Carrier Screening Disease & Gene List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Applications and Implications of Common and Founder Mutations in Indian Subpopulations
REVIEW OFFICIAL JOURNAL Clinical Applications and Implications of Common and Founder Mutations in Indian Subpopulations www.hgvs.org Arunkanth Ankala,1∗ † Parag M. Tamhankar,2 † C. Alexander Valencia,3,4 Krishna K. Rayam,5 Manisha M. Kumar,5 and Madhuri R. Hegde1 1Department of Human Genetics, Emory University School of Medicine, Atlanta, Georgia; 2ICMR Genetic Research Center, National Institute for Research in Reproductive Health, Mumbai, Maharashtra, India; 3Division of Human Genetics, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio; 4Department of Pediatrics, University of Cincinnati Medical School, Cincinnati, Ohio; 5Department of Biosciences, CMR Institute of Management Studies, Bangalore, Karnataka, India Communicated by Arupa Ganguly Received 24 October 2013; accepted revised manuscript 16 September 2014. Published online 27 November 2014 in Wiley Online Library (www.wiley.com/humanmutation). DOI: 10.1002/humu.22704 that include a lack of widespread awareness about genetic disorders in the general population and the scarcity of specialized medical ABSTRACT: South Asian Indians represent a sixth of the world’s population and are a racially, geographically, and professionals and affordable genetic tests. Seeking a molecular di- genetically diverse people. Their unique anthropological agnosis and understanding the risk estimates are critical to making structure, prevailing caste system, and ancient religious sound reproductive choices, especially in families with an affected practices have all impacted the genetic composition of most individual. Adding to this adversity is the absence of a properly func- of the current-day Indian population. With the evolving tioning social health care system and insufficient encouragement socio-religious and economic activities of the subsects and of individual health insurance by the government. -
PDF Document Created by Pdffiller
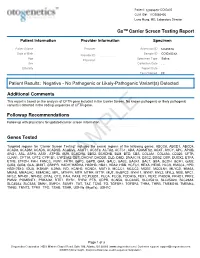
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Oxalate Loading Test: a Screening Test for Steatorrhoea
Gut: first published as 10.1136/gut.20.12.1089 on 1 December 1979. Downloaded from Gut, 1979, 20, 1089-1094 Oxalate loading test: a screening test for steatorrhoea D. S. RAMPTON', G. P. KASIDAS, G. ALAN ROSE, AND MARTIN SARNER2 From University College Hospital, London, St. Peter's Hospitals and Institute of Urology, London SUMMARY To investigate the possibility of measuring urinary oxalate output instead of faecal fat excretion as an outpatient screening test for steatorrhoea, we determined 24 hour urinary oxalate and five day faecal fat excretion before and during an oral load of sodium oxalate 600 mg daily (oxalate 4-44 mmol), in 32 patients with suspected malabsorption on a diet containing oxalate 30 mg (0-33 mmol), fat 50 g (180 mmol), and calcium 1 g (25 mmol). Nineteen patients proved to have steatorrhoea (mean faecal fat 62 mmol/24 h, range 19-186 mmol) of varying aetiologies. On the diet alone, urinary oxalate was raised in only nine of these patients (mean 0 25 mmol/24 h, range 0-08-059 mmol) (normal <0 20). By contrast, when the diet was supplemented with oral sodium oxalate, all 19 patients with steatorrhoea had hyperoxaluria (mean 0-91 mmol/24 h, range 046- 1P44 mmol) (normal <0-44). There was a significant positive linear relationship between urinary oxalate and faecal fat when the 32 patients were on the high oxalate intake (r=0*73, P <0.001), but not when they were on the low oxalate intake. Mean percentage absorption of orally administered oxalate was 58+09% (±1 SD) in normal subjects and 14-7+6-0% (P <0.002) in patients with steatorrhoea. -

Incidence of Inborn Errors of Metabolism by Expanded Newborn
Original Article Journal of Inborn Errors of Metabolism & Screening 2016, Volume 4: 1–8 Incidence of Inborn Errors of Metabolism ª The Author(s) 2016 DOI: 10.1177/2326409816669027 by Expanded Newborn Screening iem.sagepub.com in a Mexican Hospital Consuelo Cantu´-Reyna, MD1,2, Luis Manuel Zepeda, MD1,2, Rene´ Montemayor, MD3, Santiago Benavides, MD3, Hector´ Javier Gonza´lez, MD3, Mercedes Va´zquez-Cantu´,BS1,4, and Hector´ Cruz-Camino, BS1,5 Abstract Newborn screening for the detection of inborn errors of metabolism (IEM), endocrinopathies, hemoglobinopathies, and other disorders is a public health initiative aimed at identifying specific diseases in a timely manner. Mexico initiated newborn screening in 1973, but the national incidence of this group of diseases is unknown or uncertain due to the lack of large sample sizes of expanded newborn screening (ENS) programs and lack of related publications. The incidence of a specific group of IEM, endocrinopathies, hemoglobinopathies, and other disorders in newborns was obtained from a Mexican hospital. These newborns were part of a comprehensive ENS program at Ginequito (a private hospital in Mexico), from January 2012 to August 2014. The retrospective study included the examination of 10 000 newborns’ results obtained from the ENS program (comprising the possible detection of more than 50 screened disorders). The findings were the following: 34 newborns were confirmed with an IEM, endocrinopathies, hemoglobinopathies, or other disorders and 68 were identified as carriers. Consequently, the estimated global incidence for those disorders was 3.4 in 1000 newborns; and the carrier prevalence was 6.8 in 1000. Moreover, a 0.04% false-positive rate was unveiled as soon as diagnostic testing revealed negative results. -

Sphingolipid Metabolism Diseases ⁎ Thomas Kolter, Konrad Sandhoff
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1758 (2006) 2057–2079 www.elsevier.com/locate/bbamem Review Sphingolipid metabolism diseases ⁎ Thomas Kolter, Konrad Sandhoff Kekulé-Institut für Organische Chemie und Biochemie der Universität, Gerhard-Domagk-Str. 1, D-53121 Bonn, Germany Received 23 December 2005; received in revised form 26 April 2006; accepted 23 May 2006 Available online 14 June 2006 Abstract Human diseases caused by alterations in the metabolism of sphingolipids or glycosphingolipids are mainly disorders of the degradation of these compounds. The sphingolipidoses are a group of monogenic inherited diseases caused by defects in the system of lysosomal sphingolipid degradation, with subsequent accumulation of non-degradable storage material in one or more organs. Most sphingolipidoses are associated with high mortality. Both, the ratio of substrate influx into the lysosomes and the reduced degradative capacity can be addressed by therapeutic approaches. In addition to symptomatic treatments, the current strategies for restoration of the reduced substrate degradation within the lysosome are enzyme replacement therapy (ERT), cell-mediated therapy (CMT) including bone marrow transplantation (BMT) and cell-mediated “cross correction”, gene therapy, and enzyme-enhancement therapy with chemical chaperones. The reduction of substrate influx into the lysosomes can be achieved by substrate reduction therapy. Patients suffering from the attenuated form (type 1) of Gaucher disease and from Fabry disease have been successfully treated with ERT. © 2006 Elsevier B.V. All rights reserved. Keywords: Ceramide; Lysosomal storage disease; Saposin; Sphingolipidose Contents 1. Sphingolipid structure, function and biosynthesis ..........................................2058 1.1. -

Novel Association of Hypertrophic Cardiomyopathy, Sensorineural Deafness, and a Mutation in Unconventional Myosin VI (MYO6)
309 LETTER TO JMG J Med Genet: first published as 10.1136/jmg.2003.011973 on 1 April 2004. Downloaded from Novel association of hypertrophic cardiomyopathy, sensorineural deafness, and a mutation in unconventional myosin VI (MYO6) S A Mohiddin, Z M Ahmed, A J Griffith, D Tripodi, T B Friedman, L Fananapazir, R J Morell ............................................................................................................................... J Med Genet 2004;41:309–314. doi: 10.1136/jmg.2003.011973 amilial hypertrophic cardiomyopathy (FHC) is typically Key points characterised by left ventricular hypertrophy, diastolic Fdysfunction, and hypercontractility, and is often asso- ciated with disabling symptoms, arrhythmias, and sudden N Familial hypertrophic cardiomyopathy (FHC) is typi- death.1 FHC shows both non-allelic and allelic genetic cally confined to a cardiac phenotype and is caused by heterogeneity, and results from any one of more than 100 mutations in genes encoding sarcomeric proteins. mutations in genes encoding sarcomeric proteins.2 Identified Occasionally FHC may be one component of a genes include those encoding b myosin heavy chain, the hereditary multisystem disorder. myosin regulatory and essential light chains, myosin bind- N Sensorineural hearing loss is genetically heteroge- ing protein C, troponin I, troponin C, a cardiac actin, and neous. Mutations in the MYO6 gene, encoding 23 titin. The FHC phenotype is characterised by hypertrophy, unconventional myosin VI, have been found to cause myocyte disarray and fibrosis, and results from the dominant non-syndromic sensorineural hearing loss—that is, negative expression of one of these (mainly missense) sensorineural hearing loss in the absence of any other mutations. The resulting sarcomeric dysfunction leads related clinical features. ultimately, through mechanisms that remain obscure, to pathological left ventricular remodelling. -

Hereditary Galactokinase Deficiency J
Arch Dis Child: first published as 10.1136/adc.46.248.465 on 1 August 1971. Downloaded from Alrchives of Disease in Childhood, 1971, 46, 465. Hereditary Galactokinase Deficiency J. G. H. COOK, N. A. DON, and TREVOR P. MANN From the Royal Alexandra Hospital for Sick Children, Brighton, Sussex Cook, J. G. H., Don, N. A., and Mann, T. P. (1971). Archives of Disease in Childhood, 46, 465. Hereditary galactokinase deficiency. A baby with galactokinase deficiency, a recessive inborn error of galactose metabolism, is des- cribed. The case is exceptional in that there was no evidence of gypsy blood in the family concerned. The investigation of neonatal hyperbilirubinaemia led to the discovery of galactosuria. As noted by others, the paucity of presenting features makes early diagnosis difficult, and detection by biochemical screening seems desirable. Cataract formation, of early onset, appears to be the only severe persisting complication and may be due to the biosynthesis and accumulation of galactitol in the lens. Ophthalmic surgeons need to be aware of this enzyme defect, because with early diagnosis and dietary treatment these lens changes should be reversible. Galactokinase catalyses the conversion of galac- and galactose diabetes had been made in this tose to galactose-l-phosphate, the first of three patient (Fanconi, 1933). In adulthood he was steps in the pathway by which galactose is converted found to have glycosuria as well as galactosuria, and copyright. to glucose (Fig.). an unexpectedly high level of urinary galactitol was detected. He was of average intelligence, and his handicaps, apart from poor vision, appeared to be (1) Galactose Gackinase Galactose-I-phosphate due to neurofibromatosis. -

Neurodevelopmental Signatures of Narcotic and Neuropsychiatric Risk Factors in 3D Human-Derived Forebrain Organoids
Molecular Psychiatry www.nature.com/mp ARTICLE OPEN Neurodevelopmental signatures of narcotic and neuropsychiatric risk factors in 3D human-derived forebrain organoids 1 1 1 1 2 2 3 Michael Notaras , Aiman Lodhi , Estibaliz✉ Barrio-Alonso , Careen Foord , Tori Rodrick , Drew Jones , Haoyun Fang , David Greening 3,4 and Dilek Colak 1,5 © The Author(s) 2021 It is widely accepted that narcotic use during pregnancy and specific environmental factors (e.g., maternal immune activation and chronic stress) may increase risk of neuropsychiatric illness in offspring. However, little progress has been made in defining human- specific in utero neurodevelopmental pathology due to ethical and technical challenges associated with accessing human prenatal brain tissue. Here we utilized human induced pluripotent stem cells (hiPSCs) to generate reproducible organoids that recapitulate dorsal forebrain development including early corticogenesis. We systemically exposed organoid samples to chemically defined “enviromimetic” compounds to examine the developmental effects of various narcotic and neuropsychiatric-related risk factors within tissue of human origin. In tandem experiments conducted in parallel, we modeled exposure to opiates (μ-opioid agonist endomorphin), cannabinoids (WIN 55,212-2), alcohol (ethanol), smoking (nicotine), chronic stress (human cortisol), and maternal immune activation (human Interleukin-17a; IL17a). Human-derived dorsal forebrain organoids were consequently analyzed via an array of unbiased and high-throughput analytical approaches, including state-of-the-art TMT-16plex liquid chromatography/mass- spectrometry (LC/MS) proteomics, hybrid MS metabolomics, and flow cytometry panels to determine cell-cycle dynamics and rates of cell death. This pipeline subsequently revealed both common and unique proteome, reactome, and metabolome alterations as a consequence of enviromimetic modeling of narcotic use and neuropsychiatric-related risk factors in tissue of human origin. -

The Counsyl Foresight™ Carrier Screen
The Counsyl Foresight™ Carrier Screen 180 Kimball Way | South San Francisco, CA 94080 www.counsyl.com | [email protected] | (888) COUNSYL The Counsyl Foresight Carrier Screen - Disease Reference Book 11-beta-hydroxylase-deficient Congenital Adrenal Hyperplasia .................................................................................................................................................................................... 8 21-hydroxylase-deficient Congenital Adrenal Hyperplasia ...........................................................................................................................................................................................10 6-pyruvoyl-tetrahydropterin Synthase Deficiency ..........................................................................................................................................................................................................12 ABCC8-related Hyperinsulinism........................................................................................................................................................................................................................................ 14 Adenosine Deaminase Deficiency .................................................................................................................................................................................................................................... 16 Alpha Thalassemia............................................................................................................................................................................................................................................................. -

Clinical Genetics and the Hutterite Brethren
Clinical Genetics and the Hutterite Brethren: What have we learned in the new millenium? Or: A Micheil Innes MD FRCPC FCCMG Adapted from: Medical Genetics Grand Rounds January 2013 History and Population Hutterite Population Today >40 000 in AB, 30000 MB, ND, SD 1593-1770 1874-1879 25000 Transylvania 1256 migrated to American Prairies 20000 15000 World War I 10000 1565-1592 1770 - 1870 Migration to Canada Moravia5000 Ukraine 0 1500s 1520 1540 1550 1570 1580 1590 1610 1620 1680 1750 1760 1840 1860 1890 1900 1950 1975 1990 Tyrolean Alps Why Identify Genes in this Population? • Direct Benefits to • Benefit to Larger Patients/Families population – Non-invasive – Most of these disorders diagnostic test are not confined to this – Carrier test (*marriage population restrictions) – May allow for diagnosis – ?Prenatal testing of atypical cases – Enhanced understanding of – Expand basic science disease may facilitate and clinical knowledge management or treatment Initial Presentations May be Non-Specific Highlighting Importance of Careful Syndrome Delineation and Early Genetic Diagnosis • Hearing Loss – Autosomal recessive non-syndromic hearing loss (> 2loci) – Usher syndrome (> 2loci) – HDR syndrome • Cerebellar Ataxia – Joubert syndrome – DES syndrome – DCMA syndrome – CASS syndrome • Muscular Dystrophy/ High CK – LGMD2H – LGDM2I – AR EDMD – Myopathy with CPEO – Microcephaly with Chorea Genetic services and the Hutterites Religion/Culture • Has posed little barrier overall • Very accepting of medical care and technology • Although they believe that God plays a day to day role in guiding their lives, most couples accept genetic explanations for their children’s disorders • Some leuts and individual colonies are more conservative than others • Colony leader is clearly the Minister • Who speaks for the overall community when it comes to community wide issues? – e.g. -

Blueprint Genetics Primary Hyperoxaluria Panel
Primary Hyperoxaluria Panel Test code: KI0801 Is a 3 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of hyperoxaluria. About Primary Hyperoxaluria The primary hyperoxalurias are rare disorders of glyoxylate metabolism, which result in markedly increased endogenous oxalate synthesis by the liver. They are characterized by an excess of oxalate resulting in manifestations ranging from occasional renal stones, recurrent nephrolithiasis and nephrocalcinosis to end-stage renal disease (ESRD) and systemic oxalosis. Presenting ranges from the neonatal period to adulthood. Among disorders causing hyperoxaluria, the primary hyperoxalurias are the most severe, ultimately leading to ESRD and if untreated, death in most patients. Type I primary hyperoxaluria (PH1), is caused by deficient or absent activity of liver-specific peroxisomal alanine glyoxylate aminotransferase (AGT). In some patients with PH1 type disease, the enzyme is present but mistargeted to mitochondria where it is metabolically inactive. The severe infantile form is characterized by a failure to thrive, nephrocalcinosis with or without nephrolithiasis and early ESRD. Onset in childhood and adolescence is often characterized by recurrent urolithiasis (with or without nephrocalcinosis) and progressive renal failure. The late onset form is characterized by occasional renal stones with onset in adulthood, but acute renal failure caused by bilateral obstruction of the kidneys by oxalate stones may occur. Other manifestations include urinary tract infections, dysuria and hematuria. The ongoing systemic oxalosis also may lead to other clinical manifestations such as cardiac conduction defects, vascular calcification with distal gangrene, disturbed vision, specific brown colored retinal deposits, skin nodules, joint involvement and bone disease leading to fractures in long-term dialysis-dependent patients.