Chapter 26: the Urinary System an Overview of the Urinary System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Renal Vascular System of the Monkey: a Gross Anatomical Description MARK J
J. Anat. (1987), 153, pp. 123-137 123 With 8 figures Printed in Great Britain The renal vascular system of the monkey: a gross anatomical description MARK J. HORACEK, ALVIN M. EARLE AND JOSEPH P. GILMORE Departments ofAnatomy and Physiology and Biophysics, University of Nebraska College of Medicine, Omaha, Nebraska 68105, U.S.A. (Accepted 12 September 1986) INTRODUCTION Monkeys are frequently used as a model for physiological experiments involving the kidney. It is known that physiological disparity between mammalian species can often be elucidated by a study of the structural differences between these species. Despite this fact, the monkey's renal vasculature has not been described in sufficient detail. Such a description would be useful since monkey experimentation plays an important role in understanding human physiology. Also, the branching pattern and segmen- tation of the monkey's renal vasculature is interesting from both comparative and experimental viewpoints. Fourman & Moffat (1971) indicated that although all mammalian kidneys are somewhat similar, there are several species-specific differences in terms oforganisation, microstructure and function. They conducted several extensive vascular studies on mammals, including several rodents and carnivores, but did not include any specific information concerning the monkey. Graves (1971) and Fine & Keen (1966) have described the branching patterns and segmentation of human kidneys. However, comparable information pertaining to the monkey kidney is not available. The purpose of the present study is to provide a detailed morphological description of the gross renal vasculature in the kidneys of two species of monkeys, Macacafascicularis and Macaca mulatta. MATERIALS AND METHODS Twelve monkeys (Macacafascicularis and Macaca mulatta) were used in this study after they had been utilised for electrophysiological experimentation. -

Anatomy and Physiology of the Bowel and Urinary Systems
PMS1 1/26/05 10:52 AM Page 1 Anatomy and Physiology of the Bowel and 1 Urinary Systems Anthony McGrath INTRODUCTION The aim of this chapter is to increase the reader’s under- standing of the small and large bowel and urinary system as this will enhance their knowledge base and allow them to apply this knowledge when caring for patients who are to undergo stoma formation. LEARNING OBJECTIVES By the end of this chapter the reader will have: ❏ an understanding of the anatomy and physiology of the small and large bowel; ❏ an understanding of the anatomy and physiology of the urinary system. GASTROINTESTINAL TRACT The gastrointestinal (GI) tract (Fig. 1.1) consists of the mouth, pharynx, oesophagus, stomach, duodenum, jejunum, small and large intestines, rectum and anal canal. It is a muscular tube, approximately 9m in length, and it is controlled by the autonomic nervous system. However, while giving a brief outline of the whole system and its makeup, this chapter will focus on the anatomy and physiology of the small and large bowel and the urinary system. The GI tract is responsible for the breakdown, digestion and absorption of food, and the removal of solid waste in the form of faeces from the body. As food is eaten, it passes through each section of the GI tract and is subjected to the action of various 1 PMS1 1/26/05 10:52 AM Page 2 1 Anatomy and Physiology of the Bowel and Urinary Systems Fig. 1.1 The digestive system. Reproduced with kind permission of Coloplast Ltd from An Introduction to Stoma Care 2000 2 PMS1 1/26/05 10:52 AM Page 3 Gastrointestinal Tract 1 digestive fluids and enzymes (Lehne 1998). -
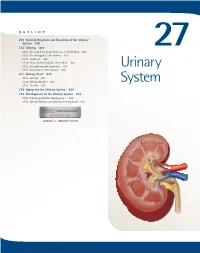
Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -
The Urinary System Dr
The urinary System Dr. Ali Ebneshahidi Functions of the Urinary System • Excretion – removal of waste material from the blood plasma and the disposal of this waste in the urine. • Elimination – removal of waste from other organ systems - from digestive system – undigested food, water, salt, ions, and drugs. + - from respiratory system – CO2,H , water, toxins. - from skin – water, NaCl, nitrogenous wastes (urea , uric acid, ammonia, creatinine). • Water balance -- kidney tubules regulate water reabsorption and urine concentration. • regulation of PH, volume, and composition of body fluids. • production of Erythropoietin for hematopoieseis, and renin for blood pressure regulation. Anatomy of the Urinary System Gross anatomy: • kidneys – a pair of bean – shaped organs located retroperitoneally, responsible for blood filtering and urine formation. • Renal capsule – a layer of fibrous connective tissue covering the kidneys. • Renal cortex – outer region of the kidneys where most nephrons is located. • Renal medulla – inner region of the kidneys where some nephrons is located, also where urine is collected to be excreted outward. • Renal calyx – duct – like sections of renal medulla for collecting urine from nephrons and direct urine into renal pelvis. • Renal pyramid – connective tissues in the renal medulla binding various structures together. • Renal pelvis – central urine collecting area of renal medulla. • Hilum (or hilus) – concave notch of kidneys where renal artery, renal vein, urethra, nerves, and lymphatic vessels converge. • Ureter – a tubule that transport urine (mainly by peristalsis) from the kidney to the urinary bladder. • Urinary bladder – a spherical storage organ that contains up to 400 ml of urine. • Urethra – a tubule that excretes urine out of the urinary bladder to the outside, through the urethral orifice. -

Normal Vascular and Glomerular Anatomy
Normal Vascular and Glomerular Anatomy Arthur H. Cohen Richard J. Glassock he topic of normal vascular and glomerular anatomy is intro- duced here to serve as a reference point for later illustrations of Tdisease-specific alterations in morphology. CHAPTER 1 1.2 Glomerulonephritis and Vasculitis FIGURE 1-1 A, The major renal circulation. The renal artery divides into the interlobar arteries (usually 4 or 5 divisions) that then branch into arcuate arteries encompassing the corticomedullary Interlobar junction of each renal pyramid. The interlobular arteries (multiple) originate from the artery arcuate arteries. B, The renal microcirculation. The afferent arterioles branch from the interlobular arteries and form the glomerular capillaries (hemi-arterioles). Efferent arteri- Arcuate oles then reform and collect to form the post-glomerular circulation (peritubular capillar- artery Renal ies, venules and renal veins [not shown]). The efferent arterioles at the corticomedullary artery junction dip deep into the medulla to form the vasa recta, which embrace the collecting tubules and form hairpin loops. (Courtesy of Arthur Cohen, MD.) Pyramid Pelvis Interlobular Ureter artery A Afferent arteriole Interlobular artery Glomerulus Arcuate artery Efferent arteriole Collecting tubule Interlobar artery B Normal Vascular and Glomerular Anatomy 1.3 FIGURE 1-2 (see Color Plate) Microscopic view of the normal vascular and glomerular anatomy. The largest intrarenal arteries (interlobar) enter the kidneys between adjacent lobes and extend toward the cortex on the side of a pyramid. These arteries branch dichotomously at the corti- comedullary junction, forming arcuate arteries that course between the cortex and medulla. The arcuate arteries branch into a series of aa ILA interlobular arteries that course at roughly right angles through the cortex toward the capsule. -

The Distal Convoluted Tubule and Collecting Duct
Chapter 23 *Lecture PowerPoint The Urinary System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Urinary system rids the body of waste products. • The urinary system is closely associated with the reproductive system – Shared embryonic development and adult anatomical relationship – Collectively called the urogenital (UG) system 23-2 Functions of the Urinary System • Expected Learning Outcomes – Name and locate the organs of the urinary system. – List several functions of the kidneys in addition to urine formation. – Name the major nitrogenous wastes and identify their sources. – Define excretion and identify the systems that excrete wastes. 23-3 Functions of the Urinary System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm 11th and 12th ribs Adrenal gland Renal artery Renal vein Kidney Vertebra L2 Aorta Inferior vena cava Ureter Urinary bladder Urethra Figure 23.1a,b (a) Anterior view (b) Posterior view • Urinary system consists of six organs: two kidneys, two ureters, urinary bladder, and urethra 23-4 Functions of the Kidneys • Filters blood plasma, separates waste from useful chemicals, returns useful substances to blood, eliminates wastes • Regulate blood volume and pressure by eliminating or conserving water • Regulate the osmolarity of the body fluids by controlling the relative amounts of water and solutes -

Anatomy of the Kidney
Anatomy of the kidney Renal block-Anatomy-Lecture 1 Editing file Color guide : Only in boys slides in Green Objectives Only in girls slides in Purple important in Red Notes in Grey By the end of this course you should be able to discuss : ● Components of the urinary system ● Kidney : 1. Shape & Position 2. Surface anatomy 3. External features 4. Hilum & its contents 5. Relation 6. Internal features 7. Blood supply 8. Lymph drainage 9. Nerve supply Introduction 3 ● Every day, each kidney filters liters (around 150 L per day ) of fluid from the bloodstream. ● Although the lungs and the skin also play roles in excretion, The kidneys bear the major responsibility for eliminating nitrogenous (nitrogen-containing) wastes, toxins, and drugs from the body. Excretes most of the Maintain acid-base waste products of balance of the blood. metabolism. By Erythropoietin Controls hormone stimulates Function of water & electrolyte bone marrow for RBCs kidney balance of the body. formation. Converts By Rennin vitamin D to its enzyme regulates active form. the blood pressure. The kidney : ● Kidneys are reddish brown in color. 4 ● Lie behind the peritoneum (retroperitoneal) on the posterior abdominal wall on either side of the vertebral column. ● They are largely under cover of the costal margin. kidney lies between T12-L3 ● With contraction of the diaphragm (during inspiration) the kidney moves downward as much as 2.5 cm. T12 Comparison between : L3 Right kidney Left kidney Anterior view lies slightly lower than the left due Location to the large size of the right lobe of Upper than the right the liver. -

Urinary System
Urinary system Sándor Katz M.D.,Ph.D. Urinary system - constituents • kidneys • ureters • urinary bladder • urethra Kidney Weight: 130-140g Kidneys - location 1. On the posterior body wall 2. Posterior to parietal peritoneum – retroperitoneal organ 3. At the level of T12-L2 (left kidney) and L1-L3 (right kidney) Kidneys - location Kidneys – covering structures 1. Renal (Gerota’s) fascia 2. Adipose capsule 3. Fibrous capsule Kidneys - neighbouring organs and structures Kidney – gross anatomy External structures: Hilum of kidney: 1. Renal vein 2. Renal artery 3. Ureter Internal structures: 1. Cortex 2. Medulla 3. Minor calyces 4. Major calyces 5. Renal pelvis Renal cortex Renal columns (Bertini’s columns) Renal medulla – renal pyramids A p p r o x i m a t e l y 3 0 pyramids are in each kidney and many of them are fused together. renal papilla Minor calyces 8-9 in each kidney Major calyces Approx. 3 in each kidney Renal pelvis Renal hilum - L1/L2 level renal sinus From anterior to posterior direction: 1. renal vein 2. renal artery 3. ureter From superior to inferior direction: 1. renal artery 2. renal vein 3. ureter Renal arteries - L1 level Renal artery • segmental arteries • interlobar arteries • arcuate arteries • interlobular arteries • afferent arterioles Renal veins left renal vein is longer than the right one and crosses over the aorta Renal veins right renal vein left renal vein is longer than the right one and crosses over the aorta left renal vein Tributaries of the renal veins • (stellate veins – only under the fibrous capsule) • interlobular veins • arcuate veins • interlobar veins • segmental veins Renal veins left suprarenal vein (empties into the left renal vein) left gonadal (testicular or ovarian) vein (empties into the left renal vein) The right suprarenal and gonadal veins empty into the IVC. -

Download Article
Advances in Health Sciences Research, volume 16 International Conference on Health and Well-Being in Modern Society (ICHW 2019) Level Organization of the Venous Bed of the Human Kidney Depending on the Options and Types of Intraorgan Veins Fusion Kafarov E.S. Fedorov S.V. Chechen State University Bashkir State Medical University of the Ministry of Health Grozny, Russia of Russia [email protected] Ufa, Russia [email protected] Khidiyatov I.I. Nasibullin I.M. Bashkir State Medical University of the Ministry of Health Bashkir State Medical University of the Ministry of Health of Russia of Russia Ufa, Russia Ufa, Russia [email protected] [email protected] Galimzyanov V.Z. Bashkir State Medical University of the Ministry of Health of Russia Ufa, Russia [email protected] Abstract – The article aims to conduct a 3D analysis of links organization of the intraorgan venous bed of the human and levels of the intraorgan venous system of the human kidney kidney. These links and levels of the venous system of the and build a model of its levels and spatial hierarchy. 46 corrosive kidney are distributed from the periphery of the organ to the preparations of the renal venous system were produced. The renal vein: vv. Stellatae -, vv. Interlobares, – vv. Arcuatae, – preparations were subjected to 3D scanning. Using Mimics-8.1, vv. Interlobares II, – Interlobares I, – vv. Renales III, – vv. options and types of fusion of intraorgan venous vessels of the renales II, – vv. Renales I, – seu v. Renalis [14]. However, kidneys were studied. The 3D stereo-anatomical analysis of the many researchers did not agree with this scheme. -
Lecture (1) Urinary System
UrinaryUrinaryUrinary systemsystemsystem Dr. Carmen E. Rexach Anatomy 35 Mt. San Antonio College Functions •Storage of urine – Bladder stores up to 1 L of urine • Excretion of urine – Transport of urine out of body • Blood volume regulation – Effects of hormones on kidneys • Regulation of erythrocyte production –Kidneys • Monitor oxygen content of blood • Produce EPO = erthrocyte production Components •Kidneys • Ureters • Urinary Bladder • Urethra Kidneys Gross Anatomy • Kidneys approx weight = 125- 150g each • Retroperitoneal – Anterior surface covered with peritoneum – Posterior surface directly against posterior abdominal wall • Superior surface at about T12 • Inferior surface at about L3 • ureters enter urinary bladder posteriorly • Left kidney 2cm superior to right –Size of liver Transverse section at L1 surface features of kidney • Hilum = the depression along the medial border through which several structures pass –renal artery –renal vein –ureter – renal nerves Surrounding structures • Fibrous capsule – Innermost layer of dense irregular CT – Maintains shape, protection • Adipose capsule (perinephric fat) – Adipose ct of varying thickness – Cushioning and insulation • Renal fascia – Dense irregular CT – Anchors kidney to peritoneum & abdominal wall • Paranephric fat – Outermost, adipose CT between renal fascia and peritoneum Coronal section •Cortex – layer of renal tissue in contact with capsule –Lighter shade –Renal columns= parts of cortex that extend into the medulla between pyramids •Medulla –Innermost – striped due to renal tubules •renal pyramids – 8-15 present in medulla of adult – conical shape – Wide base at corticomedullary junction Coronal section • Renal pelvis – collects from calyces, passes onto ureter •Calyces (pl) – funnel shaped regions – collect urine into pelvis •Minor calyx (s) – in contact with each pyramid •Major calyx (s) – collect from minor Microscopic Anatomy Microscopic anatomy Renal tubules • Nephron – functional unit of the kidney. -

Effects of Acute, Angiotensin-Induced Hypertension on Intrarenal Arteries in the Rat
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Kidney International, Vol. 25 (1984), pp. 492—501 Effects of acute, angiotensin-induced hypertension on intrarenal arteries in the rat STEPHEN K. WILSON and ROBERT H. HEPTINSTALL Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, Maryland Effects of acute, angiotensin-induced hypertension on intrarenal arter- constriction artérielle, et que les lesions vasculaires hypertensives ies in the rat. A perfusion-fixation and vascular casting technique was associCes a une permCabilitC accrue se produisent exclusivement dans used to assess the effects of acute, angiotensin-induced hypertension on les zones non constrictées. the intrarenal arteries and, for comparison, the small arteries of the intestine. The first objective was to establish that the technique accurately preserves postmortem the vascular changes induced by Most information on the reaction of small arteries to acute acute hypertension. To do this, the easily accessible intestinal arteries hypertension is derived from studies on small intestinal and were examined and photographed both in vivo and after fixation and mesenteric vessels. In response to angiotensin-induced hyper- injection of Batson's no. 17 casting resin in a group of angiotensin- tension, the intestinal arteries develop alternating zones of treated rats and controls. The second objective was to apply the technique to observe and compare acute hypertensive changes in the constriction and nonconstriction; moreover the nonconstricted intrarenal and intestinal arteries; studies included scanning electron zones, but not the constricted regions, become unduly perme- microscopy of vascular casts and transmission electron microscopy of able and manifest signs of medial smooth muscle injury [1—6]. -

The Urinary System Consists of Kidneys, Ureters, Urinary Bladder
Anatomy Lecture Notes Chapter 23 the urinary system consists of kidneys, ureters, urinary bladder, and urethra the function of the kidneys is NOT "to make urine" the kidneys: 1) regulate water balance 2) regular ECF electrolyte levels (Na, K, Ca) 3) eliminate some metabolic wastes urine is a by-product of these functions A. kidneys 1. located against posterior abdominal wall (retroperitoneal) T11 or T12 to L3 right kidney lower than left kidney 2. surrounded by a. pararenal fat (posterior only) b. renal fascia c. adipose capsule - perirenal fat d. renal capsule - dense c.t. covering surface of kidney e. parietal peritoneum Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 3. layers a. cortex - contains renal corpuscles and extends inwards as renal columns b. medulla - consists of renal pyramids which consist mostly of collecting ducts papilla - apex of renal pyramid; where collecting ducts drain into calyx 4. cavities and associated structures a. renal sinus - space in medial part of kidney; contains renal pelvis b. renal pelvis - expanded superior part of ureter minor calyx collects urine from one renal papilla major calyx formed by junction of 2 or more minor calyces renal pelvis formed by junction of all major calyces Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 5. renal hilum - medial indentation; where ureter leaves kidney 6. blood flow through the kidney - renal fraction = 20% of cardiac output aorta renal artery segmental arteries lobar arteries interlobar arteries arcuate arteries cortical radiate (interlobular) arteries afferent arterioles glomerular capillaries (glomerulus) efferent arteriole peritubular capillaries and vasa recta cortical radiate (interlobular) veins arcuate veins interlobar veins renal vein inferior vena cava Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 7.