Sleep Does Not Help Relearning Declarative Memories in Older Adults Emilie Gerbier, Guillaume T
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Emotional Arousal 1 Running Head
Effect of Emotional Arousal 1 Running Head: THE EFFECT OF EMOTIONAL AROUSAL ON RECALL The Effect of Emotional Arousal and Valence on Memory Recall 500181765 Bangor University Group 14, Thursday Afternoon Effect of Emotional Arousal 2 Abstract This study examined the effect of emotion on memory when recalling positive, negative and neutral events. Four hundred and fourteen participants aged over 18 years were asked to read stories that differed in emotional arousal and valence, and then performed a spatial distraction task before they were asked to recall the details of the stories. Afterwards, participants rated the stories on how emotional they found them, from ‘Very Negative’ to ‘Very Positive’. It was found that the emotional stories were remembered significantly better than the neutral story; however there was no significant difference in recall when a negative mood was induced versus a positive mood. Therefore this research suggests that emotional valence does not affect recall but emotional arousal affects recall to a large extent. Effect of Emotional Arousal 3 Emotional arousal has often been found to influence an individual’s recall of past events. It has been documented that highly emotional autobiographical memories tend to be remembered in better detail than neutral events in a person’s life. Structures involved in memory and emotions, the hippocampus and amygdala respectively, are joined in the limbic system within the brain. Therefore, it would seem true that emotions and memory are linked. Many studies have investigated this topic, finding that emotional arousal increases recall. For instance, Kensinger and Corkin (2003) found that individuals remember emotionally arousing words (such as swear words) more than they remember neutral words. -

Sleep, Memory, and Aging: Effects of Pre- and Post- Sleep Delays and Interference on Memory in Younger and Older Adults Michael Scullin Washington University in St
Washington University in St. Louis Washington University Open Scholarship All Theses and Dissertations (ETDs) 1-1-2011 Sleep, Memory, and Aging: Effects of Pre- and Post- Sleep Delays and Interference on Memory in Younger and Older Adults Michael Scullin Washington University in St. Louis Follow this and additional works at: https://openscholarship.wustl.edu/etd Recommended Citation Scullin, Michael, "Sleep, Memory, and Aging: Effects of Pre- and Post-Sleep Delays and Interference on Memory in Younger and Older Adults" (2011). All Theses and Dissertations (ETDs). 640. https://openscholarship.wustl.edu/etd/640 This Dissertation is brought to you for free and open access by Washington University Open Scholarship. It has been accepted for inclusion in All Theses and Dissertations (ETDs) by an authorized administrator of Washington University Open Scholarship. For more information, please contact [email protected]. WASHINGTON UNIVERSITY IN ST. LOUIS Department of Psychology Dissertation Examination Committee: Mark McDaniel, Chair Sandy Hale Larry Jacoby Henry Roediger, III Paul Shaw James Wertsch Sleep, Memory, and Aging: Effects of Pre- and Post-Sleep Delays and Interference on Memory in Younger and Older Adults by Michael K. Scullin A dissertation presented to the Graduate School of Arts and Sciences of Washington University in partial fulfillment of the requirements for the degree of Doctor of Philosophy December 2011 Saint Louis, Missouri Abstract The present research investigated the relationship between sleep and memory in younger and older adults. Previous research has demonstrated that during the deep sleep stage (i.e., slow wave sleep), recently learned memories are reactivated and consolidated in younger adults. -

Working Memory and Cued Recall Max V
Georgia Southern University Digital Commons@Georgia Southern University Honors Program Theses 2016 Working memory and cued recall Max V. Fey 8602950 Karen Naufel Georgia Southern University Lawrence Locker Georgia Southern University Follow this and additional works at: https://digitalcommons.georgiasouthern.edu/honors-theses Part of the Cognitive Psychology Commons Recommended Citation Fey, Max V. 8602950; Naufel, Karen; and Locker, Lawrence, "Working memory and cued recall" (2016). University Honors Program Theses. 220. https://digitalcommons.georgiasouthern.edu/honors-theses/220 This thesis (open access) is brought to you for free and open access by Digital Commons@Georgia Southern. It has been accepted for inclusion in University Honors Program Theses by an authorized administrator of Digital Commons@Georgia Southern. For more information, please contact [email protected]. 1 Working Memory and Cued Recall Working Memory and Cued Recall An Honors Thesis submitted in partial fulfillment of the requirements for Honors in the Department of Psychology. By Maximilian Fey Under the mentorship of Dr. Karen Naufel ABSTRACT Previous research has found that individuals with high working memory have greater recall capabilities than those with low working memory (Unsworth, Spiller, & Brewers, 2012). Research did not test the extent to which cues affect one’s recall ability in relation to working memory. The present study will examine this issue. Participants completed a working memory measure. Then, they were provided with cued recall tasks whereby they recalled Facebook friends. The cues varied to be no cues, ambiguous cues high in imageability, and cues directly related to Facebook. The results showed that there was no difference between individual’s ability to recall their Facebook friends and their working memory scores. -

Post-Encoding Stress Does Not Enhance Memory Consolidation: the Role of Cortisol and Testosterone Reactivity
brain sciences Article Post-Encoding Stress Does Not Enhance Memory Consolidation: The Role of Cortisol and Testosterone Reactivity Vanesa Hidalgo 1,* , Carolina Villada 2 and Alicia Salvador 3 1 Department of Psychology and Sociology, Area of Psychobiology, University of Zaragoza, 44003 Teruel, Spain 2 Department of Psychology, Division of Health Sciences, University of Guanajuato, Leon 37670, Mexico; [email protected] 3 Department of Psychobiology and IDOCAL, University of Valencia, 46010 Valencia, Spain; [email protected] * Correspondence: [email protected]; Tel.: +34-978-645-346 Received: 11 October 2020; Accepted: 15 December 2020; Published: 16 December 2020 Abstract: In contrast to the large body of research on the effects of stress-induced cortisol on memory consolidation in young people, far less attention has been devoted to understanding the effects of stress-induced testosterone on this memory phase. This study examined the psychobiological (i.e., anxiety, cortisol, and testosterone) response to the Maastricht Acute Stress Test and its impact on free recall and recognition for emotional and neutral material. Thirty-seven healthy young men and women were exposed to a stress (MAST) or control task post-encoding, and 24 h later, they had to recall the material previously learned. Results indicated that the MAST increased anxiety and cortisol levels, but it did not significantly change the testosterone levels. Post-encoding MAST did not affect memory consolidation for emotional and neutral pictures. Interestingly, however, cortisol reactivity was negatively related to free recall for negative low-arousal pictures, whereas testosterone reactivity was positively related to free recall for negative-high arousal and total pictures. -

2 Weeks to a Younger Brain Book Publishing
2 WEEKS TO A YOUNGER BRAIN 2 WEEKS TO A YOUNGER BRAIN GARY SMALL, MD AND GIGI VORGAN www.humanixbooks.com Boca Raton, FL, USA Two Weeks to a Younger Brain © 2015 Humanix Books All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any other infor- mation storage and retrieval system, without written permission from the publisher. Interior: Ben Davis Index: Yvette M. Chin For information, contact: Humanix Books P.O. Box 20989 West Palm Beach, FL 33416 USA www.humanixbooks.com email: [email protected] Humanix Books is a division of Humanix Publishing, LLC. Its trademark, consisting of the words “Humanix Books” is registered with the US Patent and Trademark Of- fice, and in other countries. Disclaimer: The information presented in this book is meant to be used for general resource purposes only; it is not intended as specific medical advice for any individ- ual and should not substitute medical advice from a healthcare professional. If you have (or think you may have) a medical problem, speak to your doctor or a healthcare practitioner immediately about your risk and possible treatments. Do not engage in any therapy or treatment without consulting a medical professional. Printed in the United States of America and the United Kingdom. ISBN (Hardcover) 978-1-63006-030-5 ISBN (E-book) 978-1-63006-031-2 Library of Congress Control Number: 2014958068 Acknowledgments E ARE GRATEFUL TO the many volunteers and patients who Wparticipated in the research studies that inspired this book. -

A CROSS-CULTURAL EXAMINATION of EMOTIONAL MEMORY PROCESSING: US Vs
Journal of Integrated Social Sciences www.jiss.org, 2014 - 4(1): 1-17 Original Article: A CROSS-CULTURAL EXAMINATION OF EMOTIONAL MEMORY PROCESSING: US vs. AFGHANISTAN Frishta Sharifi, M.S. Mills College, USA Christie Chung, Ph.D. Mills College, USA Abstract A positivity effect where older adults remember positive information better than young adults has been documented widely in the memory literature. However, research on the generalizability of the positivity effect to non-western cultures is still in its infancy. The present study is the first in the field of memory to explore the differences in emotional memory patterns between the US and Afghan cultures. Due to the war in Afghanistan, we hypothesized that the Afghan older adults’ negative life experiences may reduce the effect of the positivity effect usually found in the US. In the present study, we tested young and older US and Afghan adults on an emotional picture memory task consisted of 30 pictures (10 positive, 10 negative, 10 neutral). They were later asked to recall these pictures using brief verbal descriptions. US older adults remembered significantly fewer negative pictures compared to US young adults, demonstrating a positivity effect in old age. Afghan adults, however, did not show an age-related positivity effect in memory as predicted. We discussed our results with the framework of current socio-emotional theories. Keywords: Aging, emotional memory, positivity effect, cross-cultural __________________ AUTHOR NOTE: Please address all correspondence to: Dr. Christie Chung, Mills College Psychology Department, 5000 MacArthur Blvd., Oakland, CA 94613. Email: [email protected] © 2014 Journal of Integrated Social Sciences Sharifi & Chung Emotional Memory: US vs. -
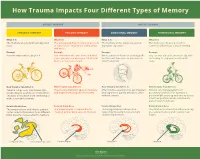
How Trauma Impacts Four Different Types of Memory
How Trauma Impacts Four Different Types of Memory EXPLICIT MEMORY IMPLICIT MEMORY SEMANTIC MEMORY EPISODIC MEMORY EMOTIONAL MEMORY PROCEDURAL MEMORY What It Is What It Is What It Is What It Is The memory of general knowledge and The autobiographical memory of an event The memory of the emotions you felt The memory of how to perform a facts. or experience – including the who, what, during an experience. common task without actively thinking and where. Example Example Example Example You remember what a bicycle is. You remember who was there and what When a wave of shame or anxiety grabs You can ride a bicycle automatically, with- street you were on when you fell off your you the next time you see your bicycle out having to stop and recall how it’s bicycle in front of a crowd. after the big fall. done. How Trauma Can Affect It How Trauma Can Affect It How Trauma Can Affect It How Trauma Can Affect It Trauma can prevent information (like Trauma can shutdown episodic memory After trauma, a person may get triggered Trauma can change patterns of words, images, sounds, etc.) from differ- and fragment the sequence of events. and experience painful emotions, often procedural memory. For example, a ent parts of the brain from combining to without context. person might tense up and unconsciously make a semantic memory. alter their posture, which could lead to pain or even numbness. Related Brain Area Related Brain Area Related Brain Area Related Brain Area The temporal lobe and inferior parietal The hippocampus is responsible for The amygdala plays a key role in The striatum is associated with producing cortex collect information from different creating and recalling episodic memory. -

Sherman Dissertation
Copyright by Stephanie Michelle Sherman 2016 The Dissertation Committee for Stephanie Michelle Sherman certifies that this is the approved version of the following dissertation: Associations between sleep and memory in aging Committee: David Schnyer, Supervisor Christopher Beevers Andreana Haley Carmen Westerberg Associations between sleep and memory in aging by Stephanie Michelle Sherman, B.S. DISSERTATION Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY The University of Texas at Austin May 2016 Acknowledgements First, I would like to thank my advisor, David Schnyer, for his guidance and mentorship. He challenged me to think critically about research questions, analyses, and the theoretical implications of our work. Over the course of 5 years, he opened the door to countless opportunities that have given me the confidence to tackle any research question. I would also like to thank my committee members: Chris Beevers, Andreana Haley, and Carmen Westerberg for their thoughtful comments and discussion. I am grateful for Corey White’s assistance on understanding and implementing the diffusion model. Jeanette Mumford and Greg Hixon were critical to advancing my understanding of statistics. From the Schnyer lab, I would especially like to thank Nick Griffin, Katy Seloff, Bridget Byrd, and Sapana Donde for their great conversations, insight, and friendship. I must acknowledge the incredible research assistants in the Schnyer lab who were willing to stay up all night to answer critical questions about sleep and memory in older adults, especially Jasmine McNeely, Mehak Gupta, Jiazhou Chen, Haley Bednarz, Tolan Nguyen, and Angela Murira. -

Cognitive and Neuropsychological Aspects of Age-Associated Memory Dysfunction
COGNITIVE AND NEUROPSYCHOLOGICAL ASPECTS OF AGE-ASSOCIATED MEMORY DYSFUNCTION A k a d e m is k a v h a n d l in g som för avläggande av filosofie doktorsexamen med vederbörligt tillstånd av rektorsämbetet vid Umeå universitet framlägges för offentlig granskning vid Psykologiska institutionen, Umeå Universitet, Seminarierum 2, fredagen den 24 januari 1992, klockan 10.15 AV Th o m a s K a r l s s o n Psykologiska institutionen, Umeå Universitet, Umeå COGNITIVE AND NEUROPSYCHOLOGICAL ASPECTS OF AGE- ASSOCIATED MEMORY DYSFUNCTION BY Thom as K arlsson Doctoral Dissertation Department of Psychology, University of Umeå, Umeå, Sweden ABSTRACT Memory dysfunction is common in association with the course of normal aging. Memory dysfunction is also obligatory in age-associated neurological disorders, such as Alzheimer’s disease. However, despite the ubiquitousness of age-related memory decline, several basic questions regarding this entity remain unanswered. The present investigation addressed two such questions: (1) Can individuals suffering from memory dysfunction due to aging and amnesia due to Alzheimer’s disease improve memory performance if contextual support is provided at the time of acquisition of to-be- remembered material or reproduction of to-be-remembered material? (2) Are memory deficits observed in ‘younger’ older adults similar to the deficits observed in ‘older’ elderly subjects, Alzheimer’s disease, and memory dysfunction in younger subjects? The outcome of this investigation suggests an affirmative answer to the first question. Given appropriate support at encoding and retrieval, even densely amnesic patients can improve their memory performance. As to the second question, a more complex pattern emerges. -

Effect of the Time-Of-Day of Training on Explicit Memory
Time-of-dayBrazilian Journal of training of Medical and memory and Biological Research (2008) 41: 477-481 477 ISSN 0100-879X Effect of the time-of-day of training on explicit memory F.F. Barbosa and F.S. Albuquerque Departamento de Fisiologia, Universidade Federal do Rio Grande do Norte, Natal, RN, Brasil Correspondence to: F.F. Barbosa, Departamento de Fisiologia, Universidade Federal do Rio Grande do Norte, Lagoa Nova, Caixa Postal 1511, 59072-970 Natal, RN, Brasil Fax: +55-84-211-9206. E-mail: [email protected] Studies have shown a time-of-day of training effect on long-term explicit memory with a greater effect being shown in the afternoon than in the morning. However, these studies did not control the chronotype variable. Therefore, the purpose of this study was to assess if the time-of-day effect on explicit memory would continue if this variable were controlled, in addition to identifying the occurrence of a possible synchronic effect. A total of 68 undergraduates were classified as morning, intermediate, or afternoon types. The subjects listened to a list of 10 words during the training phase and immediately performed a recognition task, a procedure which they repeated twice. One week later, they underwent an unannounced recognition test. The target list and the distractor words were the same in all series. The subjects were allocated to two groups according to acquisition time: a morning group (N = 32), and an afternoon group (N = 36). One week later, some of the subjects in each of these groups were subjected to a test in the morning (N = 35) or in the afternoon (N = 33). -

High 1 Effectiveness of Echoic and Iconic Memory in Short-Term and Long-Term Recall Courtney N. High 01/14/13 Mr. Mengel Psychol
High 1 Effectiveness of Echoic and Iconic Memory in Short-term and Long-term Recall Courtney N. High 01/14/13 Mr. Mengel Psychology 1 High 2 Abstract Objective: To see whether iconic memory or echoic memory is more effective at being stored and recalled as short-term and long-term memory in healthy adults. Method: Eight healthy adults between the ages of 18 and 45 were tested in the study. Participants were shown a video containing ten pictures and ten sounds of easily recognizable objects. Participants were asked to recall as many items as they could immediately after the video and were then asked again after a series of questions. Results: In younger adults more visual objects are able to be recalled both short and long term, but with older adults, in short term recall, the same number of sound and visual items where remembered, and with long term recall, sound items were remembered slightly better. Results also showed that iconic memory fades faster than echoic memory. Conclusion: The ability to store and recall iconic and echoic information both short and long term varies with age. The study has several faults including relying on self-reporting on health for participants, and testing environments not being quiet in all tests. Introduction There are three main different types of memory: Sensory memory, short-term memory, and long-term memory. Sensory memory deals with the brief storage of information immediately after stimulation. Sensory memory is then converted to short-term memory if deemed necessary by the brain where it is held. After that, some information will then be stored as long-term memory for later recall. -

2.33 Implicit Memory and Priming W
2.33 Implicit Memory and Priming W. D. Stevens, G. S. Wig, and D. L. Schacter, Harvard University, Cambridge, MA, USA ª 2008 Elsevier Ltd. All rights reserved. 2.33.1 Introduction 623 2.33.2 Influences of Explicit Versus Implicit Memory 624 2.33.3 Top-Down Attentional Effects on Priming 626 2.33.3.1 Priming: Automatic/Independent of Attention? 626 2.33.3.2 Priming: Modulated by Attention 627 2.33.3.3 Neural Mechanisms of Top-Down Attentional Modulation 629 2.33.4 Specificity of Priming 630 2.33.4.1 Stimulus Specificity 630 2.33.4.2 Associative Specificity 632 2.33.4.3 Response Specificity 632 2.33.5 Priming-Related Increases in Neural Activation 634 2.33.5.1 Negative Priming 634 2.33.5.2 Familiar Versus Unfamiliar Stimuli 635 2.33.5.3 Sensitivity Versus Bias 636 2.33.6 Correlations between Behavioral and Neural Priming 637 2.33.7 Summary and Conclusions 640 References 641 2.33.1 Introduction stimulus that result from a previous encounter with the same or a related stimulus. Priming refers to an improvement or change in the When considering the link between behavioral identification, production, or classification of a stim- and neural priming, it is important to acknowledge ulus as a result of a prior encounter with the same or that functional neuroimaging relies on a number of a related stimulus (Tulving and Schacter, 1990). underlying assumptions. First, changes in informa- Cognitive and neuropsychological evidence indi- tion processing result in changes in neural activity cates that priming reflects the operation of implicit within brain regions subserving these processing or nonconscious processes that can be dissociated operations.