The Fracturing of Authoritative 11Bbi Knowledge in Twentieth-Century India'
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
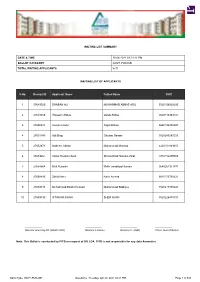
GOVT-PUNJAB Waitinglist Nphs.Pdf
WAITING LIST SUMMARY DATE & TIME 20-04-2021 02:21:11 PM BALLOT CATEGORY GOVT-PUNJAB TOTAL WAITING APPLICANTS 8711 WAITING LIST OF APPLICANTS S No. Receipt ID Applicant Name Father Name CNIC 1 27649520 SHABAN ALI MUHAMMAD ABBAS ADIL 3520106922295 2 27649658 Waseem Abbas Qalab Abbas 3520113383737 3 27650644 Usman Hiader Sajid Abbasi 3650156358657 4 27651140 Adil Baig Ghulam Sarwar 3520240247205 5 27652673 Nadeem Akhtar Muhammad Mumtaz 4220101849351 6 27653461 Imtiaz Hussain Zaidi Shasmshad Hussain Zaidi 3110116479593 7 27654564 Bilal Hussain Malik tasadduq Hussain 3640261377911 8 27658485 Zahid Nazir Nazir Ahmed 3540173750321 9 27659188 Muhammad Bashir Hussain Muhammad Siddique 3520219305241 10 27659190 IFTIKHAR KHAN SHER KHAN 3520226475101 ------------------- ------------------- ------------------- ------------------- Director Housing-XII (LDAC NPA) Director Finance Director IT (I&O) Chief Town Planner Note: This Ballot is conducted by PITB on request of DG LDA. PITB is not responsible for any data Anomalies. Ballot Type: GOVT-PUNJAB Date&time : Tuesday, Apr 20, 2021 02:21 PM Page 1 of 545 WAITING LIST OF APPLICANTS S No. Receipt ID Applicant Name Father Name CNIC 11 27659898 Maqbool Ahmad Muhammad Anar Khan 3440105267405 12 27660478 Imran Yasin Muhammad Yasin 3540219620181 13 27661528 MIAN AZIZ UR REHMAN MUHAMMAD ANWAR 3520225181377 14 27664375 HINA SHAHZAD MUHAMMAD SHAHZAD ARIF 3520240001944 15 27664446 SAIRA JABEEN RAZA ALI 3110205697908 16 27664597 Maded Ali Muhammad Boota 3530223352053 17 27664664 Muhammad Imran MUHAMMAD ANWAR 3520223937489 -

Ayurvedic Doctor V1.1
Ayurvedic Doctor v1.1 2019-2022 Program August 24, 2019 – March 6, 2022 CATALOG REGISTERED OFFICES: State of CA Kerala Ayurveda Academy 691 S. Milpitas Blvd Suite 206 Milpitas, CA 95035 Toll Free: +1 (888) 275-9103 Fax: +1 (510) 257-4378 State of WA 3876 Bridge Way N, #300, Seattle, WA 98103 Toll Free: +1 (888) 275-9103 Registration: [email protected] All Other Course Support: [email protected] Website: www.keralaayurveda.us Date of Publication 2/1/19 Kerala Ayurveda Academy, in the State of California, is a privately-owned institution that is approved to operate by the Bureau for Private Postsecondary Education under School Code# 72482254. BPPE address: 2535 Capital Oaks Drive, Suite 400, Sacramento, CA 95833, Phone: +1 (888) 370-7589. Kerala Ayurveda Academy, in the State of Washington, is licensed under Chapter 28C.10 RCW. Inquiries or complaints regarding this private vocational school may be made to the: Workforce Board, 128 10th Ave. SW, Box 43105, Olympia, Washington 98504. Web: wtb.wa.gov, phone: +1 (360) 709-4600, e-mail address: [email protected]. 2 Page © 2019 Kerala Ayurveda Academy Ayurveda Kerala 2019 © Table of Contents TABLE OF CONTENTS 3 WELCOME TO KERALA AYURVEDA ACADEMY 5 Our Mission and Heritage 5 Why Choose Kerala Ayurveda Academy? 6 Take Pride in Knowing… 6 PROGRAM OVERVIEW 7 General Format 7 Prerequisites 7 Scope of Practice 8 Course Description & Objectives 8 Curriculum 8 Learning Materials & Resources 16 Program Format & Hours 17 Student Orientation - 3 hours 17 Master Track – 436 hours 17 Allied Programs – 601 hours 18 Program Hour Breakdowns 23 Academic Advisor 25 Tests & Grading 25 Graduation Requirements 25 FACULTY 26 Senior Faculty 26 Dr. -

INDIAN NATIONAL CONGRESS 1885-1947 Year Place President
INDIAN NATIONAL CONGRESS 1885-1947 Year Place President 1885 Bombay W.C. Bannerji 1886 Calcutta Dadabhai Naoroji 1887 Madras Syed Badruddin Tyabji 1888 Allahabad George Yule First English president 1889 Bombay Sir William 1890 Calcutta Sir Pherozeshah Mehta 1891 Nagupur P. Anandacharlu 1892 Allahabad W C Bannerji 1893 Lahore Dadabhai Naoroji 1894 Madras Alfred Webb 1895 Poona Surendranath Banerji 1896 Calcutta M Rahimtullah Sayani 1897 Amraoti C Sankaran Nair 1898 Madras Anandamohan Bose 1899 Lucknow Romesh Chandra Dutt 1900 Lahore N G Chandravarkar 1901 Calcutta E Dinsha Wacha 1902 Ahmedabad Surendranath Banerji 1903 Madras Lalmohan Ghosh 1904 Bombay Sir Henry Cotton 1905 Banaras G K Gokhale 1906 Calcutta Dadabhai Naoroji 1907 Surat Rashbehari Ghosh 1908 Madras Rashbehari Ghosh 1909 Lahore Madanmohan Malaviya 1910 Allahabad Sir William Wedderburn 1911 Calcutta Bishan Narayan Dhar 1912 Patna R N Mudhalkar 1913 Karachi Syed Mahomed Bahadur 1914 Madras Bhupendranath Bose 1915 Bombay Sir S P Sinha 1916 Lucknow A C Majumdar 1917 Calcutta Mrs. Annie Besant 1918 Bombay Syed Hassan Imam 1918 Delhi Madanmohan Malaviya 1919 Amritsar Motilal Nehru www.bankersadda.com | www.sscadda.com| www.careerpower.in | www.careeradda.co.inPage 1 1920 Calcutta Lala Lajpat Rai 1920 Nagpur C Vijaya Raghavachariyar 1921 Ahmedabad Hakim Ajmal Khan 1922 Gaya C R Das 1923 Delhi Abul Kalam Azad 1923 Coconada Maulana Muhammad Ali 1924 Belgaon Mahatma Gandhi 1925 Cawnpore Mrs.Sarojini Naidu 1926 Guwahati Srinivas Ayanagar 1927 Madras M A Ansari 1928 Calcutta Motilal Nehru 1929 Lahore Jawaharlal Nehru 1930 No session J L Nehru continued 1931 Karachi Vallabhbhai Patel 1932 Delhi R D Amritlal 1933 Calcutta Mrs. -

Remembering Partition: Violence, Nationalism and History in India
Remembering Partition: Violence, Nationalism and History in India Gyanendra Pandey CAMBRIDGE UNIVERSITY PRESS Remembering Partition Violence, Nationalism and History in India Through an investigation of the violence that marked the partition of British India in 1947, this book analyses questions of history and mem- ory, the nationalisation of populations and their pasts, and the ways in which violent events are remembered (or forgotten) in order to en- sure the unity of the collective subject – community or nation. Stressing the continuous entanglement of ‘event’ and ‘interpretation’, the author emphasises both the enormity of the violence of 1947 and its shifting meanings and contours. The book provides a sustained critique of the procedures of history-writing and nationalist myth-making on the ques- tion of violence, and examines how local forms of sociality are consti- tuted and reconstituted by the experience and representation of violent events. It concludes with a comment on the different kinds of political community that may still be imagined even in the wake of Partition and events like it. GYANENDRA PANDEY is Professor of Anthropology and History at Johns Hopkins University. He was a founder member of the Subaltern Studies group and is the author of many publications including The Con- struction of Communalism in Colonial North India (1990) and, as editor, Hindus and Others: the Question of Identity in India Today (1993). This page intentionally left blank Contemporary South Asia 7 Editorial board Jan Breman, G.P. Hawthorn, Ayesha Jalal, Patricia Jeffery, Atul Kohli Contemporary South Asia has been established to publish books on the politics, society and culture of South Asia since 1947. -
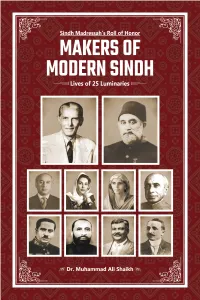
Makers-Of-Modern-Sindh-Feb-2020
Sindh Madressah’s Roll of Honor MAKERS OF MODERN SINDH Lives of 25 Luminaries Sindh Madressah’s Roll of Honor MAKERS OF MODERN SINDH Lives of 25 Luminaries Dr. Muhammad Ali Shaikh SMIU Press Karachi Alma-Mater of Quaid-e-Azam Mohammad Ali Jinnah Sindh Madressatul Islam University, Karachi Aiwan-e-Tijarat Road, Karachi-74000 Pakistan. This book under title Sindh Madressah’s Roll of Honour MAKERS OF MODERN SINDH Lives of 25 Luminaries Written by Professor Dr. Muhammad Ali Shaikh 1st Edition, Published under title Luminaries of the Land in November 1999 Present expanded edition, Published in March 2020 By Sindh Madressatul Islam University Price Rs. 1000/- SMIU Press Karachi Copyright with the author Published by SMIU Press, Karachi Aiwan-e-Tijarat Road, Karachi-74000, Pakistan All rights reserved. No part of this book may be reproduced in any from or by any electronic or mechanical means, including information storage and retrieval system, without written permission from the publisher, except by a reviewer, who may quote brief passage in a review Dedicated to loving memory of my parents Preface ‘It is said that Sindh produces two things – men and sands – great men and sandy deserts.’ These words were voiced at the floor of the Bombay’s Legislative Council in March 1936 by Sir Rafiuddin Ahmed, while bidding farewell to his colleagues from Sindh, who had won autonomy for their province and were to go back there. The four names of great men from Sindh that he gave, included three former students of Sindh Madressah. Today, in 21st century, it gives pleasure that Sindh Madressah has kept alive that tradition of producing great men to serve the humanity. -

HIGH COURT of SINDH, KARACHI (Recruitment Test) ADDITIONAL
HIGH COURT OF SINDH, KARACHI (Recruitment Test) Test held on 29 March 2015 ADDITIONAL DISTRICT & SESSIONS JUDGE Sr # Roll No Comp. Code Name Father Name CNIC NTS Marks 1 216 2014900 ATIF UDDIN ASIF UDDIN SIDDIQUI 42201-0790319-5 77 2 381 201369 HAFIZ MISBAHUDDIN NAIMATULLAH PHULPOTO 45504-1133788-1 77 3 64 2013850 ABDUL SHAKOOR KALHORO MUHAMMAD MOOSA KALHORO 45501-1880925-1 75 4 719 201327 MUHAMMAD NAEEM ALLAH WARAYO MEMON 45203-3047320-5 74 5 396 2013467 HATIM AZIZ SOLANGI AZIZ UL HAQ SOLANGI 43203-8847475-5 73 6 390 201371 HALEEM AHMED IMDAD ALI 42301-8902207-5 73 7 74 2013472 ABDULLAH ABDUL WAHAB 42301-0982702-9 72 8 1191 2013494 SYED SAJJAD HUSSAIN SHAH SYED ZAMAN SHAH 45304-1496948-5 72 9 664 2013110 MUHAMMAD ARIF RAJPUT MUHAMMAD RIAZ RAJPUT 44103-1263527-1 72 10 845 20131 NAVEED AHMED SOOMRO AFTAB AHMED SOOMRO 45504-6572854-5 71 11 298 201374 FATIMA JAMEELA JATOI GHULAM QADIR JATOI 45504-1092609-8 71 12 602 2013331 MIAN TAJ MOHAMMAD KEERIO MIAN PEER MOHAMMAD KEERIO 44203-1757881-5 70 13 357 2014929 GHULAM RAZA KHAN MUHAMMAD 42000-4391368-7 70 14 266 2013102 FAHMIDA SAHOOWAL MUHAMMAD HUSSAIN SAHOOWAL 42201-7282118-4 69 15 1214 20141052 TAHIR REHMAN PARVEZ KHAN 42301-7779048-3 69 16 625 2014997 MOHAMMAD NOONARI KALOO NOONARI 41205-0394532-5 69 17 1130 201364 SHYAM LAL ARJAN DAS 45501-1200056-3 69 18 699 2013438 MUHAMMAD ISHAQ KHAN GUL ZAMAN KHAN 42201-6080988-5 69 19 669 20141407 MUHAMMAD ASIF ARAIN MUHAMMAD SHAFI ARAIN 41306-1712567-9 69 20 1243 2013116 UZMA KHAN MUHAMMAD ISHAQ KHAN 42000-8626931-8 69 21 1044 20141194 SEREENA SAEED -

A Comparative Analysis of the Concepts of Holy War and the Idealized Topos of Holy Warrior in Medieval Anatolian and European Sources
T.C. BAHÇEŞEHİR ÜNİVERSİTESİ A COMPARATIVE ANALYSIS OF THE CONCEPTS OF HOLY WAR AND THE IDEALIZED TOPOS OF HOLY WARRIOR IN MEDIEVAL ANATOLIAN AND EUROPEAN SOURCES Master’s Thesis CEREN ÇIKIN SUNGUR İSTANBUL, 2014 T.C. BAHÇEŞEHİR UNIVERSITY GRADUATE SCHOOL OF SOCIAL SCIENCES DEPARTMENT OF HISTORY Supervisors: Prof. Dr. Heath W. LOWRY & Ass. Prof. Dr. Derya GÜRSES TARBUCK To my beloved Can, for all his kindness and support… ACKNOWLEDGEMENTS First and foremost, I must thank my research supervisors, Professor Heath W. Lowry and Assistant Professor Derya Gürses Tarbuck for giving me the chance to work together and the opportunity to study at Bahçeşehir University. Without their support and assistance this thesis could not even exist as an idea. I would also like to thank Associate Professor Dr. Fikret Yılmaz for making me question certain matters on the military warfare of the early Ottomans I had not noticed before. I also have to thank Professor Paul Latimer from Bilkent University for his assistance and for lighting my path to an understanding of European history with his advice. ABSTRACT A COMPARATIVE ANALYSIS OF THE CONCEPTS OF HOLY WAR AND THE IDEALIZED TOPOS OF THE HOLY WARRIOR IN MEDIEVAL ANATOLIAN AND EUROPEAN SOURCES Ceren Çıkın Sungur History Supervisors: Prof. Dr. Heath W. Lowry & Ass. Prof. Derya Gürses Tarbuck June, 2014, 199 pages Claims of holy war characterized the Middle Ages in both Muslim Anatolia and Christian Europe, where soldiers on both sides were portrayed as holy warriors. Named gazis, akıncıs, alps, chevaliers and knights, they came from the elite military classes. Literary depictions of these men as holy warriors were fundamentally idealized topoi created by writers who were patronized by or were close to those in power. -

TCM Diagnostics Applied to Parasite-Related Disease
TCM Diagnostics Applied to Parasite-Related Disease by Laraine Crampton, M.A.T.C.M., L. Ac. Capstone Advisor: Lawrence J. Ryan, Ph.D. Presented in partial fulfillment of the requirements for the degree Doctor of Acupuncture and Oriental Medicine Yo San University of Traditional Chinese Medicine Los Angeles, California April 2014 TCM and Parasites/Crampton 2 Approval Signatures Page This Capstone Project has been reviewed and approved by: April 30th, 2014 ____________________________________________________________________________ Lawrence J. Ryan, Ph. D. Capstone Project Advisor Date April 30th, 2014 ________________________________________________________________________ Don Lee, L. Ac. Specialty Chair Date April 30th, 2014 ________________________________________________________________________ Andrea Murchison, D.A.O.M., L.Ac. Program Director Date TCM and Parasites/Crampton 3 Abstract Complex, chronic disease affects millions in the United States, imposing a significant cost to the affected individuals and the productivity and economic realities those individuals and their families, workplaces and communities face. There is increasing evidence leading towards the probability that overlooked and undiagnosed parasitic disease is a causal, contributing, or co- existent factor for many of those afflicted by chronic disease. Yet, frustratingly, inadequate diagnostic methods and clever adaptive mechanisms in parasitic organisms mean that even when physicians are looking for parasites, they may not find what is there to be found. Examining the practice of medicine in the United States just over a century ago reveals that fully a third of diagnostic and treatment concerns for leading doctors of the time revolved around parasitic organisms and related disease, and that the population they served was largely located in rural areas. By the year 2000, more than four-fifths of the population had migrated to cities, enjoying the benefits of municipal services, water treatment systems, grocery stores and restaurants. -

THE REIGN of AL-IHAKIM Bl AMR ALLAH ‘(386/996 - 41\ / \ Q 2 \ % "A POLITICAL STUDY"
THE REIGN OF AL-IHAKIM Bl AMR ALLAH ‘(386/996 - 41\ / \ Q 2 \ % "A POLITICAL STUDY" by SADEK ISMAIL ASSAAD Thesis submitted for the Degree of Doctor of Philosophy in the University of London May 1971 ProQuest Number: 10672922 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 10672922 Published by ProQuest LLC(2017). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 ABSTRACT The present thesis is a political study of the reign of al-Hakim Bi Amr Allah the sixth Fatimid Imam-Caliph who ruled between 386-411/ 996-1021. It consists of a note on the sources and seven chapters. The first chapter is a biographical review of al-Hakim's person. It introduces a history of his birth, childhood, succession to the Caliphate, his education and private life and it examines the contradiction in the sources concerning his character. Chapter II discusses the problems which al-Hakim inherited from the previous rule and examines their impact on the political life of his State. Chapter III introduces the administration of the internal affairs of the State. -

District Handbook Murshidabad
CENSUS 1951 W.EST BENGAL DISTRICT HANDBOOKS MURSHIDABAD A. MITRA of the Indian Civil Service, Superintendent ot Census OPerations and Joint Development Commissioner, West Bengal ~ted by S. N. Guha Ray, at Sree Saraswaty Press Ltd., 32, Upper Circular Road, Calcutta-9 1953 Price-Indian, Rs. 30; English, £2 6s. 6<1. THE CENSUS PUBLICATIONS The Census Publications for West Bengal, Sikkim and tribes by Sudhansu Kumar Ray, an article by and Chandernagore will consist of the following Professor Kshitishprasad Chattopadhyay, an article volumes. All volumes will be of uniform size, demy on Dbarmapuja by Sri Asutosh Bhattacharyya. quarto 8i" x II!,' :- Appendices of Selections from old authorities like Sherring, Dalton,' Risley, Gait and O'Malley. An Part lA-General Report by A. Mitra, containing the Introduction. 410 pages and eighteen plates. first five chapters of the Report in addition to a Preface, an Introduction, and a bibliography. An Account of Land Management in West Bengal, 609 pages. 1872-1952, by A. Mitra, contajning extracts, ac counts and statistics over the SO-year period and Part IB-Vital Statistics, West Bengal, 1941-50 by agricultural statistics compiled at the Census of A. Mitra and P. G. Choudhury, containing a Pre 1951, with an Introduction. About 250 pages. face, 60 tables, and several appendices. 75 pages. Fairs and Festivals in West Bengal by A. Mitra, con Part IC-Gener.al Report by A. Mitra, containing the taining an account of fairs and festivals classified SubSidiary tables of 1951 and the sixth chapter of by villages, unions, thanas and districts. With a the Report and a note on a Fertility Inquiry con foreword and extracts from the laws on the regula ducted in 1950. -

Defining Shariʿa the Politics of Islamic Judicial Review by Shoaib
Defining Shariʿa The Politics of Islamic Judicial Review By Shoaib A. Ghias A dissertation submitted in partial satisfaction of the Requirements for the degree of Doctor of Philosophy in Jurisprudence and Social Policy in the Graduate Division of the University of California, Berkeley Committee in Charge: Professor Malcolm M. Feeley, Chair Professor Martin M. Shapiro Professor Asad Q. Ahmed Summer 2015 Defining Shariʿa The Politics of Islamic Judicial Review © 2015 By Shoaib A. Ghias Abstract Defining Shariʿa: The Politics of Islamic Judicial Review by Shoaib A. Ghias Doctor of Philosophy in Jurisprudence and Social Policy University of California, Berkeley Professor Malcolm M. Feeley, Chair Since the Islamic resurgence of the 1970s, many Muslim postcolonial countries have established and empowered constitutional courts to declare laws conflicting with shariʿa as unconstitutional. The central question explored in this dissertation is whether and to what extent constitutional doctrine developed in shariʿa review is contingent on the ruling regime or represents lasting trends in interpretations of shariʿa. Using the case of Pakistan, this dissertation contends that the long-term discursive trends in shariʿa are determined in the religio-political space and only reflected in state law through the interaction of shariʿa politics, regime politics, and judicial politics. The research is based on materials gathered during fieldwork in Pakistan and datasets of Federal Shariat Court and Supreme Court cases and judges. In particular, the dissertation offers a political-institutional framework to study shariʿa review in a British postcolonial court system through exploring the role of professional and scholar judges, the discretion of the chief justice, the system of judicial appointments and tenure, and the political structure of appeal that combine to make courts agents of the political regime. -

Halal Development: Trends, Opportunities and Challenges
HALAL DEVELOPMENT: TRENDS, OPPORTUNITIES AND CHALLENGES PROCEEDINGS OF THE 1ST INTERNATIONALCONFERENCE ON HALAL DEVELOPMENT (ICHAD 2020), MALANG, INDONESIA, 8 OCTOBER 2020 Halal Development: Trends, Opportunities and Challenges Edited by Heri Pratikto & Ahmad Taufiq Universitas Negeri Malang, Indonesia Adam Voak Deakin University, Australia Nurdeng Deuraseh Universitas Islam Sultan Sharif Ali, Brunei Darussalam Hadi Nur Universiti Teknologi Malaysia, Indonesia Winai Dahlan The Halal Science Center Chulalongkorn University, Bangkok, Thailand Idris & Agus Purnomo Universitas Negeri Malang, Indonesia CRC Press/Balkema is an imprint of the Taylor & Francis Group, an informa business © 2021 The Author(s) Typeset by MPS Limited, Chennai, India The right of the first International Conference on Halal Development (ICHaD2020) to be identified as author[/s] of this work has been asserted by him/her/them in accordance with sections 77 and 78 of the Copyright, Designs and Patents Act 1988. The Open Access version of this book, available at www.taylorfrancis.com, has been made available under a Creative Commons Attribution-Non Commercial-No Derivatives 4.0 license. The Open Access version of this book will be available six months after its first day of publication. Although all care is taken to ensure integrity and the quality of this publication and the information herein, no responsibility is assumed by the publishers nor the author for any damage to the property or persons as a result of operation or use of this publication and/or the information