Alcohol Withdrawal Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Understanding Benzodiazephine Use, Abuse, and Detection
Siemens Healthcare Diagnostics, the leading clinical diagnostics company, is committed to providing clinicians with the vital information they need for the accurate diagnosis, treatment and monitoring of patients. Our comprehensive portfolio of performance-driven systems, unmatched menu offering and IT solutions, in conjunction with highly responsive service, is designed to streamline workflow, enhance operational efficiency and support improved patient care. Syva, EMIT, EMIT II, EMIT d.a.u., and all associated marks are trademarks of General Siemens Healthcare Diagnostics Inc. All Drugs other trademarks and brands are the Global Division property of their respective owners. of Abuse Siemens Healthcare Product availability may vary from Diagnostics Inc. country to country and is subject 1717 Deerfield Road to varying regulatory requirements. Deerfield, IL 60015-0778 Please contact your local USA representative for availability. www.siemens.com/diagnostics Siemens Global Headquarters Global Siemens Healthcare Headquarters Siemens AG Understanding Wittelsbacherplatz 2 Siemens AG 80333 Muenchen Healthcare Sector Germany Henkestrasse 127 Benzodiazephine Use, 91052 Erlangen Germany Abuse, and Detection Telephone: +49 9131 84 - 0 www.siemens.com/healthcare www.usa.siemens.com/diagnostics Answers for life. Order No. A91DX-0701526-UC1-4A00 | Printed in USA | © 2009 Siemens Healthcare Diagnostics Inc. Syva has been R1 R2 a leading developer N and manufacturer of AB R3 X N drugs-of-abuse tests R4 for more than 30 years. R2 C Now part of Siemens Healthcare ® Diagnostics, Syva boasts a long and Benzodiazepines have as their basic chemical structure successful track record in drugs-of-abuse a benzene ring fused to a seven-membered diazepine ring. testing, and leads the industry in the All important benzodiazepines contain a 5-aryl substituent ring (ring C) and a 1,4–diazepine ring. -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drugs of Abuse: Benzodiazepines
Drugs of Abuse: Benzodiazepines What are Benzodiazepines? Benzodiazepines are central nervous system depressants that produce sedation, induce sleep, relieve anxiety and muscle spasms, and prevent seizures. What is their origin? Benzodiazepines are only legally available through prescription. Many abusers maintain their drug supply by getting prescriptions from several doctors, forging prescriptions, or buying them illicitly. Alprazolam and diazepam are the two most frequently encountered benzodiazepines on the illicit market. Benzodiazepines are What are common street names? depressants legally available Common street names include Benzos and Downers. through prescription. Abuse is associated with What do they look like? adolescents and young The most common benzodiazepines are the prescription drugs ® ® ® ® ® adults who take the drug Valium , Xanax , Halcion , Ativan , and Klonopin . Tolerance can orally or crush it up and develop, although at variable rates and to different degrees. short it to get high. Shorter-acting benzodiazepines used to manage insomnia include estazolam (ProSom®), flurazepam (Dalmane®), temazepam (Restoril®), Benzodiazepines slow down and triazolam (Halcion®). Midazolam (Versed®), a short-acting the central nervous system. benzodiazepine, is utilized for sedation, anxiety, and amnesia in critical Overdose effects include care settings and prior to anesthesia. It is available in the United States shallow respiration, clammy as an injectable preparation and as a syrup (primarily for pediatric skin, dilated pupils, weak patients). and rapid pulse, coma, and possible death. Benzodiazepines with a longer duration of action are utilized to treat insomnia in patients with daytime anxiety. These benzodiazepines include alprazolam (Xanax®), chlordiazepoxide (Librium®), clorazepate (Tranxene®), diazepam (Valium®), halazepam (Paxipam®), lorzepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), and quazepam (Doral®). -

Benzodiazepines Addiction & Treatment
Benzodiazepines Addiction & Treatment Benzodiazepines are often used therapeutically to produce sedation, induce sleep, relieve anxiety and muscle spasms, and to prevent seizures. Benzodiazepines act as hypnotics in high doses, anxiolytics in moderate doses, and sedatives in low doses. Benzodiazepines effect the central nervous system functions and are classified as depressants. They are more commonly referred to as “benzos” or “benzies” and are ingestible in pill form or injected. Benzodiazepines can be found in many medications, including, but not limited to: Xanax (alprazolam), Valium (diazepam), Librium (chlordiazepoxide), Tranxene (clorazepate), Paxipam (Halazepam), Centrax (prazepam), Klonopin/Clonopin (Clonazepam), Serax (oxazepam), Restoril (temazepam), ProSom (estazolam), Dalmane (flurazepam) *Rohypnol (Flunitrazepam) is a benzodiazepine not manufactured or legally marketed in the United States; however it is often smuggled in by traffickers. This drug is often referred to as a “roofie” and is known as both a “party drug” and a “date rape” drug. It often is found to be popular among younger users. Effects of Benzodiazepines Benzodiazepine use can lead to amnesia, hostility, irritability, vivid or disturbing dreams, as well as tolerance and physical dependence. Use with alcohol or another depressant can lead to death, and often benzodiazepine abuse is particularly high among heroin and cocaine abusers. Lasting/Long-Term Effects Benzodiazepines target the emotional response system (limbic) of the brain, rather than the entire central nervous system. This leads to fewer long term effects than other drugs; however continued use can lead to physical and psychological dependence as well as addiction. Due to a tolerance developed to benzodiazepines, users must increase their doses in order to achieve the desired effects. -

Formulary Benzodiazepine Anti-Anxiety Agents
Alprazolam Shortage Recently, alprazolam has been in limited supply at both retail pharmacies and mail service facilities. Alprazolam is commercially manufactured as 0.25mg, 0.5mg, 1mg, and 2mg strength tablets. Retail pharmacies and mail order facilities may have alprazolam in stock but not necessarily all strengths. In response to the shortage of alprazolam, Xanax® (the branded product) has been temporarily added to the formulary. Xanax® XR, a recently approved sustained-release formulation of alprazolam, is not on the Highmark formulary. Although alprazolam quantities are available in limited supply, there are many other benzodiazepines available to treat anxiety. The following generic products in the table below are included on the Highmark formulary. Please consider these alternatives for patients who have difficulty obtaining Xanax or its generic. Formulary Benzodiazepine Anti-anxiety Agents Brandc Name Generic Name Approximate Dosage Range3 Equivalent (mg/day) Dosea, 1 b, 2 Short - Intermediate-acting benzodiazepines Xanax® alprazolam 0.5 mg 0.75 mg – 4 mg Ativan® lorazepam 1 mg 2 mg- 4 mg Serax® oxazepam 15 mg 30 mg – 120 mg b, 2Long-acting benzodiazepines Valium® diazepam 5 mg 4 mg – 40 mg Librium® chlordiazepoxide 10 mg 15 mg – 100 mg Tranxene® clorazepate 7.5 mg 15 mg – 60 mg a Elderly patients are treated with approximately one-half of dose listed b Based on effective half-life of parent drug and active metabolites c Brand products are non-formulary References 1. DiPiro, JT., et al. Pharmacotherapy: A Pathophysiologic Approach. 4th Edition, 1999; 1187 2. Shader RI, Greenblatt DJ. Use of Benzodiazepines in Anxiety Disorders. N Engl J Med 1993; 328: 1398-1405. -

Apo-Bromazepam
PRODUCT MONOGRAPH APO-BROMAZEPAM bromazepam 1.5 mg, 3 mg and 6 mg Tablets Anxiolytic - Sedative APOTEX INC. Date of Revision: 150 Signet Drive March 10, 2016 Toronto, Ontario M9L 1T9 Control No.: 192477 1 Table of Contents PART I: HEALTH PROFFESSIONAL INFORMATION .................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................. 3 INDICATIONS AND CLINICAL USE ................................................................................... 3 CONTRAINDICATIONS ........................................................................................................ 4 WARNINGS AND PRECAUTIONS ....................................................................................... 4 ADVERSE REACTIONS ......................................................................................................... 9 DRUG INTERACTIONS ....................................................................................................... 11 DOSAGE AND ADMINISTRATION ................................................................................... 12 OVERDOSAGE ...................................................................................................................... 14 ACTION AND CLINICAL PHARMACOLOGY ................................................................. 15 STORAGE AND STABILITY ............................................................................................... 16 DOSAGE FORMS, COMPOSITION AND PACKAGING ................................................. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0078604 A1 Kanios Et Al
US 20060078604A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0078604 A1 Kanios et al. (43) Pub. Date: Apr. 13, 2006 (54) TRANSDERMAL DRUG DELIVERY DEVICE Related U.S. Application Data INCLUDING AN OCCLUSIVE BACKING (60) Provisional application No. 60/616,861, filed on Oct. 8, 2004. (75) Inventors: David Kanios, Miami, FL (US); Juan A. Mantelle, Miami, FL (US); Viet Publication Classification Nguyen, Miami, FL (US) (51) Int. Cl. Correspondence Address: A 6LX 9/70 (2006.01) DCKSTEIN SHAPRO MORN & OSHINSKY (52) U.S. Cl. .............................................................. 424/449 LLP (57) ABSTRACT 2101 L Street, NW Washington, DC 20037 (US) A transdermal drug delivery system for the topical applica tion of one or more active agents contained in one or more (73) Assignee: Noven Pharmaceuticals, Inc. polymeric and/or adhesive carrier layers, proximate to a non-drug containing polymeric backing layer which can (21) Appl. No.: 11/245,180 control the delivery rate and profile of the transdermal drug delivery system by adjusting the moisture vapor transmis (22) Filed: Oct. 7, 2005 sion rate of the polymeric backing layer. Patent Application Publication Apr. 13, 2006 Sheet 1 of 2 US 2006/0078604 A1 Fis ZZZZZZZZZZZZZZZZZZZ :::::::::::::::::::::::::::::::: Patent Application Publication Apr. 13, 2006 Sheet 2 of 2 US 2006/0078604 A1 3. s s 3. a 3 : 8 g US 2006/0078604 A1 Apr. 13, 2006 TRANSIDERMAL DRUG DELVERY DEVICE 0008. In the “classic' reservoir-type device, the active INCLUDING AN OCCLUSIVE BACKING agent is typically dissolved or dispersed in a carrier to yield a non-finite carrier form, Such as, for example, a fluid or gel. -
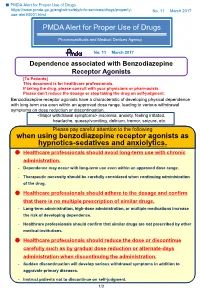
PMDA Alert for Proper Use of Drugs When Using Benzodiazepine
■ PMDA Alert for Proper Use of Drugs https://www.pmda.go.jp/english/safety/info-services/drugs/properly- No. 11 March 2017 use-alert/0001.html PMDA Alert for Proper Use of Drugs Pharmaceuticals and Medical Devices Agency No. 11 March 2017 Dependence associated with Benzodiazepine Receptor Agonists [To Patients] This document is for healthcare professionals. If taking the drug, please consult with your physicians or pharmacists. Please don’t reduce the dosage or stop taking the drug on self-judgment. Benzodiazepine receptor agonists have a characteristic of developing physical dependence with long-term use even within an approved dose range, leading to various withdrawal symptoms on dose reduction or discontinuation. <Major withdrawal symptoms> insomnia, anxiety, feeling irritated, headache, queasy/vomiting, delirium, tremor, seizure, etc. Please pay careful attention to the following when using benzodiazepine receptor agonists as hypnotics-sedatives and anxiolytics. Healthcare professionals should avoid long-term use with chronic administration. - Dependence may occur with long-term use even within an approved dose range. - Therapeutic necessity should be carefully considered when continuing administration of the drug. Healthcare professionals should adhere to the dosage and confirm that there is no multiple prescription of similar drugs. - Long-term administration, high-dose administration, or multiple medications increase the risk of developing dependence. - Healthcare professionals should confirm that similar drugs are not prescribed by other medical institutions. Healthcare professionals should reduce the dose or discontinue carefully such as by gradual dose reduction or alternate-days administration when discontinuing the administration. - Sudden discontinuation will develop serious withdrawal symptoms in addition to aggravate primary diseases. -

Chlordiazepoxide Vs Lorazepam
Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2017; 5(10D):4051-4056 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Chlordiazepoxide Vs Lorazepam- A Study of Comparison of Clinical Outcome and Cost of Alcohol Detoxification Suresh Daripelly1, Ashok ReddyK2, Nikil RavindranathT3 1SVS Medical College, Mahabubnagar 2Government Medical College, Mahabubnagar 3Institute of Mental Health, Hyderabad Abstract: Alcohol withdrawal is treated by cross tolerant benzodiazepines like Original Research Article Chlordiazepoxide, Diazepam and Lorazepam. The most frequently used Drugs Diazepam and Chlordiazepoxide have a long duration of action and are converted to *Corresponding author active metabolites in the liver, while Lorazepam is metabolized by conjugation, which Suresh Daripelly is less effected than the microsomal liver enzyme pathway in liver disease and it is short acting, with no active metabolites. The objective is to compare the clinical Article History outcome and cost in treating uncomplicated alcohol withdrawal state using Received: 11.10.2017 Chlordizepoxide and Lorazepam. This is a prospective, randomized, double blind, Accepted: 16.10.2017 interventional study. Sixty patients with alcohol dependence syndrome with moderate Published: 30.10.2017 withdrawal symptoms were allocated to receive either Chlordiazepoxide or Lorazepam, by means of a computer generated random sequence at a ratio of 1:1. DOI: Those with moderate to severe dependence on SADQ (20 and above) and moderate 10.21276/sjams.2017.5.10.48 withdrawal on CIWA-Ar (10-15) were included in the study Thirty patients each were started with lorazepam tablets 8 mg/day and chlordiazepoxide 100 mg/day. -
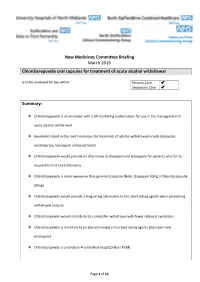
Chlordiazepoxide Oral Capsules for Treatment of Acute Alcohol Withdrawal Is to Be Reviewed for Use Within: Primary Care Secondary Care
New Medicines Committee Briefing March 2016 Chlordiazepoxide oral capsules for treatment of acute alcohol withdrawal is to be reviewed for use within: Primary Care Secondary Care Summary: Chlordiazepoxide is an anxiolytic with a UK marketing authorisation for use in the management of acute alcohol withdrawal. Anxiolytics listed in the Joint Formulary for treatment of alcohol withdrawal include diazepam, escitalopram, lorazepam and propranolol. Chlordiazepoxide would provide an alternative to diazepam and lorazepam for patients who fail to respond to first line treatments. Chlordiazepoxide is more expensive than generic diazepam (Note: Diazepam 10mg ≡ Chlordiazepoxide 25mg) Chlordiazepoxide would provide a long acting alternative to the short acting agents when preventing withdrawal seizures. Chlordiazepoxide would contribute to a smoother withdrawal with fewer rebound symptoms. Chlordiazepoxide is less likely to be abused compared to rapid acting agents (diazepam and lorazepam). Chlordiazepoxide is a schedule 4 controlled drug (CD Benz POM). Page 1 of 14 Formulary application Consultant submitting application: Ediela Iliescu (Consultant Substance Misuse Pschyiatrist) (North Staffordshire Combined Healthcare Trust) Clinical Director supporting application: Derrett Watts (Consultant addiction Psychiatrist) (North Staffordshire, Combined Healthcare Trust) The application is a request for chlordiazepoxide to be considered for inclusion in the North Staffordshire Joint Formulary for the treatment of alcohol withdrawal. In support, the applicant states that chlordiazepoxide is well suited for the treatment of alcohol withdrawal and can be used as an alternative to diazepam. Dr Iliescu states that it is difficult to quantify the exact number of patients that commence detoxification in the community. However, based on the figures provided by One Recovery in South Staffordshire (Stafford, Tamworth, Burton and Cannock), it is estimated that approximately 500 hundred patients per year commence treatment for alcohol detoxification in the community. -

Benzodiazepines (Nonsedative/ Hypnotics*)
Texas Vendor Drug Program Drug Use Criteria: Benzodiazepines (Nonsedative/ Hypnotics*) Publication History 1. Developed October 1993. 2. Revised March 2020; March 2018; May 2017; December 2014; March 2013; June 2011; January 2009; April 2003; December 2001; December 2000; December 1999; November 1998; November 1997; December 1996. Notes: Information on indications for use or diagnosis is assumed to be unavailable. All criteria may be applied retrospectively; prospective application is indicated with an asterisk [*]. The information contained is for the convenience of the public. The Texas Health and Human Services Commission is not responsible for any errors in transmission or any errors or omissions in the document. Medications listed in the tables and non-FDA approved indications included in these retrospective criteria are not indicative of Vendor Drug Program formulary coverage. Prepared by: Drug Information Service, UT Health San Antonio. The College of Pharmacy, The University of Texas at Austin. (*Sedative/hypnotic benzodiazepines are included in Sedative/Hypnotics criteria.) 1 1 Dosage 1.1 Adults Non-sedative/hypnotic benzodiazepines are FDA-approved for use in the outpatient setting to manage anxiety (alprazolam, chlordiazepoxide, clorazepate, oral diazepam, lorazepam, oxazepam), panic disorder (alprazolam, clonazepam), acute musculoskeletal (MS) conditions including spasticity (oral diazepam), seizures [clobazam (Lennox-Gastaut syndrome), clonazepam, clorazepate, nasal, oral and rectal diazepam], and acute alcohol withdrawal -
Identification and Quantification of 22 Benzodiazepines in Postmortem Fluids and Tissues Using UPLC/MS/MS
DOT/FAA/AM-18/1 Office of Aerospace Medicine Washington, DC 20591 Identification and Quantification of 22 Benzodiazepines in Postmortem Fluids and Tissues using UPLC/MS/MS Michael K. Angier Sunday R. Saenz Roxane M. Ritter Russell J. Lewis May 2018 Final Report NOTICE This document is disseminated under the sponsorship of the U.S. Department of Transportation in the interest of information exchange. The United States Government assumes no liability for the contents thereof. ___________ This publication and all Office of Aerospace Medicine technical reports are available in full-text from the Civil Aerospace Medical Institute’s publications website: http://www.faa.gov/go/oamtechreports Technical Report Documentation Page 1. Report No. 2. Government Accession No. 3. Recipient's Catalog No. DOT/FAA/AM-18/1 4. Title and Subtitle 5. Report Date Identification and Quantification of 22 Benzodiazepines in Postmortem May 2018 Fluids and Tissues using UPLC/MS/MS 6. Performing Organization Code 7. Author(s) 8. Performing Organization Report No. Angier MK, Saenz SR, Ritter RM, and Lewis RJ 9. Performing Organization Name and Address 10. Work Unit No. (TRAIS) FAA Civil Aerospace Medical Institute P.O. Box 25082 11. Contract or Grant No. Oklahoma City, OK 73125 12. Sponsoring Agency name and Address 13. Type of Report and Period Covered Office of Aerospace Medicine Federal Aviation Administration 800 Independence Ave., S.W. Washington, DC 20591 14. Sponsoring Agency Code 15. Supplemental Notes 16. Abstract Benzodiazepines, a class of drugs known to cause central nervous system depression, are widely prescribed for a variety of different medical conditions such as anxiety, insomnia, and as a preoperative sedative in conjunction with anesthesia.