Photorefractive Keratectomy Used to Be the Procedure of Choice Simply Because It Was the Only Show in Town. But, More Than A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Qualified/Nonqualified Medical Expenses Under Health FSA/HRA Or HSA
Qualified/Nonqualified Medical Expenses under Health FSA/HRA or HSA Below is a partial list of medical expenses that may be reimbursed through your FSA/HRA or HSA, including services incurred by you or your eligible dependents for the diagnosis, treatment or prevention of disease, or for the amounts you pay for transportation to get medical care. In general, deductions allowed for medical expenses on your federal income tax, according to the Internal Revenue Code Section 213 (d), may be reimbursed through your FSA/HRA or HSA. Some items might not be reimbursable under your particular health FSA or HRA if the FSA or HRA contains exclusions, restrictions, or other limitation or requirements. Consult your summary plan description (SPD) of the health FSA or HRA for guidance. If you have an HSA, you are responsible for determining whether an expense qualifies for a tax‐free distribution. Qualified Expenses (partial list) Acupuncture Insulin Alcoholism treatment Lactation consultant Ambulance Laser eye surgery, Lasik Artificial limbs Occlusal guards to prevent teeth grinding Artificial teeth Optometrist Bandages, elastic or for injured skin Organ donors Blood pressure monitoring device Orthodontia Blood sugar test kits and test strips Osteopath fees Breast Pumps Oxygen Chiropractor Prosthesis Cholesterol test kits Reading Glasses Contact lenses Stop‐smoking aids Crutches Telephone equipment to assist persons with Dental Services and procedures hearing or speech disabilities Dentures Television equipment to assist persons with Diabetic supplies -
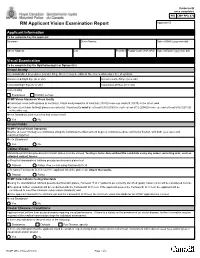
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -

(Usually Oxygen) Burn Reaction Adds Energy to Effect • Steel Typical
Reactive Fusion Cutting • When gas used reacts with gas (usually oxygen) burn reaction adds energy to effect • Steel typically 60% added energy • Titanium 90% added energy • However can reaction can chemically change the work face eg titanium gets brittle from oxygen • Cutting speed is increases with addition of oxygen Reactive Fusion Cutting Striations • Reactions create a burn front • Causes striations in material • Seen if the cut is slow Behavior of Materials for Laser Cutting • Generally break down by reflectivity and organic/inorganic Controlled Fracture and Scribing Controlled Fracture • Brittle materials vulnerable to thermal stress fracture • Heat volume: it expands, creates tensile stress • On cooling may crack • Crack continue in direction of hot spot • Mostly applies to insulators eg Sapphire, glass Scribing • Create a cut point in the material • Forms a local point for stress breakage • Use either a line of holes or grove Cold Cutting or Laser Dissociation • Uses Eximer (UV) lasers to cut without melting • UV photons 3.5 - 7.9 eV • Enough energy to break organic molecular bonds • eg C=H bond energy is 3.5 eV • Breaking the bonds causes the material to fall apart: disintigrates • Does not melt, chare or boil surface • eg ArF laser will create Ozone in air which shows the molecular effects Eximer Laser Dissociation • Done either with beam directly or by mask • Short Laser pulse absorbed in 10 micron depth • Breaks polymer bonds • Rapid rise in local pressure as dissociation • Mini explosions eject material Eximer Micromachining -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Richard C. Troutman, MD: a Pioneer
OBITUARY Richard C. Troutman, MD: A Pioneer Douglas Lazzaro, MD Dr Richard C. Troutman. ichard C. Troutman, MD, passed away on April 5, 2017, in Bal Harbour, Florida. Dr R Troutman was recognized as a gifted surgeon, an exceptional teacher, a beloved ophthalmologist, and the devoted husband of Suzanne Véronneau, MD. Dr Troutman remained active in the field into his early 90s and was still current in his knowledge of contemporary corneal transplantation and refractive surgery techniques. Dr Troutman was born in Ohio on May 16, 1922. His father, an EENT specialist, was his inspiration for pursuing a career in medicine. He enlisted in the navy as World War 2 started and went back to Ohio State University to finish medical school, where he graduated in 1945. A chance meeting with a graduate of Ohio State University in NYC led to a brief meeting with John McLean, recent Chairman at Cornell, and a week later, he was accepted into the residency program. His residency was interrupted to complete his military service. Residency was completed in 1949. He was accepted into a Fulbright Fellowship in France, but that was interrupted by a positive x-ray for tuberculosis, necessitating a year of treatment at the Trudeau Sanatorium in upstate New York. Dr Troutman’s early foray into clinical research began with work on orbital implants while still a senior resident and work was presented on this topic at the American Academy of Ophthalmology in 1951. He was asked to chair 3 major committees by the Academy during his career. R. Townley Paton gave him his first academic job as resident instructor at the Manhattan Eye, Ear and Throat Hospital after his training, where he was responsible for coordinating the training of 12 residents. -

Medical Treatment of Operative Corneal Perforation Caused By
CASE REPORTS AND SMALL CASE SERIES and clinical course of a patient with the stromal bed was thin; in the left Medical Treatment a LASIK-induced corneal perfora- eye, the corneal flap was very edema- of Operative Corneal tion that affected the final visual acu- tous and a space was visible between Perforation Caused ity. We believe that this report on the the corneal flap and the stromal bed treatment and recovery of the cor- (Figure 1, left). The anterior cham- by Laser In Situ neal perforation will be valuable in- ber was very shallow, and aqueous Keratomileusis formation for refractive surgeons. humor was observed to leak onto the ocular surface with blinking (Figure Laser in situ keratomileusis (LASIK) Report of a Case. A 33-year-old man 1, right). A round, 0.25-mm diam- is an effective procedure to treat a was referred to us with a complaint eter perforation site was observed in wide range of myopia.1 The advan- of decreased visual acuity in the left the center of the stromal bed by slit- tages of LASIK over photorefrac- eye after bilateral simultaneous lamp examination. tive keratectomy (PRK) are rapid vi- LASIK performed 3 days previ- We treated the corneal perfo- sual recovery, lower risk of corneal ously at a different facility. A cor- ration by applying a therapeutic soft haze, greater regression of myopia, neal perforation was noticed in the contact lens with topical antibiot- and less postoperative pain.1-3 How- left eye during LASIK laser abla- ics, oral carbonic anhydrase inhibi- ever, LASIK requires more skillful tion in this eye. -

Binder Innovations and New Techniques of Surgical
Susanne Binder, Univ. Prof., Dr. med., Wien, Austria Innovations and New Techniques of Surgical Ophthalmology Since the introduction of microsurgery in the field of ophthalmology with the routine use of surgical microscopes, precision and security have been tremendously improved. Numerous new instruments have been invented to do justice to the small size and the optical function of the organ and surgical sutures which are not visible to the naked eye have been developed (Barraquer, Ignacio; Joaquin, Jose 1952-77). During a cataract surgery, the intervention carried out most frequently, the clouded lens used to be excised completely in earlier times and the patient had to wear thick cataract glasses as a compensation for the missing dioptres. Cataract Surgery In the past 30 years cataract surgery was dominated by lens implantation surgery (Binghorst, Worst, 1960-70). The method of intracapsular cataract extraction was crowned by little success in the 1950ies as a result of material problems. Thus a shift in surgical technology took place in the 1960ies towards extracapsular lens extraction and implantation of an artificial lens. In industrial countries the cataract glasses were quickly replaced by implants and the employment of increasingly precise technologies for lens extraction. The state-of-the-art method of cataract surgery is phacoemulsification of the lens with a 1.2mm thick instrument and a foldable lens insertion through a tiny 3mm cornea incision. Also infants of 2 years of age and older can be implanted an artificial lens after the lens extraction in order to prevent weak-sightedness. In developing countries cataract, as a consequence of vitamin A deficiencies and the resulting drying of the cornea surface, and trachoma, caused by a bacterial infection transmitted by flies, are the most frequent causes for blindness. -

Fluency of Laser and Surgical Downtime, Loss of Fixation, As Factors Related to the Precision Refractive
112ARTIGO ORIGINAL Fluência do laser e tempo de parada cirúrgica, por perda de fixação, como fatores relacionados à precisão refracional Fluency of laser and surgical downtime, loss of fixation, as factors related to the precision refractive Abrahão da Rocha Lucena1, Newton Leitão de Andrade2, Descartes Rolim de Lucena3, Isabela Rocha Lucena4, Daniela Tavares Lucena5 RESUMO Objetivo: Avaliar a correlação da fluência e o tempo de parada transoperatória por perda de fixação, como fatores de hiper ou hipocorreções das ametropias pós-Lasik. Métodos: A idade variou entre 19 e 61 anos com média de 31,27 ± 9,99. O tempo mínimo de acompanhamento pós-operatório foi de 90 dias. Foram excluídos indivíduos com topografia corneana pré-operatória com ceratometria máxima maior que 46,5D ou presença de irregularidades; ceratometria média pós-operatória simulada menor que 36,0D; pupilas maiores que 6mm; paquimetria menor que 500 µm; miopia maior que -8,0DE, hipermetropia maior que +5,0DE e astigmatismo maior que -4,0DC. O laser utilizado foi o Esiris Schwind com Eye-Tracking de 350Hz e scanning spot de 0,8 mm. O microcerátomo utilizado foi o M2 da Moria com programação de 130µm de espessura. Resultados: A acuidade visual logMAR pré-operatória com correção variou de 0,40 a 0 com média de 0,23 ± 0,69; a pós-operatória sem correção foi de 0,40 a 0 com média de 0,30 ± 0,68. A mediana foi de 0 logMAR para os dois momentos (p=0,424). No equivalente esférico pré e pós-operatório, notou-se uma óbvia diferença (p< 0,0001), no pré-operatório com média de -4,09 ± 2,83 e o pós com média de -0,04 ± 0,38. -

LASIK: Why Doing Better Is Important
mivision • ISSUE 116 • SEP 16 miophthalmology 33 CreatingCreating vision LASIK: Why Doing Better withwith aa SMILE.SMILE. is Important ZEISSZEISS ReLExReLEx SMILESMILE Dr. DevinderRick Wolfe Chauhan LASIK has arguably become the safest It became evident that many LASIK and and most effective surgery of all time, but PRK patients, even those who had low it wasn’t always that way. It came about myopic ablations, had significantly reduced because of a confluence of technologies and night vision with halos. In Germany, where needs. José Barraquer developed the lamellar a night vision simulation is used in drivers’ refractive surgery in the 60s in Columbia. licence testing, some who had had PRK His procedure – myopic keratomileusis were denied the right to drive at night. (MKM) – involved the freezing, lathing and Quality of vision, particularly night vision, replacement of a corneal cap, which was is critical in military environments. Capt. much like the flap in modern LASIK, except (retired) Steven Schallhorn developed there was no hinge. It was not so long ago the United States Navy (USN) refractive In 1983, Dr. Trokel showed the excimer surgery program. I had the privilege of that we performed laser could be used to reshape the cornea. working with him at USN Medical Center PRK worked well, but slow recovery and San Diego as part of a RAN Reserve conventional laser postoperative pain were serious problems. exchange some years ago. Professor Ioannis Pallikaris first performed Other forces followed the USN lead in treatments that sadly excimer laser under a corneal flap in 1991 developing their own programs because at Crete University. -

Evaluating the Relation of Refractive Surgery and Glaucoma
Editorial Remedy Open Access Published: 25 Jul, 2017 Evaluating the Relation of Refractive Surgery and Glaucoma Kozobolis V*, Kostantinidis A and Labiris G Department of Ophthalmology, University of Thrace, Greece Editorial Laser-assisted refractive corrections constitute a large part of the ophthalmic surgeries that take place every year. It is estimated that about 4 million refractive procedures were performed in 2014 throughout the world. On the other hand, glaucoma is an optic neuropathy, the incidence of which is increasing steadily over time. Given the frequency of refractive surgeries and the incidence of glaucoma in the general population it becomes necessary for the ophthalmologist to assess the risks of a refractive surgery in a glaucoma patient or a patient at a risk of developing glaucoma in the future. The factors to take into consideration are: the family history of glaucoma, intraocular pressure (IOP), myopia, high vertical cup-to-disc ratio, central corneal thickness, and race, other ophthalmic diseases, hypermetropia, previous antiglaucoma procedure, visual fields and modern imaging modalities. The advantages of these modalities include objective and reproducible measurements that can be compared with future measurements. The disadvantage is that their databases (although constantly enriched) include limited number of people, while "unusual" discs (tilted, high ametropias) are excluded from the databases. Unfortunately many candidates for refractive surgery have optic discs with “unusual” appearance that cannot be meaningfully compared with the “normal” optic discs of the databases. In these cases the digital photographing of the optic disc and the comparison with future photos will give valuable information about the changes of both the optic nerve and retinal nerve fibers.