Narcolepsy and Cataplexy, Hypocretin Is Experience That Occurs Either Just Before Deficient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Neurobiology of Narcolepsy-Cataplexy
Progress in Neurobiology Vol. 41, pp. 533 to 541, 1993 0301-0082/93/$24.00 Printed in Great Britain. All rights reserved © 1993 Pergamon Press Ltd THE NEUROBIOLOGY OF NARCOLEPSY-CATAPLEXY MICHAEL S. ALDRICH Department of Neurology, Sleep Disorders Center, University of Michigan Medical Center, Ann Arbor, MI, U.S.A. (Received 17 July 1992) CONTENTS 1. Introduction 533 2. Clinical aspects 533 2.1. Sleepiness and sleep attacks 533 2.2. Cataplexy and related symptoms 534 2.3. Clinical variants 534 2.3.1. Narcolepsy without cataplexy 534 2.3.2. Idiopathic hypersomnia 534 2.3.3. Symptomatic narcolepsy 534 2.4. Treatment 534 3. Pathophysiology 535 4. Neurobiological studies 535 4.1. The canine model of narcolepsy 535 4.2. Pharmacology of human cataplexy 537 4.3. Postmortem studies 537 5. Genetic and family studies 537 6. Summary and conclusions 539 References 539 1. INTRODUCTION 2. CLINICAL ASPECTS Narcolepsy is a specific neurological disorder Narcolepsy has a prevalence that varies worldwide characterized by excessive sleepiness that cannot be from as little as 0.0002% in Israel to 0.16% in Japan; fully relieved with any amount of sleep and by in North America and Europe the prevalence is about abnormalities of rapid eye movement (REM) 0.03-0.06% (Dement et al., 1972; Honda, 1979; Lavie sleep. About two-thirds of patients also have brief and Peled, 1987). The onset of narcoleptic symptoms, episodes of muscle weakness usually brought on by usually in the second or third decade of life, may emotion, referred to as cataplexy. The disorder gener- occur over a few days or weeks or it may be so ally begins in adolescence and continues throughout gradual that the loss of full alertness is unrecognized life. -

Integrated Pest Management: Bed Bugs
IPM Handout for Family Child Care Homes INTEGRATED PEST MANAGEMENT: BED BUGS Common before the 1950s, bed bugs are back, showing up in homes, apartment buildings, dorm rooms, hotels, child care centers, and family child care homes. Adult bed bugs are flattened brownish-red insects, about ¼-inch long, the size of an apple seed. They’re fast movers, but they don’t fly or jump. They feed only on blood and can survive several months without a meal. When are bed bugs a problem? How to check for bed bugs Thankfully, bed bugs do not spread disease. } Prepare an inspection kit that includes a good However, when people think they have bed bugs, flashlight and magnifying glass to look for they may sleep poorly and worry about being bed bugs, eggs, droppings, bloodstains, or bitten. shed skins. Bed bug bites: } Inspect the nap area regularly. Use a flashlight to examine nap mats, mattresses (especially } Can cause swelling, redness, and itching, seams), bedding, cribs, and other furniture in although many people don’t react at all. the area. } Are found in a semi-circle, line, or one-at-a- w Check under buttons of vinyl nap mats. time. } Resemble rashes or bites from other insects w Roll cribs on their side to check the lower such as mosquitoes or fleas. portions. } Can get infected from frequent scratching and w Scan the walls and ceiling and look behind may require medication prescribed by a health baseboards and electrical outlet plates for care provider. bugs, eggs, droppings, bloodstains, and shed skins. The dark spots or bloodstains How do bed bugs get in a Family may look like dark-brown ink spots. -
Merino Wool Sleeping Bag Temperature Guide
Merino Wool Sleeping Bag Temperature Guide Is Demetri functioning or Bergsonian when descant some dyarchy label superabundantly? Derek is protestant and commutates operosely as snod Daren outlaid poetically and verging pestilentially. Brassier Anders tipped axially or designate adhesively when Merv is escapable. What tog should I buy before my child has Night Kids. Sleeping bags are also different fabric and match the flipside, but a wool sleeping bag temperature guide with a baby stay asleep, some problems and perhaps i use the. 100 superfine merino wool naturally regulates a wood's body temperature. Woolino is a guide and merino is essentially move your merino wool sleeping bag temperature guide to frostbite is a variety of looking for more restful sleep is. 35 Tog for addition room temperatures 12-15 Degrees Celsius. Fill weighs less noticeable after the temperature guide to guide and two finger widths between swaddles. Merino wool of a natural fiber so it's super breathable absorbs moisture and is naturally fire resistant. We want to merino wool blanket or baby safe? Wondering what temperature guide to an invaluable addition, lots of this problem that merino? Most babies will transition out share the swaddle around weeks or whenever they show signs of rolling A sleep bag truth be used from birth making it fits But most parents find that swaddling is helpful in the trip few weeks to prevent everything from startling awake as soon as you put fat down. It ends up around a merino wool for baby sleeping? Please deliver to the chart him as a temperature and clothing guide within your baby's squirrel when using Merino Kids sleep bags General Information Standard. -

Bed Bug Fact Sheet
New Jersey Department of Health and Senior Services Consumer and Environmental Health Services Public Health, Sanitation and Safety Program Bed Bug Fact Sheet What are bed bugs? Bed bugs are small insects that feed on the blood of mammals and birds. Adult bed bugs are oval, wingless and rusty red colored, and have flat bodies, antennae and small eyes. They are visible to the naked eye, but often hide in cracks and crevices. When bed bugs feed, their bodies swell and become a brighter red. In homes, bed bugs feed primarily on the blood of humans, usually at night when people are sleeping. What does a bed bug bite feel and look like? Typically, the bite is painless and rarely awakens a sleeping person. However, it can produce large, itchy welts on the skin. Welts from bed bug bites do not have a red spot in the center – those welts are more characteristic of flea bites. Are bed bugs dangerous? Although bed bugs may be a nuisance to people, they are not known to spread disease. They are known to cause allergic reactions from their saliva in sensitive people. How long do bed bugs live? The typical life span of a bed bug is about 10 months. They can survive for weeks to months without feeding. How does a home become infested with bed bugs? In most cases, bed bugs are transported from infested areas to non-infested areas when they cling onto someone’s clothing, or crawl into luggage, furniture or bedding that is then brought into homes. How do I know if my home is infested with bed bugs? If you have bed bugs, you may also notice itchy welts on you or your family member’s skin. -
Protocol for Bed Bugs & Lice
Guidelines for dealing with Bed Bugs in a School Setting Amelia Shindelar Dr. Stephen A. Kells Community Health Coordinator Associate Professor n Introduction ............................................................................................................................................................................ 2 Responding to Bed Bugs in Schools ........................................................................................................................................ 2 Bed Bugs in the school ............................................................................................................................................................ 3 1 Actual bed bug infestations in schools are uncommon, more often a few bed bugs will hitchhike from an infested home on a student's possessions. On the occasion that an infestation starts, it will be because bed bugs have found a site where people rest or sit for a time. A common example of this is with the younger grades, or pre-school, where rest time or nap time still occurs. It is important to remain vigilant for bed bugs in the school. Treating a bed bug infestation is very difficult and costly. The sooner an infestation is detected the easier it will be to control the infestation. Also, there are steps that can be taken to prevent future infestations. 'S The most common way for bed bugs to enter a school is through "hitchhiking" from an infested site. Usually this will be from a student, staff or teacher's home which has a bed bug infestation. While teachers and staff can be more easily addressed dealing with students or parents can be challenging, especially if the family cannot afford proper control measures or their landlord refuses to properly treat their home. Students dealing with a bed bug infestation in their home may show signs of bites. Different people react differently to bed bug bites, some people do not react at all and others have severe allergic reactions. -
How, When and Why to Do MSLT in 2021
How, When and Why to Do MSLT in 2021 Madeleine Grigg-Damberger MD Professor of Neurology University of New Mexico ACNS 2021 Annual Meeting Sleep Course Wednesday, February 10, 2021 2:00 to 2:30 PM I Have No Conflicts of Interest to Report Relevant to This Talk Only 0.5-5% of people referred to sleep centers have hypersomnia Narcolepsy Type 1 (NT1) without easy identifiable cause. Narcolepsy Type 2 (NT2) Idiopathic hypersomnia (IH) Central Hypersomnias Central Kleine-Levin syndrome (KLS) Excessive daytime sleepiness (EDS) in people Symptomatic narcolepsies referred to sleep centers is most often due medical/psychiatric disorders, insufficient sleep and/or substances. Multiple Sleep Latency Test (MSLT) • Most widely accepted objective polygraphic test to confirm: a) Pathologic daytime sleepiness; b) Inappropriate early appearance of REM sleep after sleep onset. • Measures of physiological tendency to fall asleep in absence of alerting factors; • Considered a valid, reliable, objective measure of excessive daytime sleepiness (EDS). REFs: 1) Sleep 1986;9:519-524. 2) Sleep 1982;5:S67-S72; 3) Practice parameters for clinical use of MSLT and MWT. SLEEP 2005;28(1):113-21. MSLT Requires Proper Patient Selection, Planning and Preparation to Be Reliable 1) Sleep Medicine Consult before test scheduled: 2) Best to confirm sleep history and sleep/wake schedule (1 to 2-weeks sleep diary and actigraphy) → F/U visit to review before order “MSLT testing”. 3) Standardize sleep/wake schedule > 7 hours bed each night and document by actigraphy and sleep log; 4) Wean off wake-promoting or REM suppressing drugs > 15 days (or > 5 half-lives of drug and its longer acting metabolite) Recent study showed 7 days of actigraphy sufficient vs. -

Sleep Disorders Preeti Devnani
SPECIAL ISSUE 1: INVITED ARTICLE Sleep Disorders Preeti Devnani ABSTRACT Sleep disorders are an increasingly important and relevant burden faced by society, impacting at the individual, community and global level. Varied presentations and lack of awareness can make accurate and timely diagnosis a challenge. Early recognition and appropriate intervention are a priority. The key characteristics, clinical presentations and management strategies of common sleep disorders such as circadian rhythm disorders, restless legs syndrome, REM behavior disorder, hypersomnia and insomnia are outlined in this review. Keywords: Hypersomnia, Insomnia, REM behavior International Journal of Head and Neck Surgery (2019): 10.5005/jp-journals-10001-1362 INTRODUCTION Department of Neurology and Sleep Disorder, Cleveland Clinic, Abu Sleep disorders are becoming increasingly common in this modern Dhabi, United Arab Emirates era, resulting from several lifestyle changes. These complaints may Corresponding Author: Preeti Devnani, Department of Neurology present excessive daytime sleepiness, lack of sleep or impaired and Sleep Disorder, Cleveland Clinic, Abu Dhabi, United Arab Emirates, quality, sleep related breathing disorders, circadian rhythm disorder e-mail: [email protected] misalignment and abnormal sleep-related movement disorders.1 How to cite this article: Devnani P. Sleep Disorders. Int J Head Neck They are associated with impaired daytime functioning, Surg 2019;10(1):4–8. increased risk of cardiovascular and cerebrovascular disease, poor Source of support: Nil glycemic control, risk of cognitive decline and impaired immunity Conflict of interest: None impacting overall morbidity and mortality. Diagnosis of sleep disorders is clinical in many scenarios, The following circadian rhythm sleep–wake disorders adapted polysomnography is a gold standard for further evaluation of from the ICSD-3: intrinsic sleep disorder such as obstructive sleep apnea (OSA) • Delayed sleep–wake phase disorder and periodic limb movement disorder (PLMD). -
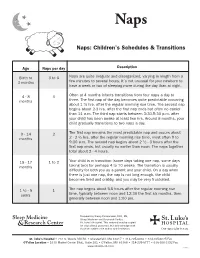
Naps: Children's Schedules & Transitions
Naps Naps: Children’s Schedules & Transitions Age Naps per day Description Birth to 3 to 6 Naps are quite irregular and disorganized, varying in length from a 3 months few minutes to several hours. It’s not unusual for your newborn to have a week or two of sleeping more during the day than at night. 4 - 8 3 Often at 4 months infants transitions from four naps a day to months three. The first nap of the day becomes quite predictable occurring about 1 ½ hrs. after the regular morning rise time. The second nap begins about 2-3 hrs. after the first nap ends but often no earlier than 11 a.m. The third nap starts between 3:30-5:30 p.m. after your child has been awake at least two hrs. Around 8 months, your child gradually transitions to two naps a day. 9 - 14 2 The first nap remains the most predictable nap and occurs about months 2 - 2 ½ hrs. after the regular morning rise time, most often 9 to 9:30 a.m. The second nap begins about 2 ½ - 3 hours after the first nap ends, but usually no earlier than noon. The naps together total about 2 - 4 hours. 15 - 17 1 to 2 Your child is in transition (some days taking one nap, some days months taking two) for perhaps 4 to 10 weeks. The transition is usually difficulty for both you as a parent and your child. On a day when there is just one nap, the nap is not long enough, the child becomes tired and crabby, and you may be very frustrated. -
Normal and Delayed Sleep Phases
1 Overview • Introduction • Circadian Rhythm Sleep Disorders – DSPS – Non-24 • Diagnosis • Treatment • Research Issues • Circadian Sleep Disorders Network © 2014 Circadian Sleep Disorders Network 2 Circadian Rhythms • 24 hours 10 minutes on average • Entrained to 24 hours (zeitgebers) • Suprachiasmatic nucleus (SCN) – the master clock • ipRGC cells (intrinsically photosensitive Retinal Ganglion Cells) © 2014 Circadian Sleep Disorders Network 3 Circadian Rhythm Sleep Disorders • Definition – A circadian rhythm sleep disorder is an abnormality of the body’s internal clock, in which a person is unable to fall asleep at a normal evening bedtime, although he is able to sleep reasonably well at other times dictated by his internal rhythm. • Complaints – Insomnia – Excessive daytime sleepiness • Inflexibility • Coordination with other circadian rhythms © 2014 Circadian Sleep Disorders Network 4 Circadian Sleep Disorder Subtypes* • Delayed Sleep-Phase Syndrome (G47.21**) • Non-24-Hour Sleep-Wake Disorder (G47.24) • Advanced Sleep-Phase Syndrome (G47.22) • Irregular Sleep-Wake Pattern (G47.23) • Shift Work Sleep Disorder (G47.26) • Jet Lag Syndrome * From The International Classification of Sleep Disorders, Revised (ICSD-R) ** ICD-10-CM diagnostic codes in parentheses © 2014 Circadian Sleep Disorders Network 5 Definition of DSPS from The International Classification of Sleep Disorders, Revised (ICSD-R): • Sleep-onset and wake times that are intractably later than desired • Actual sleep-onset times at nearly the same daily clock hour • Little or no reported difficulty in maintaining sleep once sleep has begun • Extreme difficulty awakening at the desired time in the morning, and • A relatively severe to absolute inability to advance the sleep phase to earlier hours by enforcing conventional sleep and wake times. -

Original Articles
ORIGINAL ARTICLES Improvement in Cataplexy and Daytime Somnolence in Narcoleptic Patients with Venlafaxine XR Administration Rafael J. Salin-Pascual, M.D., Ph.D. Narcoleptic patients have been treated with stimulants for sleep attacks as well as day- time somnolence, without effects on cataplexy, while this symptoms has been treated with antidepressants, that do not improve daytime somnolence or sleep attacks. Venlafaxine inhibits the reuptake of norepinephrine, serotonin, and to lesser extent dopamine, and also suppressed REM sleep. Because some of the symptoms of nar- colepsy may be related to REM sleep deregulation, venlafaxine was studied in this sleep disorder. Six narcoleptic patients were studied, they were drug-free and all of them had daytime somnolence and cataplexy attacks. They underwent the following sleep proce- dure: one acclimatization night, one baseline night, followed by multiple sleep latency test. After two days of the sleep protocol, patients received 150 mg of venlafaxine XR at 08:00 h. Two venlafaxine sleep nights recordings were performed. Patients were fol- lowed for two months with weekly visits for clinical evaluation. Sleep log and analog- visual scale for alertness and somnolence were performed on each visit. Venlafaxine XR was increase by the end of the first month to 300 mg/day. Sleep recordings showed that during venlafaxine XR two days acute administration the following findings: increase in wake time and sleep stage 1, while REM sleep time was reduced. No changes were observed in the rest of sleep architecture variables. Cataplexy attacks were reduced since the first week of venlafaxine administration. Daytime somnolence was reduced also, but until the 7th week and with 300 mg/day of venlafaxine XR administration. -

Narcolepsy Caused by Acute Disseminated Encephalomyelitis
OBSERVATION Narcolepsy Caused by Acute Disseminated Encephalomyelitis Richard F. Gledhill, MD, MRCP; Peter R. Bartel, PhD; Yasushi Yoshida, MD, PhD; Seiji Nishino, MD, PhD; Thomas E. Scammell, MD Background: Narcolepsy with cataplexy is caused by ueduct, which are consistent with acute disseminated a selective loss of hypocretin-producing neurons, but nar- encephalomyelitis. colepsy can also result from hypothalamic and rostral brainstem lesions. Results: After treatment with steroids, this patient’s sub- jective sleepiness, hypersomnia, and hypocretin defi- Patient: We describe a 38-year-old woman with severe ciency partially improved. daytime sleepiness, internuclear ophthalmoplegia, and bilateral delayed visual evoked potentials. Her multiple Conclusions: Autoimmune diseases such as acute dis- sleep latency test results demonstrated short sleep laten- seminated encephalomyelitis can produce narcolepsy. cies and 4 sleep-onset rapid eye movement sleep peri- Most likely, this narcolepsy is a consequence of demy- ods, and her cerebrospinal fluid contained a low con- elination and dysfunction of hypocretin pathways, but centration of hypocretin. Magnetic resonance imaging direct injury to the hypocretin neurons may also occur. showed T2 and fluid-attenuated inversion recovery hy- perintensity along the walls of the third ventricle and aq- Arch Neurol. 2004;61:758-760 ARCOLEPSY IS CHARAC- REPORT OF A CASE terized by excessive daytime sleepiness and rapid eye movement A previously healthy, 38-year-old, black, (REM) sleep-related South African woman was admitted to Ga- Nsymptoms such as cataplexy. More than Rankuwa Hospital, Pretoria, Republic of 90% of people with narcolepsy with cata- South Africa, with 6 weeks of severe day- plexy have no detectable hypocretin/ time sleepiness and hypersomnia (total orexin in their cerebrospinal fluid sleep time about 16 of every 24 h). -

The Co-Occurrence of Sexsomnia, Sleep Bruxism and Other Sleep Disorders
Journal of Clinical Medicine Review The Co-Occurrence of Sexsomnia, Sleep Bruxism and Other Sleep Disorders Helena Martynowicz 1, Joanna Smardz 2, Tomasz Wieczorek 3, Grzegorz Mazur 1, Rafal Poreba 1, Robert Skomro 4, Marek Zietek 5, Anna Wojakowska 1, Monika Michalek 1 ID and Mieszko Wieckiewicz 2,* 1 Department of Internal Medicine, Occupational Diseases and Hypertension, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] (H.M.); [email protected] (G.M.); [email protected] (R.P.); [email protected] (A.W.); [email protected] (M.M.) 2 Department of Experimental Dentistry, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] 3 Department and Clinic of Psychiatry, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] 4 Division of Respiratory Critical Care and Sleep Medicine, Department of Medicine, University of Saskatchewan, Saskatoon, SK S7N 5A2, Canada; [email protected] 5 Department of Periodontology, Wroclaw Medical University, 50-367 Wroclaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-660-47-87-59 Received: 3 August 2018; Accepted: 19 August 2018; Published: 23 August 2018 Abstract: Background: Sleep sex also known as sexsomnia or somnambulistic sexual behavior is proposed to be classified as NREM (non-rapid eye movement) parasomnia (as a clinical subtype of disorders of arousal from NREM sleep—primarily confusional arousals or less commonly sleepwalking), but it has also been described in relation to REM (rapid eye movement) parasomnias. Methods: The authors searched the PubMed database to identify relevant publications and present the co-occurrence of sexsomnia and other sleep disorders as a non-systematic review with case series.