Crackcast E146 – Radiation Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
RADIATION EFFECTS and SOURCES What Is Radiation? What Does Radiation Do to Us? Where Does Radiation Come From?
RADIATION EFFECTS and SOURCES What is radiation? What does radiation do to us? Where does radiation come from? United Nations Environment Programme RADIATION EFFECTS and SOURCES What is radiation? What does radiation do to us? Where does radiation come from? United Nations Environment Programme DISCLAIMER This publication is largely based on the findings of the United Nations Scientific Committee on the Effects of Atomic Radiation, a subsidiary body of the United Nations General Assembly and for which the United Nations Environment Pro- gramme provides the secretariat. This publication does not necessarily r epresent the views of the Scientific Committee or of the United Nations Environment Programme. The designations employed and the presentation of the material in this publica- tion do not imply the expression of any opinion whatsoever on the part of the United Nations Environment Programme concerning the legal status of any country, territory, city or area or of its authorities, or concerning delimitation of its frontiers or boundaries. This publication may be reproduced in whole or in part and in any form for educational or non-profit purposes without special permission from the copyright holder, provided acknowledgement of the source is made. The United Nations Environment Programme would appreciate receiving a copy of any publication that uses this publication as a source. No use of this publication may be made for resale or for any other commercial purpose whatsoever without prior permission in writing from the United Nations Environment Programme. The United Nations Environment Programme promotes environmentally sound practices globally and in its own activities. This publication was printed on recycled paper, 100 per cent chlorine free. -

GHOST GEAR: the ABANDONED FISHING NETS HAUNTING OUR OCEANS Sea Turtle Entangled in Fishing Gear in the Mediterranean Sea © Marco Care/Greenpeace CONTENTS
GHOST GEAR: THE ABANDONED FISHING NETS HAUNTING OUR OCEANS Sea turtle entangled in fishing gear in the Mediterranean Sea © Marco Care/Greenpeace CONTENTS 4 Zusammenfassung 5 Executive summary 6 Introduction 8 Main types of fishing – Nets – Lines – Traps & pots – FADs 11 Ghost gear impacts – Killing ocean creatures – Damaging habitats – Economic and other impacts 13 Current regulations – International agreements and recommendations – Other programmes and resolutions – A cross-sector approach – The need for a Global Ocean Treaty 16 References 2019 / 10 Published by Greenpeace Germany November 2019 Stand Greenpeace e. V., Hongkongstraße 10, 20457 Hamburg, Tel. 040/3 06 18 - 0, [email protected] , www . greenpeace . de Authors Karli Thomas, Dr. Cat Dorey and Farah Obaidullah Responsible for content Helena Spiritus Layout Klasse 3b, Hamburg S 0264 1 Contents 3 DEUTSCHE ZUSAMMENFASSUNG DER STUDIE GHOST GEAR: THE ABANDONED FISHING NETS HAUNTING OUR OCEANS → Rund 640.000 Tonnen altes Fischereigerät inklusive Geisternetzen, Bojen, Leinen, Fallen und Körbe landen jährlich als Fischereimüll in den Ozeanen. → Weltweit trägt altes Fischereigerät zu etwa zehn Prozent zum Plastikeintrag in die Meere bei. → 45 Prozent aller Arten auf der Roten IUCN-Liste hatten bereits Kontakt mit Plastik im Meer. → Sechs Prozent aller eingesetzten Netze, neun Prozent aller Fallen und 29 Prozent aller Langleinen gehen jährlich auf den Ozeanen verloren und enden als Meeresmüll. → Treibnetze, Fallen und Fischsammler (Fish Aggregating Devices, FADs) gehen weltweit am häufigsten als Müll auf den Ozeanen verloren und bergen die meisten Risiken für Meereslebewesen. → Durch FADs sterben 2,8 bis 6,7 Mal mehr Tiere - darunter bedrohte Arten wie Haie – als Beifang als die Zielarten, für die sie eingesetzt werden. -

Glossary Derived From: Human Research Program Integrated Research Plan, Revision A, (January 2009)
Glossary derived from: Human Research Program Integrated Research Plan, Revision A, (January 2009). National Aeronautics and Space Administration, Johnson Space Center, Houston, Texas 77058, pages 232-280. Report No. 153: Information Needed to Make Radiation Protection Recommendations for Space Missions Beyond Low-Earth Orbit (2006). National Council on Radiation Protection and Measurements, pages 309-318. Reprinted with permission of the National Council on Radiation Protection and Measurements, http://NCRPonline.org . Managing Space Radiation Risk in the New Era of Space Exploration (2008). Committee on the Evaluation of Radiation Shielding for Space Exploration, National Research Council. National Academies Press, pages 111-118. -A- AAPM: American Association of Physicists in Medicine. absolute risk: Expression of excess risk due to exposure as the arithmetic difference between the risk among those exposed and that obtaining in the absence of exposure. absorbed dose (D): Average amount of energy imparted by ionizing particles to a unit mass of irradiated material in a volume sufficiently small to disregard variations in the radiation field but sufficiently large to average over statistical fluctuations in energy deposition, and where energy imparted is the difference between energy entering the volume and energy leaving the volume. The same dose has different consequences depending on the type of radiation delivered. Unit: gray (Gy), equivalent to 1 J/kg. ACE: Advanced Composition Explorer Mission, launched in 1997 and orbiting the L1 libration point to sample energetic particles arriving from the Sun and interstellar and galactic sources. It also provides continuous coverage of solar wind parameters and solar energetic particle intensities (space weather). When reporting space weather, it can provide an advance warning (about one hour) of geomagnetic storms that can overload power grids, disrupt communications on Earth, and present a hazard to astronauts. -
Training for Radiation Emergencies: First Responder Operations
TRAINING FOR RADIATION EMERGENCIES: FIRST RESPONDER OPERATIONS STUDENT TEXT Developed by THE INTERNATIONAL ASSOCIATION OF FIRE FIGHTERS ® Alfred K. Whitehead Vincent J. Bollon General President General Secretary-Treasurer Copyright © 1998 International Association of Fire Fighters 1750 New York Avenue, N.W. Washington, D.C. 20006 THE INTERNATIONAL ASSOCIATION OF FIRE FIGHTERS ® Alfred K. Whitehead Vincent J. Bollon General President General Secretary-Treasurer Bradley M. Sant, Director Hazardous Materials Training The IAFF acknowledges the Hazardous Materials Training staff: Kimberly Lockhart, Michael Lucey, Diane Dix Massa, A. Christopher Miklovis, Carol Mintz, Michael Schaitberger, Scott Solomon, Linda Voelpel Casey, and consultants Jo Griffith, Eric Lamar, and Margaret Veroneau for their work in developing this manual. In addition, the IAFF thanks Paul Deane,Tommy Erickson, and Charlie Wright for their contributions to this project. Notice This manual was prepared as an account of work sponsored by an agency of the United States Government. Neither the United States government nor any agency thereof, nor any of their employees, nor any of their contractors, subcontractors nor their employees, make any warranty, expressed or implied, or assume any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represent that its use would not infringe upon privately-owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government or any agency thereof. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government or any agency thereof. -

Municipal Solid Waste Landfill Operation and Management Workbook
MUNICIPAL SOLID WASTE LANDFILL OPERATION AND MANAGEMENT WORKBOOK Revised April 2018 Preface In many ways, constructing, operating and maintaining a municipal solid waste landfill is similar to constructing, operating, and maintaining a highway, dam, canal, bridge, or other engineered structure. The most important similarity is that landfills, like other engineered structures, must be constructed and operated in a manner that will provide safe, long-term, and reliable service to the communities they serve. Proper design, construction, operation, monitoring, closure and post-closure care are critical because after disposal the waste can be a threat to human health and the environment for decades to centuries. This workbook is intended to provide municipal landfill operators and managers in Wyoming with the fundamental knowledge and technical background necessary to ensure that landfills are operated efficiently, effectively, and in a manner that is protective of human health and the environment. This workbook contains information regarding basic construction and operation activities that are encountered on a routine basis at most landfills. The basic procedures and fundamental elements of landfill permitting, construction management, monitoring, closure, post-closure care, and financial assurance are also addressed. The workbook includes informative tips and information that landfill operators and managers can use to conserve landfill space, minimize the potential for pollution, reduce operating costs, and comply with applicable rules and regulations. In addition to this workbook, operators and managers need to become familiar with the Wyoming Solid Waste Rules and Regulations applicable to municipal solid waste. The DEQ also provides numerous guidelines that may help understand regulatory requirements in more detail. -

Cherenkov Radiation
TheThe CherenkovCherenkov effecteffect A charged particle traveling in a dielectric medium with n>1 radiates Cherenkov radiation B Wave front if its velocity is larger than the C phase velocity of light v>c/n or > 1/n (threshold) A β Charged particle The emission is due to an asymmetric polarization of the medium in front and at the rear of the particle, giving rise to a varying electric dipole momentum. dN Some of the particle energy is convertedγ = 491into light. A coherent wave front is dx generated moving at velocity v at an angle Θc If the media is transparent the Cherenkov light can be detected. If the particle is ultra-relativistic β~1 Θc = const and has max value c t AB n 1 cosθc = = = In water Θc = 43˚, in ice 41AC˚ βct βn 37 TheThe CherenkovCherenkov effecteffect The intensity of the Cherenkov radiation (number of photons per unit length of particle path and per unit of wave length) 2 2 2 2 2 Number of photons/L and radiation d N 4π z e 1 2πz 2 = 2 1 − 2 2 = 2 α sin ΘC Wavelength depends on charge dxdλ hcλ n β λ and velocity of particle 2πe2 α = Since the intensity is proportional to hc 1/λ2 short wavelengths dominate dN Using light detectors (photomultipliers)γ = sensitive491 in 400-700 nm for an ideally 100% efficient detector in the visibledx € 2 dNγ λ2 d Nγ 2 2 λ2 dλ 2 2 11 1 22 2 d 2 z sin 2 z sin 490393 zz sinsinΘc photons / cm = ∫ λ = π α ΘC ∫ 2 = π α ΘC 2 −− 2 = α ΘC λ1 λ1 dx dxdλ λ λλ1 λ2 d 2 N d 2 N dλ λ2 d 2 N = = dxdE dxdλ dE 2πhc dxdλ Energy loss is about 104 less hc 2πhc than 2 MeV/cm in water from € -

AFRRI Biodosimetry Worksheet
Armed Forces Radiobiology Research Institute Biodosimetry Worksheet (Medical Record of Radiation Dose, Contamination, and Acute Radiation Sickness Response) Reporting Authority (person(s) creating this page of the report) Last name: First name: Country of origin: Unit: Phone: Fax: Email: Location: Date (yymmdd): Time: Casualty Last name: First name: Rank: Country of origin: Parent unit: Parent unit location: Parent unit phone: Unit e-mail: Unit fax: Casualty location: History of presenting injury (conventional and/or radiation): History of previous radiation exposure: Past medical history (general): Medical countermeasures (e.g., antiemetics, transfusion), specify: Administered (where, when, route): Exposure conditions Date of exposure (yymmdd): Exposure location: Time of exposure: Weather conditions (at time of exposure): Exposure results Describe incident: External exposure overview Contamination overview Body exposure: Total Partial Uncertain External contamination: Yes No Shielding confounder: Yes No Internal contamination: Yes No Contaminated wound: Yes No If wound(s) are radiation contaminated, please provide details here: Biodosimetric assays overview Sampling date, time Estimated time Dose Reference radiation quality yymmdd (time) post-exposure (h) (Gy) and dose rate (Gy/min) Time onset of vomiting: Lymphocyte counts or depletion kinetics: Urine bioassay: Cytogenetic biodosimetry: Other: ARS response category overview (maximum grading 0-4; see pages 4 through 6 for guidance) N: C: G: H: = RC: days after radiation exposure: AFRRI -
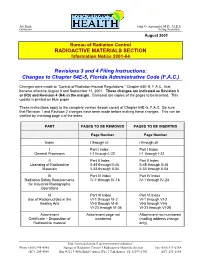
RADIOACTIVE MATERIALS SECTION Revisions 3 and 4 Filing Instructions
Jeb Bush John O. Agwunobi, M.D., M.B.A Governor Acting Secretary August 2001 Bureau of Radiation Control RADIOACTIVE MATERIALS SECTION Information Notice 2001-04 Revisions 3 and 4 Filing Instructions: Changes to Chapter 64E-5, Florida Administrative Code (F.A.C.) Changes were made to “Control of Radiation Hazard Regu lations,” Chapter 64E-5, F.A.C., that became effective August 8 and September 11, 2001. These changes are indicated as Revision 3 or (R3) and Revision 4 (R4) in the margin. Enclosed are copies of the pages to be inserted. This update is printed on blue paper. These instructions apply to the complete version (brown cover) of Chapter 64E -5, F.A.C. Be sure that Revision 1 and Revision 2 changes have been made before making these changes. This can be verified by checking page ii of the index. PART PAGES TO BE REMOVED PAGES TO BE INSERTED Page Number Page Number Index i through xii i through xii I Part I Index Part I Index General Provisions I-1 through I-22 I-1 through I-22 II Part II Index Part II Index Licensing of Radioactive II-45 through II-46 II-45 through II-46 Materials II-53 through II-54 II-53 through II-54 IV Part IV Index Part IV Index Radiation Safety Requirements IV-1 through IV-16 IV-1 through IV-24 for Industrial Radiographic Operations VI Part VI Index Part VI Index Use of Radionuclides in the VI-1 through VI-2 VI-1 through VI-2 Healing Arts VI-5 through VI-6 VI-5 through VI-6 VI-23 through VI-26 VI-23 through VI-26 Attachment Attachment page not Attachment not numbered Certificate – Disposition of numbered (mailing -

Radiation Burn / Dermatitis, Chemical Burn & Necrobiosis Lipodica Case Studies
Radiation Burn / Dermatitis, Chemical Burn & Necrobiosis Lipodica Case Studies By: Jeanne Alvarez, FNP, CWS, Independent Medical Associates, Bangor, ME Radiation Burn / Dermatitis Case Study 1: 63 year old female S/P lumpectomy with chemotherapy and radiation to the breast. She developed a burn to the area with noted dermatitis at the completion of radiation treatments. Area was very painful and blistered. Hydrofera Blue radiation dressing was applied and held in place with netting. There was significant pain reduction reported within hours of application. Wounds healed in 17 days of starting therapy. Started Healed in 17 Days Radiation Burn / Dermatitis Case Study 2: 85 year old male S/P excision of Squamous cell carcinoma of the right temple x 2, the second excision prompted the surgeon to treat area with radiation. The radiation caused the patient’s skin to burn and develop a dermatitis surrounding the wound. Started Hydrofera Blue on patient and he healed in 83 days. Started Healed in 83 Days Chemical Burn Necrobiosis Lipodica Case Study 1: 57 year old male spraying Case Study 1: 48 year old female with wounds on shins. Wounds present for 3 years. insecticide containing the cyhalothrin, Treated at wound care center and given diagnosis of pyoderma gangrenosum, tried came into contact with hands and arms. multiple treatments resulting in thick black and flesh colored eschar which festered and Flushed area with water after contact. drained on regular basis. Wounds did not resemble pyoderma gangrenosum, debrided Within 24 hours of exposure, developed eschar and obtained biopsy, which provided diagnosis of necrobiosis lipodica. Work-up for painful 10/10 blisters. -

Digital Radiation Monitor Is a Health and Safety Instrument That Measures Alpha, Digital Radiation Monitor Beta, and Gamma Radiation
1 Introduction The Digital Radiation Monitor is a health and safety instrument that measures alpha, Digital Radiation Monitor beta, and gamma radiation. With the Digital Radiation Monitor, you can: • Monitor possible radiation exposure while working near radionuclides (Order Code DRM-BTD) • Ensure compliance with regulatory standards Contents • Check for leakage from X-ray machines and other sources • Screen for environmental contamination or environmental sources of 1 Introduction ............................................................................................................. 2 radioactivity How the DRM Detects Radiation ................................................................. 2 • Connect the Digital Radiation Monitor to a computer or data logger to record 2 Features ................................................................................................................... 3 and tabulate your data The Display................................................................................................... 3 The Switches ................................................................................................4 This manual gives complete instructions for using the Digital Radiation Monitor and The Detector..................................................................................................5 procedures for common applications. The Ports....................................................................................................... 5 3 Operation................................................................................................................ -

Release of Patients Administered Radioactive Materials
NEW YORK STATE DEPARTMENT OF HEALTH BUREAU OF ENVIRONMENTAL RADIATION PROTECTION DRAFT RADIATION GUIDE 10.17 RELEASE OF PATIENTS ADMINISTERED RADIOACTIVE MATERIALS A. INTRODUCTION Section 16.123(b) of 10 NYCRR Part 16 requires licensees to assess the radiation exposure to individuals from patients administered radioactive materials and take action, as appropriate, to reduce exposures to other individuals. These requirements apply for both diagnostic and therapeutic uses regardless of the amount administered. Section 16.123(b), Medical uses of radioactive material, states: P The licensee shall confine patients undergoing procedures authorized by ...until the total effective dose equivalent for the individuals (other than the patient) likely to receive the greatest dose is 5 mSv (500 mrem) or less. P When the total effective dose equivalent to any individual that could result from the release of a patient is likely to exceed 1 mSv (100 mrem), the licensee shall: • provide the patient, or his/her competent representative, written information on risks of radiation and methods for reducing the exposure of individuals; and • keep records of such patients release for a period of five years. This document is designed to provide guidance on determining the potential dose to an individual likely to receive the highest dose from exposure to the patient, to establish appropriate activities and dose rates for release, to provide guidelines for instructions to patients on how to reduce exposures to other individuals, to describe recordkeeping requirements, and to inform licensees of other potential problems associated with the release of patients containing radioactive materials. B. DISCUSSION The radiation dose to another individual from a patient is highly dependent on a number of factors, including the amount and type of radioactive material administered, the patient's living/working arrangements, ability/willingness to follow instructions, etc. -

Industrial Radiography
RADIATION PROTECTION OF WORKERS Industrial Radiography RADIATION AND RADIOGRAPHS RADIOACTIVE SOURCES PROCEDURES RADIOGRAPHERS DO follow the procedures. Ionizing radiation can pen- Materials of higher den Sealed sources are small þ Safe storage Precautions þ DO use the appropriate equipment, including collimators. in size and contain material etrate objects and create sity absorb more radiation. þ DO confi rm that there are no other people working in the images on photographic The metal components are which emits penetrating area of radiography. fi lm. The technique is revealed inside this tele radiation continuously. Radioactive sources should be kept in a secure, fi re þ DO use clear working signs and signals. called radiography and phone because they have Special containers made þ DO set up the controlled area and the necessary barriers. the processed fi lms are absorbed more radiation of dense metal shielding resistant and adequately shielded storage location þ DO confi rm the location of the source, or that X rays are called radiographs. than the surrounding plastic. are necessary to store, not being generated, by use of a survey meter. when not in use, and should move and manipulate these þ DO secure and store the source or X ray machine when sources. Due to their small be kept separate from other not in use. materials. The storage loca- size and manoeuvrability, Portable and mobile radiographic þ DO wear your personal dosimeter. sealed sources can be containers. ~ tion for X ray machines that used in confined spaces. are not in use is not required to be shielded. OTHER WORKERS Iridium-192 is a common radioactive source used þ DO observe the access restrictions, however remote it may in gamma radiography.