Advances in Medicine and Biology. Volume
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Screening D'activités Hydrolytiques
REPUBLIQUE ALGERIENNE DEMOCRATIQUE ET POPULAIRE MINISTERE DE L’ENSEIGNEMENT SUPERIEUR ET DE LA RECHERCHE SCIENTIFIQUE UNIVERSITE MENTOURI-CONSTANTINE Institut de la Nutrition, de l’Alimentation et des Technologies Agro-alimentaires (INATAA) Département de Biotechnologie alimentaire N° d’ordre : Série : MEMOIRE Présenté en vue de l’obtention du diplôme de Magister en Sciences Alimentaires Option : Biotechnologie Alimentaire Screening d’activités hydrolytiques extracellulaires chez des souches bactériennes aérobies thermophiles isolées à partir de sources thermales terrestres de l’Est algérien Présenté par GOMRI Mohamed Amine Devant le jury composé de : Président : Pr. AGLI A. Professeur INATAA, UMC Rapporteur : Dr. KHARROUB K. Docteur INATAA, UMC Examinateurs : Pr. KACEM CHAOUACHE N. Professeur Faculté des SNV, UMC Dr. BARKAT M. Docteur INATAA, UMC Année universitaire 2011-2012 Remerciements Je rends grâce à Dieu, le miséricordieux, le tout puissant, pour ce miracle appelé vie, que sa lumière nous guide vers lui, et que son nom soit l’élixir de nos peines et douleurs. Tout d’abord, je tiens à remercier Madame KHARROUB Karima pour m’avoir donné la chance de travailler sous sa direction, pour sa confiance en moi et ses encouragements mais surtout pour sa générosité dans le travail, qu’elle trouve en ces mots toute ma gratitude. Mes remerciements sont adressés aux membres du Jury qui ont pris sur leur temps et ont bien voulu accepter de juger ce modeste travail : Mr le professeur AGLI qui m’a fait l’honneur de présider ce Jury Mr le professeur KACEM-CHAOUCH E qui a eu l’amabilité de participer à ce Jury Mme BARKAT qui a bien voulu examiner ce travail Je tiens à remercier Mlle AYAD Ryma, Mesdames ZOUBIRI Lamia et DJABALI Saliha, Messieurs ZOUAOUI Nassim, BOUGUERRA Ali, SLIMANI Zakaria et FARHAT Chouaib pour leur aide inestimable, mais aussi pour leur amitié précieuse, qu’ils trouvent ici les plus sincères marques d’affection. -

Phylogenetic Study of Thermophilic Genera Anoxybacillus, Geobacillus
bioRxiv preprint doi: https://doi.org/10.1101/2021.06.18.449068; this version posted June 19, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 bioRxiv 2 Article Type: Research article. 3 Article Title: Phylogenetic study of thermophilic genera Anoxybacillus, Geobacillus, 4 Parageobacillus, and proposal of a new classification Quasigeobacillus 5 gen. nov. 6 Authors: Talamantes-Becerra, Berenice1-2*; Carling, Jason2; Blom, Jochen3; 7 Georges, Arthur1 8 Affiliation: 1Institute for Applied Ecology, University of Canberra ACT 2601 9 Australia. 10 2Diversity Arrays Technology Pty Ltd, Bruce, Canberra ACT 2617 11 Australia. 12 3Bioinformatics & Systems Biology, Justus-Liebig-University Giessen, 13 35392 Glessen, Hesse, Germany 14 *Correspondence: Berenice Talamantes Becerra, Institute for Applied Ecology, 15 University of Canberra ACT 2601 Australia. Email: 16 [email protected] 17 Running head: Phylogenetic study of thermophilic bacteria. 18 Word Count: Abstract: 178 Main body: 3709 References: n= 60 19 20 21 bioRxiv preprint doi: https://doi.org/10.1101/2021.06.18.449068; this version posted June 19, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 22 23 Abstract 24 A phylogenetic study of Anoxybacillus, Geobacillus and Parageobacillus was performed using 25 publicly available whole genome sequences. A total of 113 genomes were selected for 26 phylogenomic metrics including calculation of Average Nucleotide Identity (ANI) and 27 Average Amino acid Identity (AAI), and a maximum likelihood tree was built from alignment 28 of a set of 662 orthologous core genes. -

A TRIBUTE in LOVING MEMORY Irina Diana Tarabac
A TRIBUTE IN LOVING MEMORY Irina Diana Tarabac (1970-2007) Irina Diana Tarabac dedicated her life to learning, teaching, and science – the field of her choice being linguistics. Among many brilliant scholars and scientists in the Linguistics Department at Stony Brook University, Irina stood out for many a reasons. Unfortunately, Irina left us too early in October 2007. After arriving to study at Stony Brook at 2002, Irina became an active member of the linguistic community in the metropolitan area of New York. She frequently attended seminars in the Linguistics Departments of NYU and the CUNY Graduate Center. Irina was dedicated to life-long learning, and she set extremely high standards for herself, her own research and her teaching responsibilities. She taught a morphology seminar in Bucharest and served as a TA for classes on many different topics at Stony Brook, including syntax, morphology, language philosophy, phonology, typology, and Semitic languages. She was a wonderful teacher and was very concerned about her students. Her dedication to linguistics didn’t leave her much time to pursue her hobbies, but whenever Irina found some time off, she enjoyed listening to symphonic music, reading good literature, visiting museums, and spending time with her friends. Irina earned a Master’s degree in Bucharest, Romania in 1996 and had studied and conducted research in the Netherlands between 1997 and 1999. Irina conducted research on well-known languages such as Dutch, Romanian, and Modern Greek as well as less-known languages such as Rapanui and Burushaki. Irina’s passing is a great loss to her family, her friends and the field of linguistics. -
The First Berkeley Meeting
__________________________________________________________ FASL 23, 2014 ________________________________________________________ Michigan Slavic Publications is a non-profit organization associated with the Department of Slavic Languages and Literatures of the University of Michigan. Its goal is to publish titles which substantially aid the study of and teaching of Slavic and East European languages and cultures. The present volume, based on a conference held at the University of California at Berkeley in May 2014, continues a series of conference proceedings devoted to formal approaches to Slavic languages. Michigan Slavic Materials, 61 Series Editor Jindřich Toman [email protected] Annual Workshop on Formal Approaches to Slavic Linguistics ______________________________ The First Berkeley Meeting Edited by Małgorzata Szajbel-Keck Roslyn Burns Darya Kavitskaya Michigan Slavic Publications Ann Arbor 2015 collection © Michigan Slavic Publications 2015 individual contributions © authors Library of Congress Cataloging-in-Publication Data Annual Workshop on Formal Approaches to Slavic Linguistics (23rd : 2014 : Berkeley, California) Annual Workshop On Formal Approaches To Slavic Linguistics : the first Berkeley meeting / edited by Malgorzata Szajbel-Keck, Roslyn Burns, Darya Kavitskaya. pages cm. -- (Michigan Slavic materials, 61) "The present volume, based on a conference held at the University of California at Berkeley, in May 2014 continues a series of conference proceedings devoted to formal approaches to Slavic languages, including Bulgarian, Croatian, Macedonian, Polish, Serbian, and Russian. We are proud to call this volume The First Berkeley Meeting." "Michigan Slavic Publications 2015." "This volume contains selected papers presented at the 23rd Annual Meeting of the Formal Approaches to Slavic Linguistics held May 2/4, 2014 at the University of California, Berkeley." ISBN 978-0-936534-16-9 (alk. -
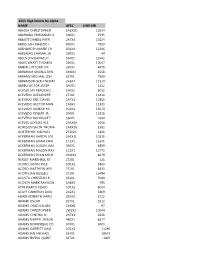
15E5 Ssgt Selects by Alpha
15E5 SSgt Selects by Alpha NAME AFSC LINE-NR ABADIA CHRISTOPHER 2A5X2D 10234 ABARAWA EMMANUEL K 3S0X1 1595 ABBOTT DANIEL PATR 2A7X3 10224 ABDULLAH MALIZIO J 3P0X1 7420 ABENDROTH MARIE CH 00XXX 11386 ABESAMIS CHAMAL JA 2S0X1 44 ABLES LOVIEANGELO 3S0X1 11062 ABLES WYATT THOMAS 2S0X1 10007 ABNER CLIFFORD LEE 3P0X1 4479 ABRAHAM SHARLA DEN 3M0X1 3558 ABRAMS MICHAEL JOH 3E7X1 7500 ABRAMSON SETH NEWM 2A6X4 11510 ABREU VICTOR JOSEP 3P0X1 1412 ACASIO JAY PEROCHO 1P0X1 8032 ACEVEDO ALEXANDER 2T3X1 11416 ACEVEDO ERIC DAVID 2A7X1 12965 ACEVEDO HECTOR MAN 1A0X1 11303 ACEVEDO JANIECE PA 3D0X1 13070 ACEVEDO ROBERT JR 2F0X1 11918 ACEVEDO RODRIGUEZ 3S0X1 2680 ACEVES ULYSSES ALE 2A3X4A 1056 ACHESON SHON THOMA 2A8X2B 5382 ACHTERHOF MICHAEL 2T3X2C 1821 ACKERMAN AARON JOS 2A3X3L 10231 ACKERMAN ADAM CRAI 1C1X1 11641 ACKERMAN LOGAN JAM 3P0X1 8889 ACKERMAN MASON RAY 1C3X1 12772 ACKERMAN RYAN MICH 2M0X3 8079 ACKLEY MARSHALL RY 2T2X1 321 ACORD JUSTIN KYLE 3D1X2 5960 ACORD MATTHEW WILL 2T2X1 5433 ACORN IAN RUSSELL 2T1X1 12494 ACOSTA CHRISTIAN R 3E3X1 7080 ACOSTA MARK RAYMON 2A6X2 495 ACRI MARCO ELIGIO 3D1X2 8009 ACUFF CAMERON DAVI 2A2X1 6869 ADAIR KENNETH HARO 3D0X2 8722 ADAME OSCAR 3E7X1 1512 ADAMS CHAD KALANI 2A6X6 97 ADAMS CHRISTOPHER 2W1X1 10004 ADAMS CYNTHIA N 2A7X3 2658 ADAMS DARRYL JEMON 4B0X1 5627 ADAMS DOMINIQUE CO 3P0X1 3003 ADAMS GARRETT DAVI 3D1X3 11290 ADAMS IAN MICHAEL 3E4X1 10643 ADAMS IRVING QUINT 3E7X1 3407 ADAMS JAMES COLBY 2T3X1 2522 ADAMS JASON ROBERT 1U0X1 7795 ADAMS JOSEPH AARON 2A9X2E 2595 ADAMS KEITH JR 3P0X1 2642 ADAMS KYLE EDWARD 3D0X2 -

Isolation and Identification of Thermophilic Amylolytic Bacteria from Likupang Marine Hydrothermal, North Sulawesi, Indonesia
BIODIVERSITAS ISSN: 1412-033X Volume 22, Number 6, June 2021 E-ISSN: 2085-4722 Pages: 3326-3332 DOI: 10.13057/biodiv/d220638 Isolation and identification of thermophilic amylolytic bacteria from Likupang Marine Hydrothermal, North Sulawesi, Indonesia ELVY LIKE GINTING1,♥, LETHA L. WANTANIA2, EMMA MAUREN MOKO3, REINY A. TUMBOL1, MAYSE S. SIBY1, STENLY WULLUR1 1Faculty of Fisheries and Marine Science, Universitas Sam Ratulangi. Jl. Kampus Unsrat, Manado 95115, North Sulawesi, Indonesia. Tel./fax.: +62-431-868027, email: [email protected] 2Faculty of Mathematics and Natural Sciences, Bonn University. D-53012 Bonn, Germany 3Department of Biology, Faculty of Mathematics and Natural Science, Universitas Negeri Manado. Jl. Raya Tondano, Minahasa 95618, North Sulawesi, Indonesia Manuscript received: 1 April 2021. Revision accepted: 24 May 2021. Abstract. Ginting EL, Wantania LL, Moko EM, Tumbol RA, Siby MS, Wulur S. 2021. Isolation and identification of thermophilic amylolytic bacteria from Likupang Marine Hydrothermal, North Sulawesi, Indonesia. Biodiversitas 22: 3326-3332. The aims of the research were to isolate and identify the amylase-producing thermophilic bacteria from Likupang Marine Hydrothermal, North Sulawesi, Indonesia. The bacteria were characterized based on the colony and cell morphology and subsequently screened for their amylase activities. The bacterial isolates were identified based on 16S rRNA gene sequences. There were 12 thermophilic bacteria isolates from Likupang Marine Hydrothermal that were able to produce amylase. Two selected isolates (L3 and L9) had an amylolytic index value in the range of 3.04-3.52 at 55oC. The colonies of L3 and L9 are circular, and they are Gram positive, rod-shaped, and motile bacteria. -

English Versions of Foreign Names
ENGLISH VERSIONS OF FOREIGN NAMES Compiled by: Paul M. Kankula ( NN8NN ) at [email protected] in May-2001 Note: For non-profit use only - reference sources unknown - no author credit is taken or given - possible typo errors. ENGLISH Czech. French German Hungarian Italian Polish Slovakian Russian Yiddish Aaron Aron . Aaron Aron Aranne Arek Aron Aaron Aron Aron Aron Aron Aronek Aronos Abel Avel . Abel Abel Abele . Avel Abel Hebel Avel Awel Abraham Braha Abram Abraham Avram Abramo Abraham . Abram Abraham Bramek Abram Abrasha Avram Abramek Abrashen Ovrum Abrashka Avraam Avraamily Avram Avramiy Avarasha Avrashka Ovram Achilies . Achille Achill . Akhilla . Akhilles Akhilliy Akhylliy Ada . Ada Ada Ara . Ariadna Page 1 of 147 ENGLISH VERSIONS OF FOREIGN NAMES Compiled by: Paul M. Kankula ( NN8NN ) at [email protected] in May-2001 Note: For non-profit use only - reference sources unknown - no author credit is taken or given - possible typo errors. ENGLISH Czech. French German Hungarian Italian Polish Slovakian Russian Yiddish Adalbert Vojta . Wojciech . Vojtech Wojtek Vojtek Wojtus Adam Adam . Adam Adam Adamo Adam Adamik Adamka Adi Adamec Adi Adamek Adamko Adas Adamek Adrein Adas Adamok Damek Adok Adela Ada . Ada Adel . Adela Adelaida Adeliya Adelka Ela AdeliAdeliya Dela Adelaida . Ada . Adelaida . Adela Adelayida Adelaide . Adah . Etalka Adele . Adele . Adelina . Adelina . Adelbert Vojta . Vojtech Vojtek Adele . Adela . Page 2 of 147 ENGLISH VERSIONS OF FOREIGN NAMES Compiled by: Paul M. Kankula ( NN8NN ) at [email protected] in May-2001 Note: For non-profit use only - reference sources unknown - no author credit is taken or given - possible typo errors. ENGLISH Czech. French German Hungarian Italian Polish Slovakian Russian Yiddish Adelina . -

Geobacillus and Hydrocarbon Utilization R
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Ulster University's Research Portal 21 The Genus Geobacillus and Hydrocarbon Utilization R. Marchant . I. M. Banat* School of Biomedical Sciences, University of Ulster, Coleraine, County Londonderry, Northern Ireland, UK *[email protected] 1 Introduction . .................................................................... 1888 2 The Degradation of Hydrocarbons by Geobacilli . ................................ 1889 3 The Molecular Basis of Thermophily . ............................................. 1891 4 Growth and Survival of Geobacilli Under Different Conditions . ......... 1892 5 Distribution and Ecology of Geobacilli ............................................. 1894 6 Potential Commercial Exploitation and Research Needs . ................... 1894 K. N. Timmis (ed.), Handbook of Hydrocarbon and Lipid Microbiology, DOI 10.1007/978-3-540-77587-4_138, # Springer-Verlag Berlin Heidelberg, 2010 1888 21 The Genus Geobacillus and Hydrocarbon Utilization Abstract: The members of the Gram-positive endospore-forming bacteria that made up the genus Bacillus have been gradually subdivided, during the last few years, into a number of new genera such as Alicyclobacillus, Aneuribacillus, Brevibacillus, Gracilibacillus, Paenibacillus, Salibacillus, Ureibacillus, and Virgibacillus. Nazina et al. in 2001 created the genus Geobacillus based around Bacillus (now Geobacillus) stearothermophilus DSM22 as the type strain. The description included two new species of hydrocarbon-oxidizing bacteria isolated from high- temperature oilfields, and the transfer of six members of genetic group 5 thermophilic species of Bacillus to the new genus. Other additions followed and, most of these species, shared the ability to grow at elevated temperatures and degrade hydrocarbons. The taxonomy of geoba- cilli, hydrocarbon degradation, molecular basis of thermophily, survival, and ecological roles in the environment and possible exploitation potential will be reviewed in this chapter. -

Microbial and Mineralogical Characterizations of Soils Collected from the Deep Biosphere of the Former Homestake Gold Mine, South Dakota
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln US Department of Energy Publications U.S. Department of Energy 2010 Microbial and Mineralogical Characterizations of Soils Collected from the Deep Biosphere of the Former Homestake Gold Mine, South Dakota Gurdeep Rastogi South Dakota School of Mines and Technology Shariff Osman Lawrence Berkeley National Laboratory Ravi K. Kukkadapu Pacific Northwest National Laboratory, [email protected] Mark Engelhard Pacific Northwest National Laboratory Parag A. Vaishampayan California Institute of Technology See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/usdoepub Part of the Bioresource and Agricultural Engineering Commons Rastogi, Gurdeep; Osman, Shariff; Kukkadapu, Ravi K.; Engelhard, Mark; Vaishampayan, Parag A.; Andersen, Gary L.; and Sani, Rajesh K., "Microbial and Mineralogical Characterizations of Soils Collected from the Deep Biosphere of the Former Homestake Gold Mine, South Dakota" (2010). US Department of Energy Publications. 170. https://digitalcommons.unl.edu/usdoepub/170 This Article is brought to you for free and open access by the U.S. Department of Energy at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in US Department of Energy Publications by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors Gurdeep Rastogi, Shariff Osman, Ravi K. Kukkadapu, Mark Engelhard, Parag A. Vaishampayan, Gary L. Andersen, and Rajesh K. Sani This article is available at DigitalCommons@University of Nebraska - Lincoln: https://digitalcommons.unl.edu/ usdoepub/170 Microb Ecol (2010) 60:539–550 DOI 10.1007/s00248-010-9657-y SOIL MICROBIOLOGY Microbial and Mineralogical Characterizations of Soils Collected from the Deep Biosphere of the Former Homestake Gold Mine, South Dakota Gurdeep Rastogi & Shariff Osman & Ravi Kukkadapu & Mark Engelhard & Parag A. -
Patterns of Horizontal Gene Transfer Into the Geobacillus Clade
Imperial College London London Institute of Medical Sciences Patterns of Horizontal Gene Transfer into the Geobacillus Clade Alexander Dmitriyevich Esin September 2018 Submitted in part fulfilment of the requirements for the degree of Doctor of Philosophy of Imperial College London For my grandmother, Marina. Without you I would have never been on this path. Your unwavering strength, love, and fierce intellect inspired me from childhood and your memory will always be with me. 2 Declaration I declare that the work presented in this submission has been undertaken by me, including all analyses performed. To the best of my knowledge it contains no material previously published or presented by others, nor material which has been accepted for any other degree of any university or other institute of higher learning, except where due acknowledgement is made in the text. 3 The copyright of this thesis rests with the author and is made available under a Creative Commons Attribution Non-Commercial No Derivatives licence. Researchers are free to copy, distribute or transmit the thesis on the condition that they attribute it, that they do not use it for commercial purposes and that they do not alter, transform or build upon it. For any reuse or redistribution, researchers must make clear to others the licence terms of this work. 4 Abstract Horizontal gene transfer (HGT) is the major driver behind rapid bacterial adaptation to a host of diverse environments and conditions. Successful HGT is dependent on overcoming a number of barriers on transfer to a new host, one of which is adhering to the adaptive architecture of the recipient genome. -

C. T. Bauer College of Business
TY OF H SI O R U E S T V I O N N U f o 7 u 2 nded 19 C. T. Bauer College of Business Convocation Friday, December 18, 2015 OF HO Y US T T I O S N R E V I 7 N U 2 9 f 1 ounded Letter from the Dean Dear graduates, Today, you join the ranks of nearly 60,000 alumni of the C. T. Bauer College of Business. As you celebrate your graduation, know that your degree has great value. In fulfilling the requirements of your program, you have demonstrated not only your academic capability, but also the personal discipline and commitment necessary to complete such an educational endeavor. I personally congratulate you on this achievement. Bauer College is more than a degree-granting institution. Yes, to begin with, it is a college of business. On a bigger dimension, I firmly believe this is a place where we change lives and make a difference. We do this by helping our students learn, gain confidence, develop support networks and create opportunity for themselves and for others around them. I am very blessed to see this happen firsthand – to see you all learn, grow and succeed as you use the life skills you learn at Bauer – this is the best part of my job. I hope this convocation marks the beginning of a lifelong relationship with the Bauer College of Business, as well as a successful continued pursuit of your personal education and development. The Bauer faculty and staff are proud to join your family and friends in honoring your accomplishment. -
Isolation and Diversity of Sediment Bacteria in The
bioRxiv preprint doi: https://doi.org/10.1101/638304; this version posted May 14, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Isolation and Diversity of Sediment Bacteria in the 2 Hypersaline Aiding Lake, China 3 4 Tong-Wei Guan, Yi-Jin Lin, Meng-Ying Ou, Ke-Bao Chen 5 6 7 Institute of Microbiology, Xihua University, Chengdu 610039, P. R. China. 8 9 Author for correspondence: 10 Tong-Wei Guan 11 Tel/Fax: +86 028 87720552 12 E-mail: [email protected] 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 bioRxiv preprint doi: https://doi.org/10.1101/638304; this version posted May 14, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 29 Abstract A total of 343 bacteria from sediment samples of Aiding Lake, China, were isolated using 30 nine different media with 5% or 15% (w/v) NaCl. The number of species and genera of bacteria recovered 31 from the different media significantly varied, indicating the need to optimize the isolation conditions. 32 The results showed an unexpected level of bacterial diversity, with four phyla (Firmicutes, 33 Actinobacteria, Proteobacteria, and Rhodothermaeota), fourteen orders (Actinopolysporales, 34 Alteromonadales, Bacillales, Balneolales, Chromatiales, Glycomycetales, Jiangellales, Micrococcales, 35 Micromonosporales, Oceanospirillales, Pseudonocardiales, Rhizobiales, Streptomycetales, and 36 Streptosporangiales), including 17 families, 41 genera, and 71 species.