Adverse Drug Reactions in Norway: a Systematic Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Conclusions and Recommendations from the Thirteenth Meeting of the WHO Advisory Committee on Safety of Medicinal Products (ACS
Conclusions and Recommendations from the Thirteenth Meeting of the WHO Advisory Committee on Safety of Medicinal Products (ACSoMP) Geneva, Switzerland 21 - 22 June 2016 The WHO Advisory Committee on Safety of Medicinal Products (ACSoMP) has been constituted to provide advice on pharmacovigilance (PV) policy and issues related to the safety and effectiveness of medicinal products. The conclusions and recommendations from the Tenth meeting of ACSoMP are presented below. Pharmacovigilance (PV) Priorities for World Health Organization (WHO): - Increasing access to essential, quality, safe and affordable medical products is a leadership priority for WHO. The ongoing WHO-reform process is to ensure that the organization is more effective, efficient, responsive, objective, transparent and accountable to its partners and stakeholders. The scope of the Safety and Vigilance (SAV) team within WHO includes: advocacy for safety and vigilance activities, establishing and consolidating partnerships for implementing and advancing the safety and safe use of medical products, strengthening infrastructure, active surveillance and training in pharmacovigilance (PV), and supporting the use of effective tools and systems for monitoring medical products of significant public health importance. - The 2016-2017 priorities for SAV/Medicines Safety are to focus on a few countries, to build capacity and support them through the full cycle of PV activities, from collecting PV data and information, to making regulatory decisions and therapeutic choices based on the collected information. The strategy would be to assess and to improve the quantitative and qualitative aspects of PV activities and outcomes in these countries. The long-term objective is to build comprehensive, sustainable, results-driven PV systems that improve our knowledge, power our decisions and promote the safe use of medicines. -

Medicinal Products and Medical Devices in Clinical Trials Conduct and Disclosure
Medicinal products and medical devices in clinical trials condduct and disclosure – and ndever the twain shall meet! Raquel Billiones 1 and Kathy B. Thomas 2 Despite some fundamental differences, 1 Takeda Pharmaceuticals, Zurich, Abstract similarities and overlaps in the requirements Switzerland “Medicinal products and medical devices are and details between the CTR and MDR are 2 Medical & Scientific Writing & Publication different species…they live in parallel evident. There is also a clear aim for the Services, Meersburg, Germany universes” according to a medical device electronic databases, as described in the two expert. But is it really so? This article regulations, to be interoperable. This high - challenges that notion by comparing the level comparison of the CTR and MDR Correspondence to: Clinical Trial Regulation EU No. 536/2014 shows that while the requirements of the two Raquel Billiones (CTR) and the EU Medical Device regulations have been aligned and are very [email protected] Regulation 2017/745 (MDR) in the context similar, their impact on the respective of clinical studies and public disclosure. industries is quite different. Two parallel universes years, we already switch between these universes pharmaceutical industry. The major changes “WARNING : Medicinal products and medical and firmly believe that linking these two is not were the centralised clinical trial application, the devices are different species. They live in parallel only feasible but also profitable, as other increased disclosure requirements, and the universes. They may appear similar (“medicinal colleagues can also attest. 2 Nevertheless, the setting up of a new EU portal and database (to products”), but they are not. -

Reporting Adverse Drug Reactions a Guide for Healthcare Professionals
BMA Board of Science Reporting adverse drug reactions A guide for healthcare professionals May 2006 improving health BMA Board of Science Reporting adverse drug reactions A guide for healthcare professionals May 2006 Reporting adverse drug reactions: A guide for healthcare professionals i BMA Board of Science Editorial board A publication from BMA Science & Education department and the BMA Board of Science Chair, Board of Science Professor Sir Charles George Director of Professional Activities Professor Vivienne Nathanson Head of Science & Education Dr Caroline Seddon Project manager Nicky Jayesinghe Research and writing Gemma Jackson Editorial secretariat EeMun Chen Nicola Fookes Darshna Gohil Emily Hoy Acknowledgements The association is very grateful for the help provided by the BMA committees and many outside experts and organisations. We would particularly like to thank: • Professor Munir Pirmohamed, Professor of Clinical Pharmacology and Director of CSM Mersey. • Dr June Raine, Director of the MHRA Post Licensing Division. • Professor Alison Blenkinsopp, Professor of the Practice of Pharmacy and member of the Committee on Safety of Medicines Patient Reporting of Adverse Drug Reactions Working Group. • Dr Patricia Wilkie, lay member of the Committee on Safety of Medicines and Chair of the Committee on Safety of Medicines Patient Reporting of Adverse Drug Reactions Working Group. • Ms Barbara Wood, Chair, BMA patient liaison group and member of the Committee on Safety of Medicines Patient Reporting of Adverse Drug Reactions Working Group. British Library Cataloguing-in-Publication Data. A catalogue record for this book is available from the British Library. ISBN: 1 905545 07 X Cover photograph: Getty Images © British Medical Association 2006 all rights reserved. -

Eudravigilance Medicines Safety Database: Publicly Accessible Data for Research and Public Health Protection
Drug Saf https://doi.org/10.1007/s40264-018-0647-1 SPECIAL ARTICLE EudraVigilance Medicines Safety Database: Publicly Accessible Data for Research and Public Health Protection 1 1 1 2 Rodrigo Postigo • Sabine Brosch • Jim Slattery • Anja van Haren • 3 1 1 1 Jean-Michel Dogne´ • Xavier Kurz • Gianmario Candore • Francois Domergue • Peter Arlett1 Ó The Author(s) 2018. This article is an open access publication Abstract The analysis of safety data from spontaneous European Union regulatory network. Driven by the full reporting systems has a proven value for the detection and implementation of the 2010 pharmacovigilance legislation, analysis of the risks of medicines following their placement EudraVigilance has undergone further enhancements on the market and use in medical practice. EudraVigilance together with a major revision of its access policy, taking is the pharmacovigilance database to manage the collection into account the use of the new individual case safety and analysis of suspected adverse reactions to medicines report standard developed by the International Council for authorised in the European Economic Area. EudraVigi- Harmonization of Technical Requirements for Pharma- lance first operated in December 2001, with access to the ceuticals for Human Use and the International Organiza- database being governed by the EudraVigilance access tion for Standardization. The aim of the broadened access policy. We performed a literature search including data up is to facilitate more effective safety monitoring of autho- to December 2016 to demonstrate how the data from rised medicines, to make more data available for research EudraVigilance has been used in scientific publications. and to provide better access to information on suspected We describe the results, including by type of publication, adverse reactions for healthcare professionals and patients. -

European Medicines Agency Policy on Access to Eudravigilance Data for Medicinal Products for Human Use (Eudravigilance Access Policy)
23 August 2019 EMA/759287/2009 Revision 4* Inspections, Human Medicines Pharmacovigilance & Committees Division European Medicines Agency policy on access to EudraVigilance data for medicinal products for human use (EudraVigilance Access Policy) Start of public consultation 4 August 2014 End of public consultation 15 September 2014 Final draft agreed by Project Team 1 “Collection of key information September 2015 on medicines” of the EMA/Member States governance structure for the implementation of the pharmacovigilance legislation Final draft submitted to the EudraVigilance Expert Working Group for 23 September 2015 information Final draft agreed by Pharmacovigilance Risk Assessment Committee 5-8 October 2015 (PRAC) Final draft agreed by Project Co-ordination Group of the 12 October 2015 EMA/Member States governance structure for the implementation of the pharmacovigilance legislation Final draft agreed by the European Risk Management Facilitation 12 October 2015 Group (ERMS-FG) Final draft agreed by the Committee for Human Medicinal Products 19-21 October 2015 (CHMP) and the Co-ordination group for Mutual recognition and Decentralised procedures – human( CMD-h) Final draft submitted to IT Directors for information 22 October 2015 Final draft submitted to Heads of Medicines Agencies Human (HMA- 21-23 October 2015 h) for information Revision 2 adopted by the EMA Management Board 16-17 December 2015 Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us An agency of the European Union Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 © European Medicines Agency, 2019. -
Experiences with Adverse Drug Reaction Reporting by Patients an 11-Country Survey
Drug Saf 2012; 35 (1): 45-60 ORIGINAL RESEARCH ARTICLE 0114-5916/12/0001-0045/$49.95/0 ª 2012 Adis Data Information BV. All rights reserved. Experiences with Adverse Drug Reaction Reporting by Patients An 11-Country Survey Florence van Hunsel,1,2 Linda Ha¨rmark,1,2 Shanthi Pal,3 Sten Olsson4 and Kees van Grootheest1,2 1 Netherlands Pharmacovigilance Centre Lareb, ‘s-Hertogenbosch, the Netherlands 2 University of Groningen, Department of Pharmacy, Pharmacotherapy and Pharmaceutical Care, Groningen, the Netherlands 3 Quality Assurance and Safety of Medicines, World Health Organization, Geneva, Switzerland 4 World Health Organization Collaborating Centre for International Drug Monitoring, Uppsala, Sweden Abstract Background: Patients are important stakeholders in pharmacovigilance; how- ever, little formal evaluation has been undertaken of existing patient reporting schemes within and outside Europe. If patient reporting is to be recognized as beneficial for pharmacovigilance and further optimized, methodology and best practice must be internationally shared and promoted. Objective: This study aims to review the methods of patient reporting of adverse drug reactions (ADRs) in 11 countries worldwide and to compare different aspects of their experiences. Methods: A survey based on telephone interviews, e-mail discussions and field visits of existing practices in consumer and patient reporting of ADRs was performed in the second half of 2010. Results: The start dates of the patient reporting schemes vary from 1964 (Australia) to 2010 (Norway). The number of patient reports per country varies widely. Most countries would ideally spend more resources on making the public aware of the possibility that patients can report ADRs. Most countries have three different ways for patients to report ADRs – a paper form, an electronic form on a website or by telephone. -

Transparency of Authorities: Opportunities and Restrictions
Transparency of authorities: opportunities and restrictions Wissenschaftliche Prüfungsarbeit zur Erlangung des Titels „Master of Drug Regulatory Affairs“ der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Dr. Nadine Corvey aus Hanau Bonn 2010 Betreuer und 1. Referent: Prof. Burkhard Sträter Zweite Referentin: Dr. Christine Haas Transparency of authorities ─ opportunities and restrictions Table of Contents List of Abbreviations....................................................................................................................2 1. Introduction ...................................................................................................................3 2. Legislative framework leading to increased transparency........................................4 2.1. European Union ..............................................................................................................4 2.2. National Provisions .........................................................................................................9 3. Transparency within the European Medicines Regulatory System ........................12 3.1. Implementation of transparency by the European Medicines Agency (EMEA) .............12 3.1.1 Transparency in the EMEA daily business ....................................................................12 3.1.2 Direct interaction with stakeholders...............................................................................25 3.1.3 Cooperation within the -

Paediatric Safety Signals Identified in Vigibase: Methods and Results from Uppsala Monitoring Centre
Received: 19 May 2018 Revised: 1 October 2018 Accepted: 10 December 2018 DOI: 10.1002/pds.4734 ORIGINAL REPORT Paediatric safety signals identified in VigiBase: Methods and results from Uppsala Monitoring Centre Kristina Star1,2 | Lovisa Sandberg1 | Tomas Bergvall1 | Imti Choonara3 | Pia Caduff‐Janosa1 | I. Ralph Edwards1 1 Research Section, Uppsala Monitoring Centre, Uppsala, Sweden Abstract 2 Department of Public Health and Caring Purpose: The purpose of this study is to uncover previously unrecognised risks of Sciences, Uppsala University, Uppsala, medicines in paediatric pharmacovigilance reports and thereby advance a safer use Sweden 3 Division of Medical Sciences and Graduate of medicines in paediatrics. Entry Medicine, University of Nottingham, Methods: Individual case safety reports (ICSRs) with ages less than 18 years were Derby, UK retrieved from VigiBase, the World Health Organization (WHO) global database of ICSRs, Correspondence K. Star, Research Section, Uppsala Monitoring in September 2014. The reports were grouped according to the following age spans: 0 to Centre, Uppsala, Sweden. 27 days; 28 days to 23 months; 2 to 11 years; and 12 to 17 years. vigiRank, a data‐driven Email: kristina.star@who‐umc.org predictive model for emerging safety signals, was used to prioritise the list of drug events by age groups. The list was manually assessed, and potential signals were identified to undergo in‐depth assessment to determine whether a signal should be communicated. Results: A total of 472 drug‐event pairs by paediatric age groups were the subject of an initial manual assessment. Twenty‐seven drug events from the two older age groups were classified as potential signals. -

Spontaneous Reports of Vasculitis As an Adverse Event Following
Vaccine 34 (2016) 6634–6640 Contents lists available at ScienceDirect Vaccine j ournal homepage: www.elsevier.com/locate/vaccine Spontaneous reports of vasculitis as an adverse event following immunization: A descriptive analysis across three international databases a,∗ a a a Patrizia Felicetti , Francesco Trotta , Caterina Bonetto , Carmela Santuccio , b c,d e f Yolanda Brauchli Pernus , David Burgner , Rebecca Chandler , Giampiero Girolomoni , g h i j k Robert D.M. Hadden , Sonali Kochhar , Merita Kucuku , Giuseppe Monaco , Seza Ozen , l m n o p Barbara Pahud , Linny Phuong , Novilia Sjafri Bachtiar , Amina Teeba , Karina Top , q r s t Frederick Varricchio , Robert P. Wise , Giovanna Zanoni , Sasaˇ Zivkovicˇ , u,b 1 Jan Bonhoeffer , for the Brighton Collaboration Vasculitis Working Group a Italian Medicines Agency, Rome, Italy b Brighton Collaboration Foundation, Basel, Switzerland c Monash Children’s Hospital-Clayton, Melbourne, Australia d Murdoch Children’s Research Institute (MCRI) - Department of Paediatrics, Melbourne University, Australia e Uppsala Monitoring Centre, Uppsala, Sweden f University of Verona, Department of Medicine, Section of Dermatology and Venereology, Verona, Italy g King’s College Hospital, London, UK h USAID, Deliver Project, JSIPL, New Delhi, India i Department of Vaccines Control, National Agency for Medicine & Medical Devices, Tirana, Albania j Centre for Pharmacovigilance, The Lombardy Region, Milan, Italy k Hacettepe University, Department of Pediatric Rheumatology, Ankara, Turkey l Children’s Mercy Hospital, -

The Launch of the New Eudravigilance System Questions and Answers (Q&A) from Stakeholders
5 October 2017 EMA/629943/2017 The launch of the new EudraVigilance System Questions and Answers (Q&A) from stakeholders Version 1.2 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2017. Reproduction is authorised provided the source is acknowledged. Table of contents Table of contents ........................................................................................................ 2 Glossary .................................................................................................................... 3 Introduction ............................................................................................................... 5 1. EudraVigilance organisation and user registration ........................................................ 6 2. Use of EVWEB and the ICSR download manager ....................................................... 13 3. Medical Literature Monitoring .................................................................................. 48 4. Guideline on good pharmacovigilance practices: Module VI – Management and reporting of adverse reactions to medicinal products ................................................................... 50 5. Reporting to National Competent Authorities in the EEA ............................................. 69 6. Guideline on good pharmacovigilance practices: Module IX - Signal -

Screening for Adverse Reactions in Eudravigilance
19 December 2016 EMA/849944/2016 Inspections, Human Medicines, Pharmacovigilance and Committees Division Screening for adverse reactions in EudraVigilance Table of contents 1. Introduction ............................................................................................ 3 2. Scope....................................................................................................... 4 3. An integrated approach to signal detection ............................................. 5 3.1. Considerations related to performance .................................................................... 5 4. Screening for adverse reactions in the total population .......................... 6 4.1. Disproportionality methods .................................................................................... 6 4.1.1. Components of the statistical signal detection system based on disproportionality methods .................................................................................................................... 6 4.1.2. Selection of a disproportionality method ............................................................... 7 4.1.3. Thresholds defining SDRs in EudraVigilance .......................................................... 9 4.1.4. Subgroup analyses and stratification .................................................................. 11 4.1.5. Some operational choices ................................................................................. 15 4.2. Alternatives to SDR based on clinical information .................................................. -
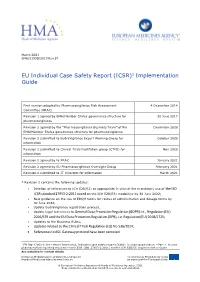
ICSR)1 Implementation Guide
March 2021 EMA/51938/2013 Rev 2* EU Individual Case Safety Report (ICSR)1 Implementation Guide First version adopted by Pharmacovigilance Risk Assessment 4 December 2014 Committee (PRAC) Revision 1 agreed by EMA/Member States governance structure for 30 June 2017 pharmacovigilance Revision 2 agreed by the “Pharmacovigilance Business Team” of the December 2020 EMA/Member States governance structure for pharmacovigilance Revision 2 submitted to EudraVigilance Expert Working Group for October 2020 information Revision 2 submitted to Clinical Trials Facilitation group (CTFG) for Nov 2020 information Revision 2 agreed by to PRAC January 2021 Revision 2 agreed by EU Pharmacovigilance Oversight Group February 2021 Revision 2 submitted to IT Directors for information March 2021 * Revision 2 contains the following updates: • Deletion of references to ICH E2B(R2) as appropriate in view of the mandatory use of the ISO ICSR standard 27953-2:2011 based on the ICH E2B(R3) modalities by 30 June 2022; • New guidance on the use of EDQM terms for routes of administration and dosage forms by 30 June 2022; • Update EudraVigilance registration process; • Update legal references to General Data Protection Regulation (GDPR) i.e., Regulation (EU) 2016/679 and the EU Data Protection Regulation (DPR), i.e. Regulation (EU) 2018/1725; • Updates to the Business Rules; • Updates related to the Clinical Trials Regulation (EU) No 536/2014; • References to AS1 Gateway protocol have been removed. 1 EN ISO 27953-2:2011 Health Informatics, Individual case safety reports (ICSRs) in pharmacovigilance — Part 2: Human pharmaceutical reporting requirements for ICSR (ISO 27953-2:2011) and the ICH E2B(R3) Implementation Guide See websites for contact details European Medicines Agency www.ema.europa.eu The European Medicines Agency is Heads of Medicines Agencies www.hma.eu an agency of the European Union © European Medicines Agency and Heads of Medicines Agencies, 2021.