Virtual Governing Body
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leigh Centurions V ROCHDALE HORNETS
Leigh Centurions SUvN DRAOY C17HTDH AMLAREC H O20R1N9 @ET 3S PM # LEYTHERS # OURTOWNOURCLUB# OURTOWNOURCLUB # LEYTHERS # OURTOWNOURCLUB# OURTOWNOURCLUB engage with the fans at games and to see the players acknowledged for their efforts at the Toronto game, despite the narrowness of the defeat, was something Welcome to Leigh Sports Village for day 48 years ago. With a new community that will linger long in the memory. this afternoon’s Betfred stadium in the offing for both the city’s Games are coming thick and fast at FChamRpionshOip gameM agains t oTur HfootbEall team s iTt could Oalso welPl also be present and the start of our involvement in friends from Rochdale Hornets. the last time Leigh play there. the Corals Challenge Cup and the newly- Carl Forster is to be commended for It’s great to see the Knights back on the instigated 1895 Cup and the prospect of taking on the dual role of player and coach up after years in the doldrums and to see playing at Wembley present great at such a young age and after cutting his interest in the professional game revived opportunities and goals for Duffs and his teeth in two years at Whitehaven, where under James Ford’s astute coaching. players. The immediate task though is to he built himself a good reputation, he now Watching York back at their much-loved carry on the good form in a tight and has the difficult task of preserving Wiggington Road ground was always one competitive Championship where every Hornets’ hard-won Championship status in of the best away days in the season and I win is hard-earned and valuable. -
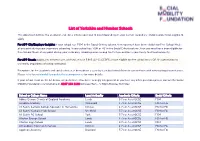
List of Yorkshire and Humber Schools
List of Yorkshire and Humber Schools This document outlines the academic and social criteria you need to meet depending on your current secondary school in order to be eligible to apply. For APP City/Employer Insights: If your school has ‘FSM’ in the Social Criteria column, then you must have been eligible for Free School Meals at any point during your secondary schooling. If your school has ‘FSM or FG’ in the Social Criteria column, then you must have been eligible for Free School Meals at any point during your secondary schooling or be among the first generation in your family to attend university. For APP Reach: Applicants need to have achieved at least 5 9-5 (A*-C) GCSES and be eligible for free school meals OR first generation to university (regardless of school attended) Exceptions for the academic and social criteria can be made on a case-by-case basis for children in care or those with extenuating circumstances. Please refer to socialmobility.org.uk/criteria-programmes for more details. If your school is not on the list below, or you believe it has been wrongly categorised, or you have any other questions please contact the Social Mobility Foundation via telephone on 0207 183 1189 between 9am – 5:30pm Monday to Friday. School or College Name Local Authority Academic Criteria Social Criteria Abbey Grange Church of England Academy Leeds 5 7s or As at GCSE FSM Airedale Academy Wakefield 4 7s or As at GCSE FSM or FG All Saints Catholic College Specialist in Humanities Kirklees 4 7s or As at GCSE FSM or FG All Saints' Catholic High -

Leigh Centurions V WIDNES VIKINGS
Leigh Centurions v WIDNES VIKINGS SUNDAY 28TH JULY 2019 @ 4PM AB SUNDECKS 1895 CUP SEMI FINAL # LEYTHERS # OURTOWNOURCLUB # LEYTHERS # OURTOWNOURCLUB AB SUNDECKS BECOME TITLE SPONSORS OF THE 1895 Cup FROM THE TOP Welcome to this afternoon’s AB Alex Murphy with cup 1971 It was great to see Adam Higson returning to Sundecks 1895 Cup semi-final the club and to see the way Junior Sa’u and Leigh Centurions club sponsor AB Mitch Clark have already settled in. Sundecks expanded its support of against Widnes Vikings. Rugby League by becoming title It’s a big game for both clubs and both sets of Meanwhile young Josh Simm made his Super players. I was speaking to Tony Barrow in the League debut at London last Sunday, one of sponsor of the inaugural 1895 Cup, nine Saints players in the team that day the final of which will be played at week ahead of him being our special guest this afternoon in Premier Club. that’ve played for Leigh this year. Wembley Stadium on Saturday, 24 Congratulations to Josh and thanks again for August: Tony was a key member of the 1971 all the Saints lads who have fully bought into Wembley team having played for Saints in playing for Leigh Centurions. AB Sundecks has established itself as one their 1966 success over Wigan. of the UK’s leading manufacturers and Tony was a top player in his day and was in Ryan Brierley installers of complete PVCu decking top form in the 1973-74 season and solutions to the leisure and domestic considered a shoe-in for a place on the GB markets. -
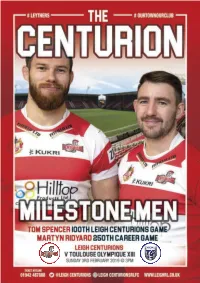
1Toulouse.Pdf
aaa Leigh v Toulouse 56pp.qxp_Layout 1 01/02/2019 08:49 Page 1 aaa Leigh v Toulouse 56pp.qxp_Layout 1 01/02/2019 08:39 Page 2 # LEYTHERS # OURTOWNOURCLUB# OURTOWNOURCLUB aaa Leigh v Toulouse 56pp.qxp_Layout 1 01/02/2019 08:39 Page 3 # LEYTHERS # OURTOWNOURCLUB# OURTOWNOURCLUB MIKEFROM LATHAM THE TOP CHAIRMAN,Welcome to Leigh Sports Village OPERATIONAL for that day would soon be our BOARD Messiah. Chris Hall came along and filmed the this afternoon’s Betfred On 1 November we had to file our new-look Leigh, working to put the Championship opener against preliminary 2019 squad list to the RFL. pride back into the club. His fantastic Toulouse Olympique. On it were just two names. By three-minute feature on ITV Granada It’s great to be back isn’t it? Last Christmas we had 20 and the reached out to 750k viewers. Sunday’s Warm Up game against metamorphosis was almost complete. The last few weeks have been hectic, London Broncos was a really The key to it all, appointing John Duffy preparing for the season and at the worthwhile exercise and it was great to as coach. He immediately injected Championship launch at York there was see over 2,000 Leigh fans in the positivity, local knowledge and a ready a palpable air of excitement for the ground, despite the bitterly cold smile, a bulging contacts book and with prospects of a great competition to weather. it a long list of players who were come. We are extremely grateful to our bursting to play for the club. -
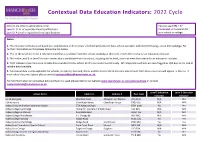
Education Indicators: 2022 Cycle
Contextual Data Education Indicators: 2022 Cycle Schools are listed in alphabetical order. You can use CTRL + F/ Level 2: GCSE or equivalent level qualifications Command + F to search for Level 3: A Level or equivalent level qualifications your school or college. Notes: 1. The education indicators are based on a combination of three years' of school performance data, where available, and combined using z-score methodology. For further information on this please follow the link below. 2. 'Yes' in the Level 2 or Level 3 column means that a candidate from this school, studying at this level, meets the criteria for an education indicator. 3. 'No' in the Level 2 or Level 3 column means that a candidate from this school, studying at this level, does not meet the criteria for an education indicator. 4. 'N/A' indicates that there is no reliable data available for this school for this particular level of study. All independent schools are also flagged as N/A due to the lack of reliable data available. 5. Contextual data is only applicable for schools in England, Scotland, Wales and Northern Ireland meaning only schools from these countries will appear in this list. If your school does not appear please contact [email protected]. For full information on contextual data and how it is used please refer to our website www.manchester.ac.uk/contextualdata or contact [email protected]. Level 2 Education Level 3 Education School Name Address 1 Address 2 Post Code Indicator Indicator 16-19 Abingdon Wootton Road Abingdon-on-Thames -

Eligible If Taken A-Levels at This School (Y/N)
Eligible if taken GCSEs Eligible if taken A-levels School Postcode at this School (Y/N) at this School (Y/N) 16-19 Abingdon 9314127 N/A Yes 3 Dimensions TA20 3AJ No N/A Abacus College OX3 9AX No No Abbey College Cambridge CB1 2JB No No Abbey College in Malvern WR14 4JF No No Abbey College Manchester M2 4WG No No Abbey College, Ramsey PE26 1DG No Yes Abbey Court Foundation Special School ME2 3SP No N/A Abbey Gate College CH3 6EN No No Abbey Grange Church of England Academy LS16 5EA No No Abbey Hill Academy TS19 8BU Yes N/A Abbey Hill School and Performing Arts College ST3 5PR Yes N/A Abbey Park School SN25 2ND Yes N/A Abbey School S61 2RA Yes N/A Abbeyfield School SN15 3XB No Yes Abbeyfield School NN4 8BU Yes Yes Abbeywood Community School BS34 8SF Yes Yes Abbot Beyne School DE15 0JL Yes Yes Abbots Bromley School WS15 3BW No No Abbot's Hill School HP3 8RP No N/A Abbot's Lea School L25 6EE Yes N/A Abbotsfield School UB10 0EX Yes Yes Abbotsholme School ST14 5BS No No Abbs Cross Academy and Arts College RM12 4YB No N/A Abingdon and Witney College OX14 1GG N/A Yes Abingdon School OX14 1DE No No Abraham Darby Academy TF7 5HX Yes Yes Abraham Guest Academy WN5 0DQ Yes N/A Abraham Moss Community School M8 5UF Yes N/A Abrar Academy PR1 1NA No No Abu Bakr Boys School WS2 7AN No N/A Abu Bakr Girls School WS1 4JJ No N/A Academy 360 SR4 9BA Yes N/A Academy@Worden PR25 1QX Yes N/A Access School SY4 3EW No N/A Accrington Academy BB5 4FF Yes Yes Accrington and Rossendale College BB5 2AW N/A Yes Accrington St Christopher's Church of England High School -

School Name POSTCODE AUCL Eligible If Taken GCSE's at This
School Name POSTCODE AUCL Eligible if taken GCSE's at this AUCL Eligible if taken A-levels at school this school City of London School for Girls EC2Y 8BB No No City of London School EC4V 3AL No No Haverstock School NW3 2BQ Yes Yes Parliament Hill School NW5 1RL No Yes Regent High School NW1 1RX Yes Yes Hampstead School NW2 3RT Yes Yes Acland Burghley School NW5 1UJ No Yes The Camden School for Girls NW5 2DB No No Maria Fidelis Catholic School FCJ NW1 1LY Yes Yes William Ellis School NW5 1RN Yes Yes La Sainte Union Catholic Secondary NW5 1RP No Yes School St Margaret's School NW3 7SR No No University College School NW3 6XH No No North Bridge House Senior School NW3 5UD No No South Hampstead High School NW3 5SS No No Fine Arts College NW3 4YD No No Camden Centre for Learning (CCfL) NW1 8DP Yes No Special School Swiss Cottage School - Development NW8 6HX No No & Research Centre Saint Mary Magdalene Church of SE18 5PW No No England All Through School Eltham Hill School SE9 5EE No Yes Plumstead Manor School SE18 1QF Yes Yes Thomas Tallis School SE3 9PX No Yes The John Roan School SE3 7QR Yes Yes St Ursula's Convent School SE10 8HN No No Riverston School SE12 8UF No No Colfe's School SE12 8AW No No Moatbridge School SE9 5LX Yes No Haggerston School E2 8LS Yes Yes Stoke Newington School and Sixth N16 9EX No No Form Our Lady's Catholic High School N16 5AF No Yes The Urswick School - A Church of E9 6NR Yes Yes England Secondary School Cardinal Pole Catholic School E9 6LG No No Yesodey Hatorah School N16 5AE No No Bnois Jerusalem Girls School N16 -

Leigh Centurions V HALIFAX
Leigh Centurions v HALIFAX SUNDAY 9TH JUNE 2019 @ 3PM FROM# LEYTHERS THE TOP# OURTOWNOURCLUB Welcome to Leigh Sports Village for conditioning work and took part in some For Jamie Acton, sadly his playing days this afternoon’s Betfred punishing Saturday morning training are over. Jamie announced his retirement Championship game against Halifax. sessions at places like Rivington Pike and from the game recently due to injury, a The visit of ‘Fax is always one of the Borsdane Woods. Seeing at first hand the career sadly cut short far too early. The highlights of the season and it’s great to extent to which our players push board have invited Jamie and his family meet up with old friends and chew the themselves to prepare for playing the down to LSV to celebrate his career and fat. Halifax are one of a declining number game for our enjoyment is a humbling say thanks to the Leigh fans in the north of clubs who really make you welcome at experience. and west stands and hopefully he will be their ground and MC Pete Emmett does a Doubtless the Halifax players went able to do this shortly. It goes without brilliant job hosting their banqueting suite through exactly the same kind of rigorous saying that we all wish him every success before the game. It was great to spend pre-season activities. After all, there are and happiness in the future. time chatting with Wilf George when we far more hills around Halifax than there ............................................................. visited The Shay earlier this season and are around Leigh and great days like last Maurice Bamford Wilf must have been as proud as anyone Sunday, beating Bradford at Odsal in front last Sunday after the tremendous of a national television audience must Challenge Cup win at Bradford. -
Contextual Data Education Indicators: 2020 Cycle
Contextual Data Education Indicators: 2020 Cycle Schools are listed in alphabetical order. You can use CTRL + F/ Level 2: GCSE or equivalent level qualifications Command + F to search for Level 3: A Level or equivalent level qualifications your school or college. Notes: 1. The education indicators are based on a combination of three years' of school performance data, where available, and combined using z-score methodology. For further information on this please follow the link below. 2. 'Yes' in the Level 2 or Level 3 column means that a candidate from this school, studying at this level, meets the criteria for an education indicator. 3. 'No' in the Level 2 or Level 3 column means that a candidate from this school, studying at this level, does not meet the criteria for an education indicator. 4. 'N/A' indicates that there is no reliable data available for this school for this particular level of study. All independent schools are also flagged as N/A due to the lack of reliable data available. 5. Contextual data is only applicable for schools in England, Scotland, Wales and Northern Ireland meaning only schools from these countries will appear in this list. If your school does not appear please contact [email protected]. For full information on contextual data and how it is used please refer to our website www.manchester.ac.uk/contextualdata or contact [email protected]. Level 2 Education Level 3 Education School Name Address 1 Address 2 Post Code Indicator Indicator 16-19 Abingdon Wootton Road Abingdon-on-Thames -

Virtual Governing Body
Virtual Governing Body To be held on Thursday 2 September 2021 From 1.00 pm until 3.30 pm VIRTUAL GOVERNING BODY To be held on Thursday, 2 September 2021 at 1pm A G E N D A Ref Item Enclosure Led By Action Required 1. Apologies for Absence Verbal Dr Crichton For noting 2. Declarations of Interest Verbal All For noting The CCG’s register is available via the Governance team or on the CCG website which can be accessed here. 3. Minutes of the meeting held on 1 July Enc A Dr Crichton For approval 2021 4. Matters Arising not on the Agenda Verbal Dr Crichton For discussion 5. Notification of Any Other Business Verbal Dr Crichton For discussion 6. Questions from Members of the Public Verbal Dr Crichton For discussion (See our website for how to submit questions – required in advance) 7. Patient Story Verbal Dr Crichton For discussion Strategy 8. LeDeR Annual Report Enc B I Boldy For approval 9. Joint Commissioning Strategy & Enc C Dr Crichton For approval delegation to the Joint Committee Clinical Commissioning Groups 10. Healthwatch Doncaster Annual Report Enc D S Whittle For noting 2020/2021 11. Audit Committee Annual Report Enc E P Wilkin For noting Assurance 12. Quality & Performance Report Enc F A Fitzgerald & For noting A Russell • Spotlight Report on Living Well 13. Finance Report Enc G T Wyatt For noting 14. Governing Body Assurance Framework – Enc H C Rollinson For approval Quarter 1 Page 1 of 2 Ref Item Enclosure Led By Action Required 15. Chair and Chief Officers Report Enc I Dr Crichton & J For noting Pederson Items to Note 16. -

University Technical College Serving Sheffield City Region ______
FORM 2 SHEFFI ELD CITY COUNCILAgenda Item 10 Cabinet Report Report of: Executive Director, CYPF ________________________________________________________________ Report to: Cabinet ________________________________________________________________ Date: 27 May 2015 ________________________________________________________________ Subject: A second University Technical College serving Sheffield City Region ________________________________________________________________ Author of Report: Tony Tweedy 0114 2296140 ________________________________________________________________ Key Decision: YES ________________________________________________________________ Reason Key Decision: Expenditure/savings over £500,000* Affects 2 or more wards* ___________________________________________________________ _____ Summary: The Department for Education (DfE) has approved the City’s application, submitted by the Sheffield College, to establish a second University Technical College (UTC2) in the Lower Don Valley. In return, the DfE has asked that the local authority transfers the land to the UTC Trust on a 125 year lease at a peppercorn ground rent. The local authority has been invited to be a member of the Governing Body of the UTC. The procurement of the construction of the building will be a matter solely for the UTC Academy Trust in association with DfE consultants. The UTC 2 for Human Sciences and Computing has, as with the city’s first UTC, been developed in partnership with local employers and is designed to address skills shortages and gaps reported -

Medicine Contextual Schools If the School Where You Studied for Gcses and a Levels Is on the List Below, an Application Will Be Assigned a Contextual Score
University of Birmingham Medicine Contextual Schools If the school where you studied for GCSEs and A Levels is on the list below, an application will be assigned a contextual score. If you moved schools, only one of those schools needs to be on the list below. The schools have been identified using the criteria described on our website (www.birmingham.ac.uk/applying-to-medicine) Please use the 'Find' facility of your PDF Reader programme to search for your school. Because schools can be known by quite different names, we suggest that you search using the first part (only) of a postcode and work through the schools identified by that strategy. DfE SCHNAME PCODE 2024000 The UCL Academy NW3 3AQ 2024104 Haverstock School NW3 2BQ 2024166 Parliament Hill School NW5 1RL 2024196 Regent High School NW1 1RX 2024275 Hampstead School NW2 3RT 2024285 Acland Burghley School NW5 1UJ 2024652 Maria Fidelis Roman Catholic Convent School FCJ NW1 1TA 2024652 Maria Fidelis Catholic School FCJ NW1 1LY 2024688 William Ellis School NW5 1RN 2024952 LaSWAP Sixth Form NW5 1RP 2025401 La Sainte Union Catholic Secondary School NW5 1RP 2027137 Camden Centre for Learning (CCfL) Special School NW1 8DP 2028045 Capital City College Group NW1 3HB 2028045 The WKCIC Group WC1X 8RA 2034000 Harris Academy Greenwich SE9 5EQ 2034001 Ark Greenwich Free School SE18 4LH 2034006 Royal Greenwich Trust School SE7 8LJ 2034007 The Halley Academy SE3 8EP 2034077 Eltham Hill School SE9 5EE 2034130 Plumstead Manor School SE18 1QF 2034243 Corelli College SE3 8EP 2034250 Woolwich Polytechnic