Report of the Independent Inquiry Into the Care and Treatment of Alexander
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Berkshire Echo 96
July 2021 l Abbey versus town l Hammer and chisel: Reading Abbey after the Dissolution l New to the Archives The Berkshire Echo WHAT’S ON From the Editor after a drawing by Paul Sandby (1731-1809) (D/EX2807/37/11) South ‘A Top: Prospect of the Abbey-Gate at Reading’, by Michael Angelo Rooker (c.1743-1801) Welcome to the Summer edition of the When the Abbey’s founder, Henry I, Where Smooth Waters Glide Berkshire Echo where we take a look died in Normandy in 1136, his body Take a look at our fantastic online into the history of Reading Abbey as was brought from there to be buried exhibition on the history of the River it celebrates its 900th anniversary in front of the high altar in the abbey Thames to mark 250 years of caring for this year. The abbey was founded in church. Unfortunately, as we discover the river at thames250exhibition.com June 1121 by Henry I and became one of in ‘Hammer and chisel’: Reading Abbey the richest and most important religious after the Dissolution, his coffin was institutions of medieval England. not handled very well later in the Pilgrims travelled to Reading to see nineteenth century. the hand of St James, a relic believed But how did it come to pass that the to have miraculous powers. The abbey resting place of a Royal was treated also has a place in the history of both this way? Well, it stems from another music and the English language, as royal – Henry VIII. After declaring it is believed to be the place where himself the Supreme Head of the the song ‘Summer is icumen in’ was Church of England in 1534, Henry VIII composed in the 13th century – the first disbanded monasteries across England, known song in English. -
RRH Orts Leaflet for Website:Layout 1
vealing Reading’s PRUDENTIAL INSURANCE COMPANY, KINGS ROAD Hidden History Take a closer look at YOUR RUPERT SQUARE local heritage... Orts Road & Newtown KENNETSIDE Pen & ink drawings of local landmarks by Kate Lockhart, commissioned as part of the Happy Museum project and added to Reading Museum’s permanent art collection in 2013 Visit Reading Museum at the Town Hall on Blagrave Street (behind Marks & Spencers) Admission is FREE! Opening hours: Tuesday to Saturday - 10am to 4pm Sunday and Bank Holiday Mondays - 11am to 4pm (Closed on Mondays except on Bank Holidays and during school half-terms) www.readingmuseum.org.uk ‘Revealing Our Hidden History’ is supported by Reading Neighbourhood Action Groups (NAGs). Funded by the Happy Museum project. Researched and compiled with the assistance of local residents. This leaflet is printed onto FSC Paper. The demanding standards of the FSC (Forestry Stewardship Council)® mean that every sheet of paper can be traced back to its source ensuring the responsible husbandry of forests. The Early History of the Orts Road Roman: and Newtown area: Reading’s proximity to the land- The fast flowing waters of the rivers Thames and Kennet meet at the locked town of Silchester has led to eastern end of Reading, shaping natural gravel terraces upon which early the conclusion that Reading served as nomadic people found dry land and established primitive an inland port for the Romans. The dwellings. Rivers Thames and Kennet must have been a trade route for Archaeological excavations in the area have unearthed the imported goods evidence of human activity dating back to this excavated there. -

Historic Places Panel Review Paper Reading Town Centre 2020: Abbey Quarter, Minster Quarter and Oxford Road Historic Places Panel Review Paper: Reading 2020
Historic Places Panel Review Paper Reading Town Centre 2020: Abbey Quarter, Minster Quarter and Oxford Road Historic Places Panel Review Paper: Reading 2020 Contents 1. Introduction ................................................................................................... 2 Key questions for the panel ................................................................................ 3 Other questions .................................................................................................. 4 2. Initial Observations ........................................................................................ 5 3. The Abbey Ruins and Prison area .................................................................... 7 4. The Castle Street/St Mary Butts Conservations Area ....................................... 9 5. Oxford Road from the Inner Distribution Road (IDR) in the east to the Reading West Railway Bridge ...................................................................... 11 6. Other Matters ............................................................................................... 13 The Heritage Action Zone ...................................................................................13 Reading Economic Forum: 2050 Vision ...............................................................13 The Lido .............................................................................................................14 7. Conclusions and Recommendations ............................................................. 15 8. Recommendations -

Easter 2021 Bank Holiday Pharmacy Opening Hours: Berkshire West
Easter 2021 Bank Holiday Pharmacy Opening Hours: Berkshire West The pharmacies listed below should be open as shown. The details are correct at the time of publishing but are subject to change. You are advised to contact the pharmacy before attending to ensure they are open and have the medication you require. Details of local pharmacies can also be found by scanning the code opposite or by visiting www.nhs.uk Good Friday Easter Sunday Easter Monday Town Pharmacy Name Address Phone Number 2nd April 2021 4th April 2021 5th April 2021 Reading Tesco Pharmacy Tesco Extra, Portman Road, Reading, Berkshire, RG30 1AH 09450 269558 08:00-21:00 Closed 09:00-18:00 Reading Asda Pharmacy Chalfont Way, Lower Earley, Reading, Berkshire, RG6 5TT 01189 9870300 09:00-18:00 Closed 09:00-18:00 Unit 7, Brunel Arcade, Reading Mainline Station, Reading, Reading Boots the Chemists 01189 591523 09:00-16:00 Closed Closed Berkshire, RG1 1LT Lloydspharmacy (in Savacentre, Bath Road, Calcot, Reading, Berkshire, RG31 Reading 01189 382265 10:00-16:00 Closed 10:00-16:00 Sainsbury) 7SA Reading Tilehurst Pharmacy 7 School Road, Tilehurst, Reading, Berkshire, RG31 5AR 01189 427353 Closed 14:00-17:00 Closed Reading Superdrug Pharmacy 55-59 Broad Street, Reading, Berkshire, RG1 2AF 01189 599772 08:00-18:00 Closed Closed 89-91 Crockhamwell Road, Woodley, Reading, Berkshire, Reading Boots the Chemists 01189 695253 10:00-16:00 Closed 10:00-16:00 RG5 3JP Reading Tesco Pharmacy Tesco Extra, Napier Road, Reading, Berkshire, RG1 8DF 01189 904507 06:30-22:30 Closed 09:00-18:00 Reading Asda Pharmacy Honey End Lane, Reading, Berkshire, RG30 4EL 01189 514710 09:00-18:00 Closed 09:00-18:00 Your Local Boots Unit 2,Asda Mall, Lower Earley District Ctr, Lower Earley, Reading 01189 311750 11:00-18:00 Closed 11:00-18:00 Pharmacy Reading, Berkshire, RG6 5GA Mortimer Mortimer Pharmacy 72 Victoria Road, Mortimer, Reading, Berkshire, RG7 3SQ 01189 333161 Closed 10:00-17:00 Closed Easter 2021 Bank Holiday Pharmacy Opening Hours: Berkshire West Cont.. -

Getting to the Royal Berkshire Hospital
Tel: 0118 322 5111 Web: www.royalberkshire.nhs.uk Web: 5111 322 0118 Tel: London Road, Reading RG1 5AN RG1 Reading Road, London Royal Berkshire NHS Foundation Trust Foundation NHS Berkshire Royal July 2006 July service information Patient www.busbook.co.uk Thames Travel: 01491 837988 837988 01491 Travel: Thames www.reading-buses.co.uk Reading Transport: 0118 959 4000 4000 959 0118 Transport: Reading www.traveline.org.uk Traveline Public Transport Information: 0870 608 2608 608 0870 Information: Transport Public Traveline Further information is available from available is information Further Craven Road. Craven N2a NightTrack from Reading to Woodley via via Woodley to Reading from NightTrack Craven Road Craven N3 NightTrack from Lower Earley to Reading via via Reading to Earley Lower from NightTrack Redlands Road (Thames Travel) (Thames Road Redlands Royal Berkshire Hospital Berkshire Royal 144 Reading to Wokingham via Craven Road and and Road Craven via Wokingham to Reading Redlands Road Redlands Getting to the the to Getting 42 Reading to Woodley via Craven Road and and Road Craven via Woodley to Reading 28 Redlands Road to Reading, Grovelands and Tilehurst and Grovelands Reading, to Road Redlands Reading station Reading 18 Lower Earley to Calcot via RBH South block and and block South RBH via Calcot to Earley Lower Road and Redlands Road Redlands and Road 9 Caversham Heights to Whitley Wood via Craven Craven via Wood Whitley to Heights Caversham Reading town centre town Reading A number of buses travel between the hospital and and hospital the between travel buses of number A Travelling by bus by Travelling Car parking Park & Ride During peak periods on weekdays, there is often difficulty During peak periods on weekdays, there are many finding a parking space. -

Reading Abbey Revealed Conservation Plan August 2015
Reading Abbey Revealed Conservation Plan August 2015 Rev A First Draft Issue P1 03/08/2015 Rev B Stage D 10/08/2015 Prepared by: Historic Buildings Team, HCC Property Services, Three Minsters House, 76 High Street, Winchester, SO23 8UL On behalf of: Reading Borough Council Civic Offices, Bridge Street, Reading RG1 2LU Conservation Plan – Reading Abbey Revealed Contents Page Historical Timeline ………………………………………………………………………………. 1 1.0 Executive Summary……………………………………………………………………………… 2 2.0 Introduction ………………………………………………………………………………………. 3 3.0 Understanding the Heritage 3.1 – Heritage Description ……………………………………………………………………… 5 3.2 – History ……………………………………………………………………………………… 5 3.3 – Local Context ……………………………………………………………………………… 19 3.4 – Wider Heritage Context ………………………………………………………………….. 20 3.5 – Current Management of Heritage ………………………………………………………. 20 4.0 Statement of Significance 4.1 – Evidential Value ………………………………………………………………………….. 21 4.2 – Historical Value …………………………………………………………………………... 21 4.3 – Aesthetic Value …………………………………………………………………………… 21 4.4 – Communal Value …………………………………………………………………………. 22 4.5 - Summary of Significance ………………………………………………………………... 24 5.0 Risks to Heritage and Opportunities 5.1 – Risks ………………………………………………………………………………………. 26 5.2 – Opportunities ……………………………………………………………………………… 36 6.0 Policies 6.1 – Conservation, maintenance and climate change …………………………………….. 38 6.2 – Access and Interpretation ……………………………………………………………….. 39 6.3 – Income Generation ………………………………………………………………………. 40 7.0 Adoption and Review 7.1 – General Approach -

Where They Have Buy to Let Mortgages. Check What to Do If You Can't Pay Your Rent Because of Coronavirus
These sites support Parents and Children with SEND – updated 27th April 2020 Me2 Club support young people aged 5-19 with additional needs and disabilities to take part in mainstream after school activities. They now support in; Abbey, Battle, Church, Katesgrove, Minster, Norcot, Park, Redlands, Southcote and Whitley wards. They would like to let everyone know that although they are not currently able to get young people started at activities with volunteers, their waiting list is still very much open and they are still accepting applications, ready to get going again as soon as it is safe to do so. For full details visit: https://me2club.org.uk/about-us/ Parenting Special Children have developed three 90 minute online linked workshops to support families of children with SEND during the Covid-19 lockdown. They have two series running, one starting in April and one starting in May (each series contains the same information). Series One: Mondays: 20th and 27th April, 4 May: 7:30pm - 9pm https://www.eventbrite.co.uk/e/understanding-supporting-childrens-behaviour-during-the-covid-19- lockdown-registration-102796182148 Series Two: Mondays: 11th, 18th and 25th May: 7:30pm - 9pm https://www.eventbrite.co.uk/e/understanding-supporting-childrens-behaviour-during-the-covid-19- lockdown-registration-102883619676 Cost: Free for families with children living, or attending a school, in Berkshire (£5 refundable booking deposit). The local Charity Stepping Forward can help with Benefits Advice - including DLA, PIP, Carers Allowance and Universal Credit applications. If you are a disabled person, or you are supporting someone with a disability, we can help with Benefits Advice - including DLA, PIP, Carers Allowance and Universal Credit applications. -

Your Friendly Village Newsletter
Your Friendly Village Newsletter Issue Number 94 : July 2008 ISSN 1755-9502 (Print) : ISSN 1755-9510 (Online) MINSTER FLOWER SHOW Saturday 19th July Recreation Ground This year marks the staging of the 122nd Logo designed by Michaela Hockley Annual Flower Show in the village and the Committee are pleased to announce that they have ABBEY PLANNING APPLICATION been able to acquire the services of Ben Mills, of (Parkminster - Former Museum Site) X-Factor fame, to ‘do the honours’ and officially We were requested by the Abbey Trustees not to open the show at 2.00pm. add an editorial comment, to the notice we Apart from the usual offerings of exhibits and published for them last month, regarding the competitions in the granting of the change of use of the former Museum Barn and surrounding area. marquee, you will However, since then, the following has come to also be entertained by our notice, and we feel it is our duty to report that both a “Baby Show” the Thanet District Council Planning Committee and a “Dog Show” has applied the following conditions to that alongside of which application: there will be a variety “No use other than non-residential of races for children hospitality use, as specified by information and adults alike and submitted by the applicant on 12 March 2008 Minster Mayhems entitled 'Hospitality at Minster Abbey', shall be will be there complete carried on at the site, and the approved use shall with their Maypole. be carried on only by Mother Nikola Kroksch, A skateboard competition for the 8 to 18 yr olds Sister Benedict Gaughan, Sister Aelred Erwin is being staged at the skate-park area plus for and Sister Johanna Caton (hereinafter referred everyone’s enjoyment you can look forward to a to as the Trustees of Minster Abbey) and by no good variety of stalls, a fun fair and a music other person or persons. -

Tewkesbury Abbey Fine and Almost
Tewkesbury Abbey Fine and almost complete example of a Romanesque abbey church Pre-dates Reading. Dedicated in 1121, the year of Reading’s foundation. Look out for anniversary events at Tewksbury in 2021. But some important and interesting links to Reading Both were Benedictine Founder Robert Fitzhamon (honour of Gloucester), friend of Rufus, supported against Robert Curthose. At his death in the New Forest. Then loyal to Henry I – campaigned in Normandy against supporters of Curthose and died doing so in 1107. Fitzhamon’s heiress Mabel married Robert of Gloucester d 1147, the first and most favoured illegitimate son of Henry I, who was a key supporter of his half sister Matilda Granddaughters were coheiresses – but one of them Hawise (or Isabella of Gloucester) married Prince John. Despite annulment, Tewksbury became a royal abbey Later passed to the de Clares. Earls of Gloucester and Hereford. And made their mausoleum Richard III de Clare (grandson) married Joan of Acre, daughter of Edward I Again co heiresses in the early 14th C. the eldest Eleanor married Hugh Despenser the younger, favourite of Edward II, executed 1326. She is instrumental in making Tewksbury into a Despenser mausoleum (significant rebuilding and splendid tombs) Her great grandson Thomas Despenser marries Constance of York granddaughter of Ed III. A strong link with Reading abbey here as she was buried there in 1416 The Despenser line also ended up with an heiress Isabella who married in turn two men called Richard Beauchamp, the first Richard Beauchamp lord Abergavenny a great friend of Henry V who created him earl of Worcester: but Richard died in the French wars in March 1422; and then his half cousin Richard Beauchamp earl of Warwick, also prominent in the wars in France. -
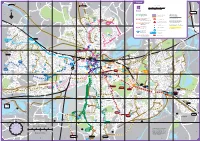
Reading Cycle Routes Networ
T Legend W Y F 1 O 8 R R A B C D 4 E F H D O D Pangbourne B A W E O V R L R I Goring, Streatley ROKEBY DRIVE A N Scale 1:22,000 R Oxford O L I N D Y K E A PH E IL E N A 5 Wallingford LIMORE R A N D V L W D A O KI H C D D D D TOWER R C N CLOS A O U E E D M H H A O 0 250m 500m 750m 1 kilometre C D O 4 U O W W S L H O 0 R F R C N O A T 7 E R C R U R A O XH H 4 E H D G N E I M K S L R D O L L E I P D R R E L A A R D O A A L N V A R S L D E E R G T L G E K A A N E S R L S R IL P 0 ¼ mile ½ mile DR H U Y E O HA S A P E R S RO C W R A E RA R K C P D N A R W E Reading O L S W A P H D N A A PE Cycle Routes THAMES Y L E 5 N O JEFFERSON CL A Wargrave D P R N R P N E A 4 L Eton RD I RIVE K D ENAY RT R London OU B C D U B K R R N I O D H M A O South Reading M H E K O V I L R I I G Y R S 1 R 1 E Cycle Facilities Key N E H E Town Centre Route V A Madejski Stadium I D R D D E S R F E N O N HIGHDOWN AV O H D (for all route colours) O X W C & Whitley H D MAPLEDURHAM N R I O L D E O Y P H R E WA C L O I H V Linking Route L O A L S L V E L H I L L I A R L V E A C ALG V Caversham L I E A CH E Work in ProgressR A R D R L A F G G V E S Park Primary W R H St Martin's R N L E L A S W AS School S M D A Primary E T P UEEN W R O EMMER AR Q Y A O E M K R School N D I G R ALL W A N OR South-East Reading R O O A T Y H G D C E A A Traffic-free cycle route G R V V A A OL K R BE D E R A V Y R E E I B A D S M GREEN H V D G A E Y K R N E N E U AYS E A M R L N RO TI I R O R Y R & Wokingham A National Cycle Path L W L R A S I A O A B NG S O S Y T S OD W R C P VE 4 N Emmer -

FOR SALE Rare Freehold Opportunity
FOR SALE Sui Generis Rare Freehold Opportunity Police Box, Corwen Road, School Road, Tilehurst, Berkshire RG30 4TA 240 Sq Ft (22.30 Sq M) Approximately 107 sq ft (9.94 sq m) Site area 0.006 acres (0.002 hectares) Small freehold opportunity Suitable for other uses (subject to planning) Lambert Smith Hampton Midland House, West Way, Botley, Oxford, Oxfordshire OX2 0PH T: 01865 200 244 Police Box, Corwen Road, School Road, Tilehurst, Berkshire RG30 4TA ACCOMMODATION Schedule of Areas sq ft sq m Total 240 22.3 VAT All prices, premiums and rents, etc are quoted exclusive of VAT at the prevailing rate. LEGAL COSTS Each party to be responsible for their own legal costs incurred in any transaction. BUSINESS RATES TBC LOCATION TERMS The Box is located in Tilehurst, approximately 3.5 miles west of The agents will be inviting offers for the freehold purchase of this Reading town centre. The property is located on Corwen Road that site by a date to be confirmed. links directly to Tilehurst's High street named School Road. The High Street provides a good range of local shopping facilities including Unconditional offers are preferred, however those subject to planning national and local occupiers such as Nationwide, The Cooperative and will be considered. Those that are subject to planning will need to Dominos. include details of the development proposals upon which the offer is based. Tilehurst has good provision for public transport with Reading Train ENERGY PERFORMANCE CERTIFICATE Station, approximately a 15 minutes walk serving direct lines to London and Exeter. Road services are also very good with the M4 TBC motorway easily accessible via Junction 12 approximately 2.5 miles away. -
Completely Reading. Completely Reading
Barclay Road, Calcot, Reading , RG31 7EL £37 555,,,000000 000 Freehold Completely Reading. • Excellent Decorative Order • Cul-De-Sac Location • Three Bedrooms • Convenient Access To M4 Junction 12 • 19' Kitchen/Breakfast Room • Delightful Rear Garden • Off Road Parking • Gas Radiator Central Heating, Double Glazing • Excellent Family Home • Council Tax Band D Offered to the market in excellent decorative order is this semi -detached house conveniently located giving excellent access to M4 Junction 12, Reading town centre and local amenities. The good size accommodation includes three bedrooms with en-suite to master plus family bathroom, 17' lounge, downstairs WC, family room and storage area (garage conversion) and 19' kitchen/breakfast room. To the rear is a well maintained garden and to the front off road parking for several vehicles. This property would make an excellent first time buy or family home and viewings are highly recommended. The Agent has not tested any apparatus, fittings or services and Tilehurst Office so cannot verify they are in working order. In the case of an extension, conversion or double glazing, the Agent has not 152 Park Lane, Tilehurst, Reading, verified any planning consents, building regulation approval or FENSA certification that may be required. On these matters you Berkshire, RG31 4DU are advised to obtain verification from your solicitor or surveyor. Living in a designated school catchment area does not guarantee T: 0118 942 0600 a school place, we advise consulting the Local Authority and E: [email protected] school. Lower Earley Office 0118 931 0011 Tilehurst Office 0118 942 0600 Woodley Office 0118 969 7000 Lettings 0118 935 1004 [email protected] [email protected] [email protected] [email protected] whiteknights.co.uk Earley Office 0118 966 8655 Reading Office 0118 986 8888 Spencers Wood Office 0118 988 2011 Property Management 0844 682 2101 [email protected] [email protected] [email protected] [email protected] .