTP) is essential for the assembly of lipoproteins. MTP has been shown on the surface of lipid droplets of adipocytes; however its function in adipose tissue is not well defined. We hypothesized that MTP may play critical role in adipose lipid droplet formation and expansion. Methods: Plasmids mediated overexpression and siRNA mediated knockdown of Mttp gene were performed in 3T3-L1 pre-adipocytes to evaluate the effects of MTP on cell differentiation and triglyceride accumulation. Adipose- specific knockdown of MTP was achieved in mice bybreeding MTP floxed (Mttpfl/fl) mice with aP2-Cre recombinase transgenic mice. Adipose-specific MTP deficient (A-Mttp-/-) mice were fed 60 % high-fat diet (HFD), and the effects of MTP knockdown on body weight, body fat composition, plasma and tissues lipid composition, glucose metabolism, lipogenesis and intestinal absorption was studied. Lipids were measured in total fasting plasma and size fractionated plasma using colorimetric assays. Gene expression was investigated by Real-Time quantitative PCR. All data was assessed using t-test, ANOVA. Results: MTP expression increased during early differentiation in 3T3-L1 cells, and declined later. The increases in MTP expression preceded PPARγ expression. MTP overexpression enhanced lipid droplets formation, and knockdown attenuated cellular lipid accumulation. These studies indicated that MTP positively affects adipogenesis. -

EAU Pocket Guidelines on Male Hypogonadism 2013
GUIDELINES ON MALE HYPOGONADISM G.R. Dohle (chair), S. Arver, C. Bettocchi, S. Kliesch, M. Punab, W. de Ronde Introduction Male hypogonadism is a clinical syndrome caused by andro- gen deficiency. It may adversely affect multiple organ func- tions and quality of life. Androgens play a crucial role in the development and maintenance of male reproductive and sexual functions. Low levels of circulating androgens can cause disturbances in male sexual development, resulting in congenital abnormalities of the male reproductive tract. Later in life, this may cause reduced fertility, sexual dysfunc- tion, decreased muscle formation and bone mineralisation, disturbances of fat metabolism, and cognitive dysfunction. Testosterone levels decrease as a process of ageing: signs and symptoms caused by this decline can be considered a normal part of ageing. However, low testosterone levels are also associated with several chronic diseases, and sympto- matic patients may benefit from testosterone treatment. Androgen deficiency increases with age; an annual decline in circulating testosterone of 0.4-2.0% has been reported. In middle-aged men, the incidence was found to be 6%. It is more prevalent in older men, in men with obesity, those with co-morbidities, and in men with a poor health status. Aetiology and forms Male hypogonadism can be classified in 4 forms: 1. Primary forms caused by testicular insufficiency. 2. Secondary forms caused by hypothalamic-pituitary dysfunction. 164 Male Hypogonadism 3. Late onset hypogonadism. 4. Male hypogonadism due to androgen receptor insensitivity. The main causes of these different forms of hypogonadism are highlighted in Table 1. The type of hypogonadism has to be differentiated, as this has implications for patient evaluation and treatment and enables identification of patients with associated health problems. -

UFC PROHIBITED LIST Effective June 1, 2021 the UFC PROHIBITED LIST
UFC PROHIBITED LIST Effective June 1, 2021 THE UFC PROHIBITED LIST UFC PROHIBITED LIST Effective June 1, 2021 PART 1. Except as provided otherwise in PART 2 below, the UFC Prohibited List shall incorporate the most current Prohibited List published by WADA, as well as any WADA Technical Documents establishing decision limits or reporting levels, and, unless otherwise modified by the UFC Prohibited List or the UFC Anti-Doping Policy, Prohibited Substances, Prohibited Methods, Specified or Non-Specified Substances and Specified or Non-Specified Methods shall be as identified as such on the WADA Prohibited List or WADA Technical Documents. PART 2. Notwithstanding the WADA Prohibited List and any otherwise applicable WADA Technical Documents, the following modifications shall be in full force and effect: 1. Decision Concentration Levels. Adverse Analytical Findings reported at a concentration below the following Decision Concentration Levels shall be managed by USADA as Atypical Findings. • Cannabinoids: natural or synthetic delta-9-tetrahydrocannabinol (THC) or Cannabimimetics (e.g., “Spice,” JWH-018, JWH-073, HU-210): any level • Clomiphene: 0.1 ng/mL1 • Dehydrochloromethyltestosterone (DHCMT) long-term metabolite (M3): 0.1 ng/mL • Selective Androgen Receptor Modulators (SARMs): 0.1 ng/mL2 • GW-1516 (GW-501516) metabolites: 0.1 ng/mL • Epitrenbolone (Trenbolone metabolite): 0.2 ng/mL 2. SARMs/GW-1516: Adverse Analytical Findings reported at a concentration at or above the applicable Decision Concentration Level but under 1 ng/mL shall be managed by USADA as Specified Substances. 3. Higenamine: Higenamine shall be a Prohibited Substance under the UFC Anti-Doping Policy only In-Competition (and not Out-of- Competition). -

Diverse Pathomechanisms Leading to the Breakdown of Cellular Estrogen Surveillance and Breast Cancer Development: New Therapeutic Strategies
Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2014 Volume: 8 Drug Design, Development and Therapy Dovepress Running head verso: Suba Running head recto: Diverse pathomechanisms leading to breast cancer development open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DDDT.S70570 Open Access Full Text Article REVIEW Diverse pathomechanisms leading to the breakdown of cellular estrogen surveillance and breast cancer development: new therapeutic strategies Zsuzsanna Suba Abstract: Recognition of the two main pathologic mechanisms equally leading to breast cancer National Institute of Oncology, development may provide explanations for the apparently controversial results obtained by sexual Budapest, Hungary hormone measurements in breast cancer cases. Either insulin resistance or estrogen receptor (ER) defect is the initiator of pathologic processes and both of them may lead to breast cancer development. Primary insulin resistance induces hyperandrogenism and estrogen deficiency, but during these ongoing pathologic processes, ER defect also develops. Conversely, when estrogen resistance is the onset of hormonal and metabolic disturbances, initial counteraction is For personal use only. hyperestrogenism. Compensatory mechanisms improve the damaged reactivity of ERs; however, their failure leads to secondary insulin resistance. The final stage of both pathologic pathways is the breakdown of estrogen surveillance, leading to breast cancer development. Among pre- menopausal breast cancer cases, insulin resistance is the preponderant initiator of alterations with hyperandrogenism, which is reflected by the majority of studies suggesting a causal role of hyperandrogenism in breast cancer development. In the majority of postmenopausal cases, tumor development may also be initiated by insulin resistance, while hyperandrogenism is typi- cally coupled with elevated estrogen levels within the low postmenopausal hormone range. -

139 Normal Bone Density in Male
SEPTEMBER-OCTOBER REV. HOSP. CLÍN. FAC. MED. S. PAULO 56(5):139-142, 2001 NORMAL BONE DENSITY IN MALE PSEUDOHERMAPHRODITISM DUE TO 5α- REDUCTASE 2 DEFICIENCY Elaine Maria Frade Costa, Ivo Jorge Prado Arnhold, Marlene Inacio and Berenice Bilharinho Mendonca RHCFAP/3050 COSTA EMF et al. - Normal bone density in male pseudohermaphroditism due to 5α-reductase 2 deficiency. Rev. Hosp. Clín. Fac. Med. S. Paulo 56(5):139-142, 2001. Bone is an androgen-dependent tissue, but it is not clear whether the androgen action in bone depends on testosterone or on dihydrotestosterone. Patients with 5α-reductase 2 deficiency present normal levels of testosterone and low levels of dihydrotestosterone, providing an in vivo human model for the analysis of the effect of testosterone on bone. Objective: To analyze bone mineral density in 4 adult patients with male pseudohermaphroditism due to 5α-reductase 2 deficiency. Results: Three patients presented normal bone mineral density of the lumbar column (L1-L4) and femur neck, and the other patient presented a slight osteopenia in the lumbar column. Conclusion: Patients with dihydrotestosterone deficiency present normal bone mineral density, suggesting that dihydrotestosterone is not the main androgen acting in bone. DESCRIPTOR: Bone mineral density. Male pseudohermaphroditism. 5α-reductase type 2 deficiency. It has been well documented in the fied androgenic receptors in these cells, fects require aromatization into estro- literature that gonadal steroids regulate thus demonstrating that both androgens gens with subsequent activation of the normal bone metabolism and that in- and estrogens act by a direct mecha- estrogenic receptor. Although it has adequate estrogen concentrations in fe- nism through their respective receptors.