Lead Levels in Teeth As a Measure of Life-Time Lead Exposure in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Was the Tooth Fairy Breast Fed? the Politics of Infant Tooth Decay
Was the Tooth Fairy Breast Fed? The Politics of Infant Tooth Decay Yvonne Luxford Thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy at the University of New South Wales ORIGINALITY STATEMENT ‘I hereby declare that this submission is my own work and to the best of my knowledge it contains no materials previously published or written by another person, or substantial proportions of material which have been accepted for the award of any other degree or diploma at UNSW or any other educational institution, except where due acknowledgement is made in the thesis. Any contribution made to the research by others, with whom I have worked at UNSW or elsewhere, is explicitly acknowledged in the thesis. I also declare that the intellectual content of this thesis is the product of my own work, except to the extent that assistance from others in the project's design and conception or in style, presentation and linguistic expression is acknowledged.’ Signed ……………………………………………........................... i COPYRIGHT STATEMENT ‘I hereby grant the University of New South Wales or its agents the right to archive and to make available my thesis or dissertation in whole or part in the University libraries in all forms of media, now or here after known, subject to the provisions of the Copyright Act 1968. I retain all proprietary rights, such as patent rights. I also retain the right to use in future works (such as articles or books) all or part of this thesis or dissertation. I also authorise University Microfilms to use the 350 word abstract of my thesis in Dissertation Abstract International. -
Visitor Guide 2010
VisitorVisitor GuideGuide 2010 Free to you • FREE PULL OUT WALKING GUIDE INSIDE • • WHAT TO DO • WHERE TO GO • KIDS PAGE • WILDLIFE • EVENTS • www.northumberlandnationalpark.org.uk Welcome Vision for the future in Free to you! Northumberland National Park National Parks are ‘Britain's Breathing Spaces’ and Northumberland National Park with its distinctive open and tranquil landscapes and unique heritage will provide you with wonderful memories to savour. Stretching from Hadrian's Wall in the south, through the rolling valleys of the Tyne and Rede to the impressive hills of the Cheviots on the Scottish Border, the National Park has some of the most unspoilt landscapes in the country. Hadrian’s Wall page 6, page 11 Its’ wealth of history and culture has been shaped by a past that was Tony Gates, National Park Officer Chief Executive NNPA not always peaceful.The landscape of the National Park as it is today has been formed over centuries - from Iron Age hillforts to the legacy Northumberland National Park is a of the Romans, through the Middle Ages to the Victorian industrial age - special place and we have a vision for the 405 scenic square miles and the evidence is everywhere. (1049km2) of this protected landscape that we share with the many people In this Visitor Guide you will see how the National Park Authority, who helped us to develop our latest landowners, farmers, businesses and other organisations are all working Management Plan. to ensure that Northumberland National Park remains one of Britain's Our vision is that Northumberland most beautiful breathing spaces for everyone to enjoy. -

Please Note Venue Scrutiny Co-Ordinating Committee Agenda
PLEASE NOTE VENUE SCRUTINY CO-ORDINATING COMMITTEE AGENDA Friday 4 January 2008 at 2.00 p.m. at Owton Manor Community Centre, Wynyard Road, Hartlepool MEMBERS: SCRUTINY CO-ORDINATING COMMITTEE: Councillors Akers-Belcher, Brash, R W Cook, S Cook, Fleet, Flintoff, James, Laffey, A E Lilley, G Lilley, A Marshall, Plant, Preece, Shaw, Simmons and Wright. Resident Representatives: Jean Kennedy, Iris Ryder and Linda Shields 1. APOLOGIES FOR ABSENCE 2. TO RECEIVE ANY DECLARATIONS OF INTEREST BY MEMBERS 3. MINUTES 3.1 To confirm the minutes of the meetings held on 2nd, 9th and 21st November 2007 (attached) 4. RESPO NS ES FROM THE CO UNCIL, THE EX ECUT IV E OR COMMI TT EES OF THE COUNCIL TO REPORTS OF THE SCRUTINY COORDINATING COMMITTEE No Items 5. CONSIDERATION OF REQUES T FOR SCRUTINY REVIEWS FROM COUNCIL, EX ECUTIV E MEMBERS AND NON EX ECUTIV E MEM BERS No Items 08.01.04 - SCR UTCOORD AGENDA Hartlepool Bor ough Council 1 PLEASE NOTE VENUE 6. FORWARD PLAN 6.1 Forward Plan: January 2008 – March 2008 - Scrutiny Manager 7. CONSIDERATION OF PROGRESS REPORTS / BUDGET AND POLICY FRAM EWORK DOCUM ENTS 7.1 2008/09 Budget and Policy Framework Proposals – Scrutiny Manager 8. CONSIDERATION OF FINANCIAL MONITORING/CORPORATE REPORTS 8.1 Quarter 2 – Corporate Plan and Revenue Financial Management Report 2007/2008 – Chief Financial Officer 8.2 Quarter 2 – NRF, Capital and Accountable Body Programme Monitoring Report 2007/2008 – Chief Financial Officer 9. ITEMS FOR DISCUSSION 9.1 Adult and Community Services and Health Scrutiny Forum – Restructure Proposals – Chair of the Scrutiny Co-ordinating Committee 9.2 Funding of Contract Monitoring System – Explanation of the Adult and Public Health Portfolio Holder – Chair of the Adult and Community Services and Health Scrutiny Forum 9.3 Request for Items for Joint Cabinet / Scrutiny Event of 22 January 2008 – Scrutiny Manager 10. -

Arkan Sonney (Erkin Sonna)
.. Arkan Sonney (erkin sonna) Easter Fairy The Arkan Sonney or ‘Lucky Piggy’ Easter fairies gather in spring to is the name given to the Fairy Pig of harvest the eggs which the hares decorate The isle of Man. It is believed to at the time of the Spring Equinox bring luck and can alter it’s size to present as symbols of fertility to but not it’s shape. Oestre, the pagan goddess after which Easter is named. They can be easily caught Draig at this time of year as overeating Draig is very fond of treasure chocolate greatly reduces their agility! and maidens, especially princesses. He has fiery breath, a sting in his tail and can stay asleep for up to 25 years . Urban Fairy We cannot be sure how long your young Urban fairies congregate in vacant lots and Draig has been subways where they find many of the objects snoozing, so beware! carelessly discarded by people very useful for decorating their homes. Cluricaune Cluricaunes dwell in wine cellars and make themselves objectionable Australian Bunyip Babies by unnerving those who come for the As we have not yet seen one we have not been able to confirm the wine. Sometimes the owners have been appearance of these elusive characters, but our sources suggest that known to move away to escape these they may look a bit like this! troublesome sprites. This little chap was found in Bunyips inhabit inland waterways one such abandoned cellar. especially waterholes in dried up river beds in outback Australia. They are Will O’ the Wisp notoriously fond of Billabongs where, for countless generations they have Will O’ Wisp or lurked, frightening the native people Ignis Fatus (the foolish fire), as they come to fetch water. -

Archaeology in Northumberland Friends
100 95 75 Archaeology 25 5 in 0 Northumberland 100 95 75 25 5 0 Volume 20 Contents 100 100 Foreword............................................... 1 95 Breaking News.......................................... 1 95 Archaeology in Northumberland Friends . 2 75 What is a QR code?...................................... 2 75 Twizel Bridge: Flodden 1513.com............................ 3 The RAMP Project: Rock Art goes Mobile . 4 25 Heiferlaw, Alnwick: Zero Station............................. 6 25 Northumberland Coast AONB Lime Kiln Survey. 8 5 Ecology and the Heritage Asset: Bats in the Belfry . 11 5 0 Surveying Steel Rigg.....................................12 0 Marygate, Berwick-upon-Tweed: Kilns, Sewerage and Gardening . 14 Debdon, Rothbury: Cairnfield...............................16 Northumberland’s Drove Roads.............................17 Barmoor Castle .........................................18 Excavations at High Rochester: Bremenium Roman Fort . 20 1 Ford Parish: a New Saxon Cemetery ........................22 Duddo Stones ..........................................24 Flodden 1513: Excavations at Flodden Hill . 26 Berwick-upon-Tweed: New Homes for CAAG . 28 Remapping Hadrian’s Wall ................................29 What is an Ecomuseum?..................................30 Frankham Farm, Newbrough: building survey record . 32 Spittal Point: Berwick-upon-Tweed’s Military and Industrial Past . 34 Portable Antiquities in Northumberland 2010 . 36 Berwick-upon-Tweed: Year 1 Historic Area Improvement Scheme. 38 Dues Hill Farm: flint finds..................................39 -

November 2017
www.richlandareachamber.comw Presented by: Encourage Your Family & Friends to Re-Think Richland Karen Seman RCDG, Workforce Development Re-Think Richland is a new iniave meant to offer a fresh perspecve on life and work in the Richland County area. Life is great in a small pond - low cost of living, affordable child care, a wide array of professional opportunies, and growing communies! You will be seeing the below campaign across Richland County. Please help by spreading the word about this upcoming event, and be sure to like Re-Think Richland on Facebook! Chamber Staff RCDG Staff Contact us @ 419-522-3211 or e-mail us: Contact us @ 419-755-7234 or email us: [email protected] [email protected] Jodie A. Perry, IOM, CCEO-AP, President/CEO Roberta Perry, Community Development Suzy Beeson, Front Office Karen Seman, Workforce Development Lisa Duckworth, Program & Events Barre Thomas, Economic Development Stephany Elgin, Member Services Angie Fanello, Markeng & Communicaons Nikki Lewis, Foundaon Manager www.richlandareachamber.com S Carrousel Antiques 20th JJS Sports Academy Anniversary (Mansfield) (Mansfield/Ontario) Blue Barista Coffee Co. (Richland Mall) Aesthetic Lookz i-Browz (Richland Mall) Clothes Mentor (Ontario) Avita Health System groundbreaking (Bellville) The Hope Homes of Richland County (Mansfield) Contemporary Art Space (Richlandwww.richlandareachamber.com Mall) Little Buckeye Children’s Museum Grocery Store Exhibit (Mansfield) “Around here, however, we don’t look backwards for very long. We keep moving forward, opening up new doors and doing new things, because we’re curious…and curiosity keeps leading us down new paths.” ~Walter Elias Disney In keeping with the back-to-school season and doing new things, CareWorksComp has a few educaonal opportunies to share with you that we hope you will consider: a Risk Reducon Workshop, and Two Hour Group Safety Training classes. -
Waste Arisings and Waste Management Capacity Model
Addendum to 2012 study: Waste Arisings and Waste Management Capacity Model Durham County Council June 2018 Addendum to 2012 study: Waste Arisings and Waste Management Capacity Model Disclaimer Anthesis Consulting Group PLC has prepared this report for the sole use of Durham County Council and for the intended purposes as stated in the agreement between Anthesis and Durham County Council under which this report was completed. Anthesis has exercised due and customary care in preparing this report but has not, save as specifically stated, independently verified information provided by others. No other warranty, express or implied, is made in relation to the contents of this report. The use of this report, or reliance on its content, by unauthorised third parties without written permission from Anthesis shall be at their own risk, and Anthesis accepts no duty of care to such third parties. Any recommendations, opinions or findings stated in this report are based on facts and circumstances as they existed at the time the report was prepared. Any changes in such facts and circumstances may adversely affect the recommendations, opinions or findings contained in this report. Anthesis Consulting Group, 2018 1 Addendum to 2012 study: Waste Arisings and Waste Management Capacity Model Addendum to 2012 study: Waste Arisings and Waste Management Capacity Model Durham County Council Prepared for: Prepared by: Spatial Policy Team Anthesis Consulting Group Regeneration & Local Services Development The Future Centre, Durham County Council 9 Newtec Place, -

County Durham Plan (Adopted 2020)
County Durham Plan ADOPTED 2020 Contents Foreword 5 1 Introduction 7 Neighbourhood Plans 7 Assessing Impacts 8 Duty to Cooperate: Cross-Boundary Issues 9 County Durham Plan Key Diagram and Monitoring 10 2 What the County Durham Plan is Seeking to Achieve 11 3 Vision and Objectives 14 Delivering Sustainable Development 18 4 How Much Development and Where 20 Quantity of Development (How Much) 20 Spatial Distribution of Development (Where) 29 5 Core Principles 71 Building a Strong Competitive Economy 71 Ensuring the Vitality of Town Centres 78 Supporting a Prosperous Rural Economy 85 Delivering a Wide Choice of High Quality Homes 98 Protecting Green Belt Land 124 Sustainable Transport 127 Supporting High Quality Infrastructure 138 Requiring Good Design 150 Promoting Healthy Communities 158 Meeting the Challenge of Climate Change, Flooding and Coastal Change 167 Conserving and Enhancing the Natural and Historic Environment 185 Minerals and Waste 212 Appendices A Strategic Policies 259 B Table of Superseded Policies 261 C Coal Mining Risk Assessments, Minerals Assessments and Minerals and/or Waste 262 Infrastructure Assessment D Safeguarding Mineral Resources and Safeguarded Minerals and Waste Sites 270 E Glossary of Terms 279 CDP Adopted Version 2020 Contents List of County Durham Plan Policies Policy 1 Quantity of New Development 20 Policy 2 Employment Land 30 Policy 3 Aykley Heads 38 Policy 4 Housing Allocations 47 Policy 5 Durham City's Sustainable Urban Extensions 61 Policy 6 Development on Unallocated Sites 68 Policy 7 Visitor Attractions -

Grand Gardens and Castles Itinerary
Itinerary 2016 ©VisitBritain/Pawel Libera ©VisitBritain/Pawel of Yeare English Garden TRAvEL fact fiLE Car (recommended transport) 87 miles/140 km 2 h 40 min Newcastle International newcastleairport.com Durham Tees Valley durhamteesvalleyairport.com Newcastle nationalrail.co.uk GRAND GARDENS Real-time local information realtimetravelguide.co.uk Morpeth Tourist Information Centre visitnorthumberland.com AND CASTLES Want to see more gardens? Continue your tour with the Magnificent Yorkshire Gardens itinerary. Alnwick Castle This fascinating two-day tour in Northumberland A brief 5-minute drive along the picturesque B6346 will is a must for all Downton Abbey and Harry Potter take you to one of England’s most iconic castles, Alnwick fans. Explore magnificent gardens, historic castles Castle. You may recognise it as it was the location for and visit the very first house in the world to be lit Downton Abbey’s ‘Brancaster Castle’ and Harry Potter’s by hydroelectricity, located in the grounds of an ‘Hogwarts School of Witchcraft and Wizardry’. Full of incredible garden. history on a grand scale, there has been a castle recorded on this site for over 1,000 years. Join in a free tour of the Italianate State Rooms, home to one of the country’s Day 1: The Alnwick Garden • Alnwick Castle ● finest private collections of art and furniture and then • Morpeth on to the vast grounds. Harry Potter fans will love the broomstick training by the resident wizard. Make sure you book your tickets on arrival to secure your training. Take Your day begins at The Alnwick Garden in a well-earned break in the Courtyard Café located behind Northumberland, described by the Duchess of the Clock Tower before a 30-minute drive to the historic Northumberland as “an inspiring landscape with beautiful market town of Morpeth. -
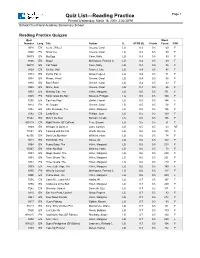
Crystal Reports Activex Designer
Quiz List—Reading Practice Page 1 Printed Wednesday, March 18, 2009 2:36:33PM School: Churchland Academy Elementary School Reading Practice Quizzes Quiz Word Number Lang. Title Author IL ATOS BL Points Count F/NF 9318 EN Ice Is...Whee! Greene, Carol LG 0.3 0.5 59 F 9340 EN Snow Joe Greene, Carol LG 0.3 0.5 59 F 36573 EN Big Egg Coxe, Molly LG 0.4 0.5 99 F 9306 EN Bugs! McKissack, Patricia C. LG 0.4 0.5 69 F 86010 EN Cat Traps Coxe, Molly LG 0.4 0.5 95 F 9329 EN Oh No, Otis! Frankel, Julie LG 0.4 0.5 97 F 9333 EN Pet for Pat, A Snow, Pegeen LG 0.4 0.5 71 F 9334 EN Please, Wind? Greene, Carol LG 0.4 0.5 55 F 9336 EN Rain! Rain! Greene, Carol LG 0.4 0.5 63 F 9338 EN Shine, Sun! Greene, Carol LG 0.4 0.5 66 F 9353 EN Birthday Car, The Hillert, Margaret LG 0.5 0.5 171 F 9305 EN Bonk! Goes the Ball Stevens, Philippa LG 0.5 0.5 100 F 7255 EN Can You Play? Ziefert, Harriet LG 0.5 0.5 144 F 9314 EN Hi, Clouds Greene, Carol LG 0.5 0.5 58 F 9382 EN Little Runaway, The Hillert, Margaret LG 0.5 0.5 196 F 7282 EN Lucky Bear Phillips, Joan LG 0.5 0.5 150 F 31542 EN Mine's the Best Bonsall, Crosby LG 0.5 0.5 106 F 901618 EN Night Watch (SF Edition) Fear, Sharon LG 0.5 0.5 51 F 9349 EN Whisper Is Quiet, A Lunn, Carolyn LG 0.5 0.5 63 NF 74854 EN Cooking with the Cat Worth, Bonnie LG 0.6 0.5 135 F 42150 EN Don't Cut My Hair! Wilhelm, Hans LG 0.6 0.5 74 F 9018 EN Foot Book, The Seuss, Dr. -

Northeast England – a History of Flash Flooding
Northeast England – A history of flash flooding Introduction The main outcome of this review is a description of the extent of flooding during the major flash floods that have occurred over the period from the mid seventeenth century mainly from intense rainfall (many major storms with high totals but prolonged rainfall or thaw of melting snow have been omitted). This is presented as a flood chronicle with a summary description of each event. Sources of Information Descriptive information is contained in newspaper reports, diaries and further back in time, from Quarter Sessions bridge accounts and ecclesiastical records. The initial source for this study has been from Land of Singing Waters –Rivers and Great floods of Northumbria by the author of this chronology. This is supplemented by material from a card index set up during the research for Land of Singing Waters but which was not used in the book. The information in this book has in turn been taken from a variety of sources including newspaper accounts. A further search through newspaper records has been carried out using the British Newspaper Archive. This is a searchable archive with respect to key words where all occurrences of these words can be viewed. The search can be restricted by newspaper, by county, by region or for the whole of the UK. The search can also be restricted by decade, year and month. The full newspaper archive for northeast England has been searched year by year for occurrences of the words ‘flood’ and ‘thunder’. It was considered that occurrences of these words would identify any floods which might result from heavy rainfall. -
Northumberland Local Plan Core Strategy Pre-Submission Draft October 2015 Contents
Northumberland Local Plan Core Strategy Pre-Submission Draft October 2015 Contents Foreword 3 1 Introduction 4 2 A Spatial Portrait of Northumberland – opportunities and challenges 12 3 Spatial vision, objectives and outcomes 29 4 Delivering the vision for Northumberland 37 5 Delivering a thriving and competitive economy 46 6 Providing existing and future communities with a choice of decent, affordable homes 85 7 Green Belt 115 8 Conserving and enhancing Northumberland's distinctive and valued natural, historic, water and built environments 137 9 Ensuring connectivity and infrastructure delivery 180 10 Community well-being 195 11 Managing natural resources 205 12 Implementation 240 Glossary 246 Appendices A Employment land portfolio 262 B Primary Shopping Area and Commercial Centre boundaries 336 C Northumberland housing trajectory 2011 to 2031 348 D Green Belt Inset Boundaries for small settlements 349 E Mineral Safeguarding Areas 380 F Safeguarded minerals infrastructure 385 Northumberland Local Plan Core Strategy - Pre-Submission Draft (October 2015) Foreword Foreword As Cabinet Member for Economic Growth in Northumberland, I am pleased to have overseen recent stages in the preparation of the Northumberland Local Plan 'Core Strategy' – the Council's strategic plan for the development of the County over the next decade and a half. We are now reaching the most crucial stage in the process. Soon we will be sending the Core Strategy to the Government and they will appoint an inspector to decide whether it is a sound plan. But before that, you have one final chance to shape what is in the document. Since 2012, about 5,000 people have taken the opportunity to comment on stages of the Core Strategy and 4,500 have attended drop-in sessions, meetings or workshops.