Scheuermann's Disease As a Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OMM PRACTICAL EXAM Saroj Misra, DO, FACOFP Rachel Nixon, DO Marissa Rogers, DO Family Medicine Goals/Objectives
OMM PRACTICAL EXAM Saroj Misra, DO, FACOFP Rachel Nixon, DO Marissa Rogers, DO Family Medicine Goals/Objectives • Review Exam Day procedure • Understand scoring process • Discuss possible cases and 2 OMM techniques that may be used for each case Disclaimer: The material being presented is NOT necessarily identical to what will be tested upon. We are not affiliated with the actual exam. This is our approach to the practical exam material. EXAM DAY Exam day • You will be assigned a time slot based on your last name • You will select a partner within your time slot • May not partner with a spouse or relative • You will be asked to sign a waiver stating that if you choose to do HVLA you will not perform the corrective “thrust” • You will then stand in line with your partner and await entering the testing room Exam day • There will be two rooms - one in which you will review cases and the second where you will be tested • Once you enter the first room you will not be able to leave • If you DO leave, both you and your partner will be given new cases Exam day • You will be given 3 cases: • Spine • Extremities • Systemic Disease • You will enter your name, ID number and your partners ID number on each case before turning them over Exam day • Each case will have the following information: • HPI • PMH • PSH • FHx • SocHx • There will be multiple choice for the best answer for your diagnosis • You will have 20 minutes to choose the best answer and plan a treatment strategy for each of your cases Exam day • After the 20 minutes are complete, you will -

1 the Thoracic Wall I
AAA_C01 12/13/05 10:29 Page 8 1 The thoracic wall I Thoracic outlet (inlet) First rib Clavicle Suprasternal notch Manubrium 5 Third rib 1 2 Body of sternum Intercostal 4 space Xiphisternum Scalenus anterior Brachial Cervical Costal cartilage plexus rib Costal margin 3 Subclavian 1 Costochondral joint Floating ribs artery 2 Sternocostal joint Fig.1.3 3 Interchondral joint Bilateral cervical ribs. 4 Xiphisternal joint 5 Manubriosternal joint On the right side the brachial plexus (angle of Louis) is shown arching over the rib and stretching its lowest trunk Fig.1.1 The thoracic cage. The outlet (inlet) of the thorax is outlined Transverse process with facet for rib tubercle Demifacet for head of rib Head Neck Costovertebral T5 joint T6 Facet for Tubercle vertebral body Costotransverse joint Sternocostal joint Shaft 6th Angle rib Costochondral Subcostal groove joint Fig.1.2 Fig.1.4 A typical rib Joints of the thoracic cage 8 The thorax The thoracic wall I AAA_C01 12/13/05 10:29 Page 9 The thoracic cage Costal cartilages The thoracic cage is formed by the sternum and costal cartilages These are bars of hyaline cartilage which connect the upper in front, the vertebral column behind and the ribs and intercostal seven ribs directly to the sternum and the 8th, 9th and 10th ribs spaces laterally. to the cartilage immediately above. It is separated from the abdominal cavity by the diaphragm and communicates superiorly with the root of the neck through Joints of the thoracic cage (Figs 1.1 and 1.4) the thoracic inlet (Fig. -

Neurogenic Thoracic Outlet Syndrome
NEUROGENIC THORACIC OUTLET SYNDROME Karl A. Illig, MD, and Mathew Wooster, MD Perhaps no condition treated by vascular surgeons has been up undergoing thoracic outlet decompression. Although associated with more confusion, subjectivity, and nihilism at least two high outliers exist (Denver and St. Louis, with than neurogenic thoracic outlet syndrome (NTOS). Why is UCLA, Johns Hopkins, and several other practices also candi- this, a nerve compression syndrome, even treated by vascular dates), it is estimated that the 10 or 15 high-volume American surgeons? How is it diagnosed, and what other conditions TOS centers perform between 30 and 50 first rib excisions mimic its symptoms? Who should undergo treatment, and yearly, 75% or so for neurogenic symptoms. what exactly does treatment consist of? Is it a real entity or Although several notable thoracic surgeons and neuro- simply just one end of a continuum that is probably just a part surgeons have significant interest in NTOS, the vast majority of normal physiology? of these cases are treated by vascular surgeons. The reasons are The thoracic outlet is the area of the body at the base of the obscure, but almost certainly a large part of this arose from the neck and upper chest and shoulder region that contains the fact that “vascular” TOS —arterial and, more recently, venous nerves, artery, and vein as they pass from the upper extrem- pathology—was the first form to be recognized, and vascular ity to the spine and thorax [see Figure 1]. Each of these three surgeons initiated investigation and treatment of problems in structures can be compressed by abnormal anatomy in one of this area. -
Thoracic Outlet Syndrome Anaesthesia Tutorial of the Week 286
Sign up to receive ATOTW weekly - email [email protected] THORACIC OUTLET SYNDROME ANAESTHESIA TUTORIAL OF THE WEEK 286 17TH JUNE 2013 Dr Sandeep Kusre, Dr Richard Telford Royal Devon & Exeter Hospital, United Kingdom Correspondence to [email protected] QUESTIONS Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. 1. Which of the following are transmitted through the thoracic outlet? a. Internal jugular vein b. Thoracic duct c. Trachea d. Oesophagus e. Brachial plexus 2. List 5 different causes of thoracic outlet syndrome. 3. The following are important anaesthetic considerations in surgical correction of thoracic outlet syndrome. a. Risk of haemorrhage b. Risk of air embolus c. Invasive monitoring with an arterial line is often required d. Post-operative bleeding will be seen by closely monitoring losses into drains e. All patients should have a chest x-ray performed in recovery INTRODUCTION Thoracic outlet syndrome (TOS) refers to a constellation of symptoms caused by compression of the neurovascular bundle of the upper limb as they pass between the uppermost rib and clavicle en route to the axilla. Precise symptoms depend on the component affected – the brachial plexus, subclavian artery or subclavian vein – giving rise to neurogenic, arterial or venous TOS, respective AETIOLOGY Compression of the neurovascular bundle can be caused by congenital or acquired soft tissue and bony abnormalities. (table 1) Any process that narrows the passage through which these important neurovascular structures pass can lead to symptoms of thoracic outlet syndrome. Major locations of compression of the neurovascular structures include over the first rib, behind pectoralis minor and within the scalene muscle triangle. -
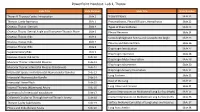
Powerpoint Handout: Lab 1, Thorax
PowerPoint Handout: Lab 1, Thorax Slide Title Slide Number Slide Title Slide Number Thorax & Thoracic Cavity: Introduction Slide 2 Visceral Pleura Slide 21 Thoracic Cavity Apertures Slide 3 Pneumothorax, Pleural Effusion, Hemothorax Slide 22 Osseous Thorax: Sternum Slide 4 Types of Pneumothorax Slide 23 Osseous Thorax: Sternal Angle and Transverse Thoracic Plane Slide 5 Pleural Recesses Slide 24 Osseous Thorax: Ribs Slide 6 Costodiaphragmatic Recess and Costophrenic Angle Slide 25 Osseous Thorax: Ribs Slide 7 Pleurisy and Referred Pain Slide 26 Osseous Thorax: Ribs Slide 8 Diaphragm Introduction Slide 27 Supernumerary Ribs Slide 9 Diaphragm Apertures Slide 28 Osseous Thorax: Rib Joints Slide 10 Diaphragm Motor Innervation Slide 29 Muscular Thorax: Intercostal Muscles Slide 11 Diaphragm Movements Slide 30 Muscular Thorax: Intercostal Muscles (Continued) Slide 12 Diaphragm Sensory Innervation Slide 31 Intercostal Spaces and Intercostal Neurovascular Bundles Slide 13 Lung Surfaces Slide 32 Intercostal Neurovascular Bundle Slide 14 Root of the Lung Slide 33 Intercostal Nerve Block Slide 15 Slide 34 Internal Thoracic (Mammary) Artery Slide 16 Lung Lobes and Fissures Summary of of Intercostal Vasculature Slide 17 Contact Impressions on Mediastinal Lung Surface (Right) Slide 35 Collateral Circulation Through Internal Thoracic Artery Slide 18 Contact Impressions on Mediastinal Lung Surface (Left) Slide 36 Thoracic Cavity Subdivisions Slide 19 Surface Anatomy Correlates of Lung Lobes and Fissures Slide 37 Pleura and Endothoracic Fascia Slide 20 Lung Auscultation Slide 38 Thorax & Thoracic Cavity: Introduction The thorax refers to the region of the body between the neck https://3d4medic.al/enFsQOFf and the abdomen. The thoracic cavity is an irregularly shaped cylinder enclosed by the musculoskeletal walls of the thorax and the diaphragm. -

A Case of Cervical Rib and Neurovascular Compression in Roman Period
CASE REPORT Eur. J. Anat. 23(6): 453-458(2019) A case of cervical rib and neurovascular compression in Roman period Mauro Rubini1,2, Alessandro Gozzi1, Nunzia Libianchi1, M. Letizia Arancio3, Paola Zaio1 1S.A.B.A.P.-LAZ, Anthropological Service Ministry of Culture, Via degli Stabilimenti 5 00019 Tivoli, Rome, Italy, 2University of Foggia, Department of Archeology,3S.A.B.A.P.-RM-MET SUMMARY mammalians there are the supernumerary (or ac- cessory) ribs (SNR) that can be either lumbar ribs The possibility to study axial anomalies directly (LR) or cervical ribs (CR). The biological signifi- on a skeletal individual is not very frequent. One cance of SNR is very problematic and debated. well preserved skeletal individual from an Italian For example, in mouse models the spontaneous site dating to the late antique period (5th -4th cen- incidence of SNR is related to their species and turies CE) was studied. This individual shows ranges from <1% to >30%. Among humans, CRs some interesting skeletal changes in the vertebrae have a low frequency, about 0.2-1% (Guttentag et and ribs. A supernumerary rib was found. It is a al., 1999; Chang et al., 2013) and show variation in cervical rib connected to the 1st thoracic rib, pre- prevalence between different ethnic populations sumably with a fibrous bundle. The presence of (Brewin et al., 2009). The first to describe CR in cervical ribs can produce neurovascular compres- humans was Gruber, a German physician who sion of the brachial plexus and subclavian vessels. proposed a classification system (the Gruber Because of this, it is often a cause of thoracic out- scale) that is still utilized (Gruber, 1869; Chang et let syndrome (TOS). -

Thoracic Outlet Syndrome: First Rib Resection by Video-Thoracoscopy Using Two Ports
6 Surgical Technique Page 1 of 6 Thoracic outlet syndrome: first rib resection by video-thoracoscopy using two ports Ignacio Sastre, Manuel España, Roberto Ceballos, Mario Eduardo Francisco Bustos Thoracic Surgery Department, Hospital Privado Universitario de Cordoba, Cordoba, Argentina Correspondence to: Ignacio Sastre. Hospital Privado Universitario de Cordoba, Av Naciones Unidas 346, CP 5000, Cordoba, Argentina. Email: [email protected]. Abstract: Thoracic outlet syndrome (TOS) is defined as the set of signs and symptoms due to compression of the neural and vascular structures that cross the opening of the upper thorax. It can involve the brachial plexus, subclavian artery and vein. Treatment can be medical or surgical. The latter is indicated when conservative management fails and is based on decompression of the compromised structures by resection of the first rib, scalenotomy and resection of the cervical rib, if present. Open extrathoracic approaches have been used over time. Ohtsuka et al. described the first endoscopic approach for resection of the first rib and since then the videothoracoscopic technique has been optimized, finding several fully endoscopic approaches in the literature. We present our video-assisted surgical technique with 2 ports. We have been performing this technique for several years and each patient who will undergo surgery is evaluated in a multidisciplinary way, with neurologists, vascular doctors and orthopedists. The main advantages of this technique have been in the illumination and the magnified view from the video-camera. Visualization of the full length of the first rib and the neurovascular bundle is excellent and there is no need to retract any of the elements of the neurovascular bundle, therefore eliminating the risk of brachial plexus injury. -

Thoracic Outlet Syndrome
Thoracic Outlet Syndrome Introduction Thoracic Outlet Syndrome (TOS) is a condition affecting the shoulder, arm, and hand. This condition is a very frustrating problem - both for the patient and for the physician. It is extremely difficult to prove that the diagnosis of Thoracic Outlet Syndrome is correct, because there is no test that has a high degree of accuracy in showing the problem. Usually, the diagnosis is made after all other causes of the symptoms have been ruled out - a frustrating and slow process sometimes! Anatomy The nerves and blood vessels that run into the arm and hand start at the side of the neck. They exit from the side of the spine through small openings between each vertebra called foramen. As they leave the spine the nerves are referred to as nerve roots. The individual spinal nerve roots then begin to join together to form the nerves that will run into the arm and hand. The nerves travel between two muscles in the neck (the scalene muscles), over the top of the rib cage, under the collar bone (clavicle), through the arm pit (axilla) and down the arm to the hand. The area where the nerves and vessels leave the neck between the two scalene muscles and over the first rib is know as the Thoracic Outlet. Causes There are probably several causes of TOS. The common underlying cause of the syndrome is compression of the nerves and arteries of the arm in the Thoracic Outlet. Some people have an extra first rib or an old fracture of the clavicle, which limits the space for the vessels. -
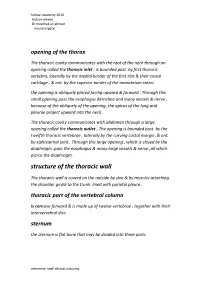
Structure of the Thoracic Wall
human anatomy 2016 lecture eleven Dr meethak ali ahmed neurosurgeon opening of the thorax The thoracic cavity communicates with the root of the neck through an opening called the thoracic inlet ; is bounded post. by first thoracic vertebra, laterally by the medial border of the first ribs & their costal cartilage , & ant. by the superior border of the manubrium sterni. the opening is obliquely placed facing upward & forward . Through this small opening pass the esophagus &trachea and many vessels & nerve . because of the obliquely of the opening ,the apices of the lung and pleurae project upward into the neck. The thoracic cavity communicates with abdomen through a large opening called the thoracic outlet . The opening is bounded post. by the twelfth thoracic vertebrae , laterally by the curving costal margin ,& ant. by xiphisternal joint . Through this large opening , which is closed by the diaphragm ,pass the esophagus & many large vessels & nerve ,all which pierce the diaphragm. structure of the thoracic wall The thoracic wall is coverd on the outside by skin & by muscles attaching the shoulder girdle to the trunk. lined with parietal pleura . thoracic part of the vertebral column is concave forward & is made up of twelve vertebrae , together with their intervertebral disc. sternum the sternum is flat bone that may be divided into three parts reference, snell clinical anatomy human anatomy 2016 lecture eleven Dr meethak ali ahmed neurosurgeon manubrium; is the upper part of the sternum ,& it articulates with the clavical & the first & upper part of the second costal cartilages on each side . it opposite the third and fourth thoracic vertebrae. -
Backpod-User-Guide-2018.Pdf
® USER GUIDE Designed and made in New Zealand Introduction and how to use the Backpod® 1 Introduction: Why you have neck or upper back pain - the iHunch 3 Instructions: How to use the Backpod® 6 Care of your Backpod® 7 Warnings and precautions Home care programme 9 One simple muscle stretch 10 Two simple strengthening exercises 12 Posture Home care programme Home care 13 Massage – two simple techniques Note from Steve August, B.A., Dip. Physio Thank you for buying the Backpod®. The views and recommendations contained in this user guide are my own. They are those of a New Zealand physiotherapist with 30 years’ experience. This amounts to over 40,000 patient treatments performed personally, plus innumerable courses, conferences, clinical discussions, reading, etc. Views on the strengths and limitations of other treatment and care approaches are fair comment from the viewpoint of a very experienced practitioner. Health Practitioner pages 15 Backpod® combined with manipulation and manual therapy from doctors, physiotherapists, osteopaths and chiropractors 17 Backpod® for straight or concave thoracic spines 18 Backpod® for scoliosis Backpod for Costochondritis, Tietze’s Syndrome, ‘slipping ribs’ and 19 costovertebral (posterior rib) joints 21 Backpod® for chronic asthma, bronchitis; rib pain in pregnancy Backpod® for ankylosing spondylitis, Scheuermann’s Osteochondritis and 23 Parkinson’s Disease 24 Backpod® for persisting pain after neck or thoracic surgery 25 Backpod® for sacroiliac mobilisations, and for coccydynia (tailbone pain) 27 Backpod® for T4 Syndrome and Thoracic Outlet Syndrome 28 Backpod® for prescribing doctors, pharmacists and acupuncturists 29 Backpod® combined with massage therapy 30 Backpod® with yoga, Feldenkrais Method, Alexander Technique and ergonomics 31 Backpod® for gymnasiums, Pilates and personal trainers Why you have neck or upper back pain - the iHunch Pain in the neck and upper back is a truly enormous See the iHUNCH page on the Backpod’s website problem. -

Thoracic Outlet Syndrome Either Modified Or Discarded
This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues. Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited. In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit: http://www.elsevier.com/copyright Author's personal copy SYNDROMES ago, after the concepts underlying each of its subgroups were Thoracic outlet syndrome either modified or discarded. In contrast the current classification proposed in 1984, is based on the structure(s) injured.2 Hani Abdul-Jabar True neurologic TOS Abbas Rashid This is a rare unilateral disorder that occurs predominantly in women in their late teens to mid 50s. It is almost invariably asso- Francis Lam ciated with a bony anomaly, such as a small cervical rib or an elongated C7 transverse process. A very taut fibrous band extends from the tip of the bony anomaly to the first thoracic rib which results in stretching of the proximal portion of the lower trunk of the brachial plexus or the distal portion of the T1 anterior Abstract primary ramus around the band. Symptoms are predominantly Thoracic Outlet Syndrome (TOS) is the constellation of symptoms motor, i.e. weakness of hand and forearm muscles with sub- caused by compression of neurovascular structures at the superior ap- stantial atrophy of the lateral thenar muscles (innervated by the erture of the thorax, properly the thoracic inlet! The diagnosis and treat- median nerve). -

Botulinum Toxin Treatment for Thoracic Outlet Syndrome Induced by Subclavius Muscle Hypertrophy
Case Report Botulinum Toxin Treatment for Thoracic Outlet Syndrome Induced by Subclavius Muscle Hypertrophy Francesco Cavallieri 1,2,* , Stefano Galletti 3, Valentina Fioravanti 1, Elisa Menozzi 4,5, Sara Contardi 4 and Franco Valzania 1 1 Neurology Unit, Neuromotor & Rehabilitation Department, Azienda USL-IRCCS di Reggio Emilia, 42123 Reggio Emilia, Italy; [email protected] (V.F.); [email protected] (F.V.) 2 Clinical and Experimental Medicine PhD Program, University of Modena and Reggio Emilia, 41121 Modena, Italy 3 Muscoloskeletal Interventional Sonographic Unit, Casa di Cura Toniolo, 40141 Bologna, Italy; [email protected] 4 Department of Neuroscience, S. Agostino-Estense Hospital and University of Modena and Reggio Emilia, 41126 Modena, Italy; [email protected] (E.M.); [email protected] (S.C.) 5 Department of Clinical and Movement Neurosciences, UCL Queen Square Institute of Neurology, London WC1N 3BG, UK * Correspondence: [email protected]; Tel.: +39-05-2229-5569 Abstract: Thoracic outlet syndrome (TOS) is frequently caused by bone abnormalities and congenital or acquired soft-tissue alterations. Among these, isolated Subclavius Muscle (SM) hypertrophy represents a rare condition that could lead to a reduction in costoclavicular space and brachial plexus compression. A 47-year-old forest ranger with a history of gun shooting during animal hunting and training sessions of skeet shooting for 20 years developed TOS due to ultrasonography-detected Citation: Cavallieri, F.; Galletti, S.; isolated SM hypertrophy, successfully treated with an ultrasound-guided Botulinum Toxin (BTX)-A Fioravanti, V.; Menozzi, E.; Contardi, injection. In our patient, ultrasonography of the brachial plexus has allowed SM hypertrophy to S.; Valzania, F.