2018 Cardiology Reimbursement Coding Fact Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cardiac Checklist Connecticare
Cardiac Checklist ConnectiCare Please be prepared to provide the applicable information from the following list when requesting prior authorization for a cardiac procedure managed by Magellan Healthcare1: 1. Medical chart notes – all notes from patient chart related to the requested procedure, including patient’s current cardiac status/symptoms, cardiac factors and indications. 2. Relevant patient information, including: a. Patient age, height, weight, and BMI. b. Family history of heart problems (including relationship to member, age at diagnosis, type of event, etc.). c. Medical history (e.g. diabetes, hypertension, stroke, arrhythmia, etc.). d. Cardiac risk factors. e. Previous cardiac treatments, surgeries or interventions (medications, CABG, PTCA, stent, heart valve surgery, pacemaker/defibrillator insertion, surgery for congenital heart disease, etc.). f. Problems with exercise capacity (orthopedic, pulmonary, or peripheral vascular disease; distance, heart rate). 3. Diagnostic or imaging reports from previous tests (exercise stress test, echocardiography, stress echocardiography, MPI, coronary angiography, etc.). a. For pacemaker or Implantable Cardioverter Defibrillator (ICD) requests, include EKG and/or telemetry strips showing bradycardia, EKG showing conduction abnormalities, EP study report, and/or tilt table test report, if applicable. b. For cardiac resynchronization therapy requests, include left ventricular function test report indicating LVEF, documentation of CHF symptoms and NYHA class and/or 12-Lead EKG showing QRS width, if applicable. c. For cardiac catheterization requests, include EKG results showing relevant changes, left ventricular function test reports, documentation of recent ejection fraction, etc. d. Cardiac catheterization requests also require the submission of digital images (e.g. DICOM files) from previous procedures. The digital image from a previous MPI, Stress Echocardiography, Heart PET or other cardiac catheterization is considered to be relevant and necessary clinical information. -

Correlation Between Echocardiography and Cardiac Catheterization for the Assessment of Pulmonary Hypertension in Pediatric Patients
Open Access Original Article DOI: 10.7759/cureus.5511 Correlation between Echocardiography and Cardiac Catheterization for the Assessment of Pulmonary Hypertension in Pediatric Patients Arshad Sohail 1 , Hussain B. Korejo 1 , Abdul Sattar Shaikh 2 , Aliya Ahsan 1 , Ram Chand 1 , Najma Patel 3 , Musa Karim 4 1. Pediatric Cardiology, National Institute of Cardiovascular Diseases, Karachi, PAK 2. Cardiology, National Institute of Cardiovascular Disease, Karachi, PAK 3. Paediatric Cardiology, National Institute of Cardiovascular Diseases, Karachi, PAK 4. Miscellaneous, National Institute of Cardiovascular Diseases, Karachi, PAK Corresponding author: Musa Karim, [email protected] Abstract Introduction Cardiac catheterization is widely considered the “gold standard” for the diagnosis of pulmonary hypertension. However, its routine use is limited due to its invasive nature. Therefore, the aim of this study was to evaluate the correlation between pulmonary artery pressures obtained by various parameters of transthoracic echocardiography and cardiac catheterization. Methods This study includes 50 consecutive patients with intracardiac shunt lesions diagnosed with severe pulmonary hypertension on echocardiography and admitted for cardiac catheterization at the National Institute of Cardiovascular Diseases (NICVD) in Karachi, Pakistan. Cardiac catheterization and transthoracic echocardiography were performed in all patients simultaneously and systolic (sPAP) and mean pulmonary artery pressure (mPAP) were assessed with both modalities. Correlations -

641 Iowa Administrative Code Chapter
IAC 12/9/15 Public Health[641] Ch 203, p.1 IOWA ADMINISTRATIVE CODE [641] CHAPTER 203 STANDARDS FOR CERTIFICATE OF NEED REVIEW [Prior to 7/29/87, Health Department[470] Ch 203] 641—203.1(135) Acute care bed need. Rescinded ARC 2297C, IAB 12/9/15, effective 1/13/16. 641—203.2(135) Cardiac catheterization and cardiovascular surgery standards. 203.2(1) Purpose and scope. a. These standards are measures of some of those criteria found in Iowa Code sections 135.64(1)“a” to “q,” and 135.64(3). Criteria which are measured by a standard are cited in parentheses following each standard. b. Certificate of need applications which are to be evaluated against these cardiac catheterization and cardiovascular surgery standards include: (1) Proposals to commence or expand capacity to perform cardiac catheterization. (2) Proposals to add new or replace cardiovascular surgery services. (3) Any other applications which relate to cardiac catheterization or cardiovascular surgery. 203.2(2) Definitions. a. Adult cardiac catheterization laboratory—a diagnostic facility exclusively for intracardiac or coronary artery catheterization on adults. b. Pediatric cardiac catheterization laboratory—the same as adult cardiac catheterization laboratory, except exclusively for children and infants. c. Cardiac catheterization— (1) Intracardiac—a diagnostic study of the heart, and pulmonary arteries, or both, in which a small catheter passes through a vein or artery in the neck, leg or arm and advances into the great vessels, the heart or the pulmonary arteries. Through this procedure one can measure pressure within the heart and in adjacent veins and arteries, collect blood samples for blood gas analysis and inject radiopaque material, visualize cardiac and vessel anatomy. -

ICD~10~PCS Complete Code Set Procedural Coding System Sample
ICD~10~PCS Complete Code Set Procedural Coding System Sample Table.of.Contents Preface....................................................................................00 Mouth and Throat ............................................................................. 00 Introducton...........................................................................00 Gastrointestinal System .................................................................. 00 Hepatobiliary System and Pancreas ........................................... 00 What is ICD-10-PCS? ........................................................................ 00 Endocrine System ............................................................................. 00 ICD-10-PCS Code Structure ........................................................... 00 Skin and Breast .................................................................................. 00 ICD-10-PCS Design ........................................................................... 00 Subcutaneous Tissue and Fascia ................................................. 00 ICD-10-PCS Additional Characteristics ...................................... 00 Muscles ................................................................................................. 00 ICD-10-PCS Applications ................................................................ 00 Tendons ................................................................................................ 00 Understandng.Root.Operatons..........................................00 -

Introduction
RIMS, IMPHAL ANNUAL REPORT 2014-15 INTRODUCTION 1. DESCRIPTION : The Regional Institute of Medical Sciences (RIMS), Imphal was established in the year 1972. It is an institution of regional importance catering to the needs of the North Eastern Region in the field of imparting undergraduate and post graduate medical education.The Institution brings together educational facilities for the training of personnel in all important branches of medical specialities including Dental and Nursing education in one place. The Institute is affiliated to the Manipur University, Canchipur, Imphal. 2. MANAGEMENT : The Institute was transferred to the Ministry of Health & Family Welfare, Government of India from North Eastern Council, Shillong (under Ministry of DoNER, Government of India) w.e.f. 1st April, 2007. Under the existing administrative set-up, the highest decision making body is the Board of Governors headed by the Union Minister of Health & Family Welfare as the President and the Director of the Institute as the Secretary. The Executive Council is responsible for the management of the Institute. The Secretary, Ministry of Health & Family Welfare, Government of India is the Chairman of the Executive Council while the head of the Institute remains as Secretary. Thus, the institute is managed at two levels, namely the Board of Governors and the Executive Council. A. Board of Governors : 1. Hon’ble Union Minister, - President Health & Family Welfare, Government of India. 2. Hon’ble Chief Minister, Manipur. - Vice-President 3. A Representative of the Planning Commission, - Member Government of India. 4. Health Ministers of the Beneficiary States - Member 5. Secretary, Ministry of Health & Family Welfare, - Member Government of India. -

Using Sound Advice—Intravascular Ultrasound As a Diagnostic Tool
Commentary Using sound advice—intravascular ultrasound as a diagnostic tool Yasir Parviz1, Khady N. Fall1, Ziad A. Ali1,2 1Center for Interventional Vascular Therapy, Division of Cardiology, Presbyterian Hospital and Columbia University, New York, USA; 2Cardiovascular Research Foundation, New York, USA Correspondence to: Ziad A. Ali. Center for Interventional Vascular Therapy, Division of Cardiology, Presbyterian Hospital and Columbia University, New York, NY, USA; Cardiovascular Research Foundation, New York, NY, USA. Email: [email protected]. Submitted Sep 06, 2016. Accepted for publication Sep 08, 2016. doi: 10.21037/jtd.2016.10.64 View this article at: http://dx.doi.org/10.21037/jtd.2016.10.64 Intravascular ultrasound (IVUS) uses varying-frequency (6.0% vs. 13.6%) (5). catheter-based transducers for assessment of blood vessel By extrapolation, IVUS may also have utility in the dimensions and morphology. Along with advances in the emergency setting for pathologies involving the LMCA field of interventional cardiology, IVUS technology has such as spontaneous or iatrogenic dissection. The incidence progressed in the last two decades. Dedicated training of spontaneous dissection in the LMCA has been reported centers in combination with enthusiasm from a new to be ~1% of all epicardial coronary arteries (6,7). Similar generation of cardiologists complemented by well- to aortic dissection, a spontaneous dissection of the established evidence for simplicity, safety and efficacy of LMCA leads to generation of a false lumen and intramural IVUS systems have led to increased routine use of this hematoma with or without intimal tear that may propagate imaging modality. Currently available catheters use sound retrograde into the aorta. -

Crucial Role of Carotid Ultrasound for the Rapid Diagnosis Of
m e d i c i n a 5 2 ( 2 0 1 6 ) 3 7 8 – 3 8 8 Available online at www.sciencedirect.com ScienceDirect journal homepage: http://www.elsevier.com/locate/medici Clinical Case Report Crucial role of carotid ultrasound for the rapid diagnosis of hyperacute aortic dissection complicated by cerebral infarction: A case report and literature review a a, b a Eglė Sukockienė , Kristina Laučkaitė *, Antanas Jankauskas , Dalia Mickevičienė , a a c a Giedrė Jurkevičienė , Antanas Vaitkus , Edgaras Stankevičius , Kęstutis Petrikonis , a Daiva Rastenytė a Department of Neurology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania b Department of Radiology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania c Institute of Physiology and Pharmacology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania a r t i c l e i n f o a b s t r a c t Article history: Aortic dissection is a life-threatening rare condition that may virtually present by any organ Received 24 January 2016 system dysfunction, the nervous system included. Acute cerebral infarction among multiple Received in revised form other neurological and non-neurological presentations is part of this acute aortic syndrome. 14 September 2016 Rapid and correct diagnosis is of extreme importance keeping in mind the possibility of Accepted 8 November 2016 thrombolytic treatment if a patient with a suspected ischemic stroke arrives to the Emergency Available online 19 November 2016 Department within a 4.5-h window after symptom onset. Systemic intravenous thrombolysis in the case of an acute brain infarction due to aortic dissection may lead to fatal outcomes. -

Acute Chest Pain-Suspected Aortic Dissection
Revised 2021 American College of Radiology ACR Appropriateness Criteria® Suspected Acute Aortic Syndrome Variant 1: Acute chest pain; suspected acute aortic syndrome. Procedure Appropriateness Category Relative Radiation Level US echocardiography transesophageal Usually Appropriate O Radiography chest Usually Appropriate ☢ MRA chest abdomen pelvis without and with Usually Appropriate IV contrast O MRA chest without and with IV contrast Usually Appropriate O CT chest with IV contrast Usually Appropriate ☢☢☢ CT chest without and with IV contrast Usually Appropriate ☢☢☢ CTA chest with IV contrast Usually Appropriate ☢☢☢ CTA chest abdomen pelvis with IV contrast Usually Appropriate ☢☢☢☢☢ US echocardiography transthoracic resting May Be Appropriate O Aortography chest May Be Appropriate ☢☢☢ MRA chest abdomen pelvis without IV May Be Appropriate contrast O MRA chest without IV contrast May Be Appropriate O MRI chest abdomen pelvis without IV May Be Appropriate contrast O CT chest without IV contrast May Be Appropriate ☢☢☢ CTA coronary arteries with IV contrast May Be Appropriate ☢☢☢ MRI chest abdomen pelvis without and with Usually Not Appropriate IV contrast O ACR Appropriateness Criteria® 1 Suspected Acute Aortic Syndrome SUSPECTED ACUTE AORTIC SYNDROME Expert Panel on Cardiac Imaging: Gregory A. Kicska, MD, PhDa; Lynne M. Hurwitz Koweek, MDb; Brian B. Ghoshhajra, MD, MBAc; Garth M. Beache, MDd; Richard K.J. Brown, MDe; Andrew M. Davis, MD, MPHf; Joe Y. Hsu, MDg; Faisal Khosa, MD, MBAh; Seth J. Kligerman, MDi; Diana Litmanovich, MDj; Bruce M. Lo, MD, RDMS, MBAk; Christopher D. Maroules, MDl; Nandini M. Meyersohn, MDm; Saurabh Rajpal, MDn; Todd C. Villines, MDo; Samuel Wann, MDp; Suhny Abbara, MD.q Summary of Literature Review Introduction/Background Acute aortic syndrome (AAS) includes the entities of acute aortic dissection (AD), intramural hematoma (IMH), and penetrating atherosclerotic ulcer (PAU). -
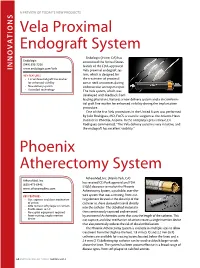
Vela Proximal Endograft System Phoenix Atherectomy System
A PREVIEW OF today’s NEW PRODUCTS ONS I Vela Proximal Endograft System Endologix (Irvine, CA) has Endologix announced the United States (949) 595-7200 launch of the FDA-approved INNOVAT www.endologix.com/Vela Vela proximal endograft sys- KEY FEATURES tem, which is designed for • Circumferential graft line marker the treatment of proximal for enhanced visibility aortic neck anatomies during • New delivery system endovascular aneurysm repair. • ActiveSeal technology The Vela system, which was developed with feedback from leading physicians, features a new delivery system and a circumferen- tial graft line marker for enhanced visibility during the implantation procedure. One of the first Vela procedures in the United States was performed by Julio Rodriguez, MD, FACS, a vascular surgeon at the Arizona Heart Institute in Phoenix, Arizona. In the company’s press release, Dr. Rodriguez commented, “The Vela delivery system is very intuitive, and the endograft has excellent visibility.” Phoenix Atherectomy System AtheroMed, Inc. (Menlo Park, CA) AtheroMed, Inc. has received CE Mark approval and FDA (650) 473-6846 510(k) clearance to market the Phoenix www.atheromedinc.com Atherectomy System, a pushable, over-the- KEY FEATURES wire system that uses a rotating, front-cut- • Cut, capture, and clear mechanism ting element located at the distal tip of the of action catheter to shave diseased material directly • Able to treat soft plaque or calcium • Profile down to 5 F into the catheter. The debulked material is • No capital equipment required then continuously captured and removed • Front-cutting, single insertion by an internal Archimedes screw that runs the length of the catheter. -

Medicare National Coverage Determinations Manual, Part 1
Medicare National Coverage Determinations Manual Chapter 1, Part 1 (Sections 10 – 80.12) Coverage Determinations Table of Contents (Rev. 10838, 06-08-21) Transmittals for Chapter 1, Part 1 Foreword - Purpose for National Coverage Determinations (NCD) Manual 10 - Anesthesia and Pain Management 10.1 - Use of Visual Tests Prior to and General Anesthesia During Cataract Surgery 10.2 - Transcutaneous Electrical Nerve Stimulation (TENS) for Acute Post- Operative Pain 10.3 - Inpatient Hospital Pain Rehabilitation Programs 10.4 - Outpatient Hospital Pain Rehabilitation Programs 10.5 - Autogenous Epidural Blood Graft 10.6 - Anesthesia in Cardiac Pacemaker Surgery 20 - Cardiovascular System 20.1 - Vertebral Artery Surgery 20.2 - Extracranial - Intracranial (EC-IC) Arterial Bypass Surgery 20.3 - Thoracic Duct Drainage (TDD) in Renal Transplants 20.4 – Implantable Cardioverter Defibrillators (ICDs) 20.5 - Extracorporeal Immunoadsorption (ECI) Using Protein A Columns 20.6 - Transmyocardial Revascularization (TMR) 20.7 - Percutaneous Transluminal Angioplasty (PTA) (Various Effective Dates Below) 20.8 - Cardiac Pacemakers (Various Effective Dates Below) 20.8.1 - Cardiac Pacemaker Evaluation Services 20.8.1.1 - Transtelephonic Monitoring of Cardiac Pacemakers 20.8.2 - Self-Contained Pacemaker Monitors 20.8.3 – Single Chamber and Dual Chamber Permanent Cardiac Pacemakers 20.8.4 Leadless Pacemakers 20.9 - Artificial Hearts And Related Devices – (Various Effective Dates Below) 20.9.1 - Ventricular Assist Devices (Various Effective Dates Below) 20.10 - Cardiac -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Computed Tomography Angiographic Assessment of Acute Chest Pain
SA-CME ARTICLE Computed Tomography Angiographic Assessment of Acute Chest Pain Matthew M. Miller, MD, PhD,* Carole A. Ridge, FFRRCSI,w and Diana E. Litmanovich, MDz Acute chest pain leads to 6 million Emergency Depart- Abstract: Acute chest pain is a leading cause of Emergency Depart- ment visits per year in the United States.1 Evaluation of acute ment visits. Computed tomography angiography plays a vital diag- chest pain often leads to a prolonged inpatient assessment, nostic role in such cases, but there are several common challenges with assessment duration often exceeding 12 hours. The associated with the imaging of acute chest pain, which, if unrecog- estimated cost of a negative inpatient chest pain assessment nized, can lead to an inconclusive or incorrect diagnosis. These 2,3 imaging challenges fall broadly into 3 categories: (1) image acquis- amounts to $8 billion per year in the United States. ition, (2) image interpretation (including physiological and pathologic The main challenge to diagnosis is the broad range of mimics), and (3) result communication. The aims of this review are to pathologies that can cause chest pain. Vascular causes describe and illustrate the most common challenges in the imaging of include pulmonary embolism (PE), traumatic and acute chest pain and to provide solutions that will facilitate accurate spontaneous aortic syndromes including aortic transection, diagnosis of the causes of acute chest pain in the emergency setting. dissection, intramural hematoma, and penetrating athero- sclerotic ulcer, aortitis, and coronary artery disease. The Key Words: acute chest pain, challenges, pulmonary angiography, latter will not be discussed in detail because of the com- aortography, computed tomography plexity and breadth of this topic alone.