July 2018 Ijabms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S.No. Name of Ethics Committee RC No
S.No. Name of Ethics Committee RC No. Address State All India Institute of Medical Sciences, Room No.102, 1st floor, OT Block, 1 Ethics Committee ECR/538/Inst/DL/2014/RR-17 Delhi Ansari Nagar, New Delhi-110029 Aster Aadhar Hospital, R.S. NO. 628, 'B' Ward, Near Shastri Nagar, KMT 2 Aster Aadhar Ethics Committee ECR/470/Inst/MH/2013/RR-16 Maharashtra Workshop, Kohlapur-416012 3 Visakha Institutional Review Board ECR/4/Indt/AP/2013/RR-16 A-11, Prince Villae Royal Appartment, Siripuram, Visakhapatnam- 530003 Andhra Pradesh SAUMYAA, C-321, Behind Ganesh Temple N-1, CIDCO, Aurangabad- 4 Aurangabad Ethics Committee ECR/122/Indt/MH/2013/RR-16 Maharashtra 431003 Ethics Committee of Diabetes Thyroid BCM Health Island, PU4, Scheme 54, Behind Prestige Management 5 ECR/409/Inst/MP/2013/RR-16 Madhya Pradesh Hormone Research Institute Institute, Near Bombay Hospital, Indore- 452010 Jehangir Clinical Development Centre Pvt. Ltd., Jehangir Hospital 6 Ethics Committee ECR/352/Inst/MH/2013/RR-19 Maharashtra Premises, 32 Sassoon Road, Pune- 411001 89, 3rd Cross, S V K Layout, Basaveshwar Nagar, Banagalore, Urban- 7 Lifeline Ethics Committee ECR/76/Indt/KA/2013/RR-16 Karnataka 560079 Instutional Ethics Committee-Clinical Indraprastha Apollo Hospitals, Sarita Vihar, Delhi- Mathura road, New 8 ECR/5/Inst/DL/2013/RR-16 Delhi Studies Delhi- 110076 H.No.- D/129, St. No.-13 Opp-Durga Mandir, Ashok Nagar, Shahdara- 9 Good Society for Ethical Research ECR/69/Indt/DL/2013/RR-19 Delhi 110093 Ethics Committee, S.P. Medical College & S.P Medical College & A.G Hospitals, HRMC Cardiovascular Sciences & 10 ECR/27/SP/Inst/RJ/2013/RR-16 Rajasthan A.G. -

Annual Report 2016-17
The Gujarat Cancer & Research Institute (M. P. Shah Cancer Hospital) STATE CANCER INSTITUTE (Recognized by Ministry of Health & Family Welfare, Govt. of India) Annual Report 2016 - 2017 Shri Pankaj R. Patel Chairman, Governing Board, GCRI Members of Governing Board Nominated by Nominated by Govt. of Gujarat Gujarat Cancer Society Shri Pankaj R. Patel Shri Punamchand Parmar, IAS Executive Chairman, Add. Chief Secretary, Health & Family Gujarat Cancer Society Welfare Department, Shri Prashant Kinarivala Government of Gujarat General Secretary, Gujarat Cancer Society Dr. Jayanti Ravi, IAS Shri Kshitish Madanmohan Commissioner of Health Services, Secretary, Government of Gujarat Gujarat Cancer Society Dr. N. L. Patel Shri Milind Torawane, IAS Vice President, Gujarat Cancer Society Secretary, Finance Department Dr. Devendra Patel (Expenditure), Government of Gujarat Former Director, GCRI Nominated by Govt. of India Chairman/Managing Director, GMDC Deputy Director General, Ministry of Health & Family Welfare, Dr. Bharat Amin, MS Government of India Nominated by Government of Gujarat Director (IF), Ministry of Health, Government of India Dr. Rakesh Vyas Incharge Director, GCRI & Member Secretary Purchase Committee Members Shri Prashant Kinarivala General Secretary, Gujarat Cancer Society Chairman Dr. Rakesh Vyas Incharge Director, GCRI Shri Kshitish Madanmohan Member Secretary Secretary, Gujarat Cancer Society Member ‘JOINT VENTURE OF GOVERNMENT OF GUJARAT AND THE GUJARAT CANCER SOCIETY’ GUJARAT CANCER & RESEARCH INSTITUTE (M. P. SHAH CANCER -

Store Name Address State City West-VS Shop No. G
Store Name Address State City West-VS Shop No. G- 21, Ground Floor, Centre Maharashtra Mumbai One Mall, Sector-30, Vashi Frc30020 1-Jain Nagar Road, Abohar Punjab Punjab Abhohar Cell World 5-9-215/ Bg-5, Shop No.01, Saphari Andhra Pradesh Abids Communications Private Plaza, Chirag Alo Lane , Abids Adrash Kumar & Sons Bhagat Singh Chowk,Near Weear Well, Punjab Abohar Abore,Punjab Pund0040 PUND2114 MOBILE Allen Solly Show room , Circular Road, Punjab Abohar RAJD16048 Purnima NAKODA TOWER,OPP.SHANTI KUNJ, Rajasthan Abu Road Stores Abu MOUNT ROAD, ABUROAD Big C Mobiles Pvt Ltd Ambedkar Chowkopp Ganesh Talkies Andhra Pradesh Adilabad Univercell D No 4 3 6 6 And 43 6 7 Hameedpura Andhra Pradesh Adilabad Telecommunications India Pvt Ltd Univercell Ground Floor D No 744 & 45 Andhra Pradesh Adilabad Telecommunications India Garimillaboundaries Main Road Pvt Ltd Mahchiryala Apex Electronics # 4-2-173/10, Cinema Road, Adilabad. Andhra Pradesh Adilabad Communication(Ses) 504001 Andd12633 Cell World 6-5-84/A And 6-7-77/14/10, Netaji Andhra Pradesh Adilabad Communications Private Chwk, Bhotapur , Adilabad Andd13850 ANDD5080 DIGITAL ZONE 4-3-8/4/5 Cinema Road Andhra Pradesh Adilabad Adilabad,Andhra Pradesh-504001 Sky Mobiles Near Ks Rtc Bus Stand Mc Road Kerala Adoor Adoor,Pathanamthitta Kerd5628 Satisfaction 142, Motorstand Road, Agartala Tripura Agartala G S Electronics (Ses) 160 H.G.B Rd.,Melar Math, Near Tripura Agartala Womens Commission Office Trid0595 Sadar Bazar 4, Taj Road, Sadar Bazar, Agra - Uttar Pradesh Agra Frc30056 Shop No.3, Block 5C, -

Tribute to Late Dr. Ashok Kanodia
AHMEDABAD MEDICAL ASSOCIATION DR. MEHUL N. SHELAT DR. KIRITKUMAR C. GADHAVI President - AMA Hon. Secretary - AMA Imm. Past President - DR. JAYESH P. SACHDE Vol.13 JANUARY-2019 Issue-9 03-02-2019 Mega Health Check-Up Camp 03-02-2019 Kid's Talent Evening 14-02-2019 Valentine's Day with Thelesemia Kids 14-02-2019 Ladies Club Programme 17-02-2019 Scientific Programme No. 6 20-02-2019 to Sports Week 28-02-2019 } 21-02-2019 Career Seminar 22-02-2019 The Guru Speaks 03-03-2019 Ladies Club Programme 10-03-2019 Woman's Day Celebration DR. KIRITKUMAR C. GADHAVI Happy Valentine's Day "LOOK BACK & THANK GOD, LOOK FORWARD & TRUST GOD" 84 27-11-2018 Message From President and Hon. Secretary Desk Respected Seniors & Dear friends, Namaste! We are thankful to you all for your whole-hearted participation in AMA programmes in good numbers. This is what we all need to meet off & on & yes make us fulfil by Edutainment. Please accept TEAM AMA’s BIG THANKS for last month’s programmes, we are trying to make every programme different & useful. Sports Zone is ready. Thanks to Dr. Adit Desai for coming and inaugurate it. Request all of you to come AMA & spare time at Sports Zone. Our thanks & salute to Dr. Maheshbhai Patel & Dr. Parimalbhai Desai for coming & give valuable suggestions in Career Seminar. Now let’s move forward with kids talents, Career Seminar for Medical Students, Community Projects & Sports Week. We have planned to celebrate Valentine Day in a special way. Need your Suggestions always. -

Abstract Book
JIC 2020 January 3-5, 2020 Abstract Book Annual Scientific GMERS th Medical College, Symposium Sola, 16 Ahmedabad 25th Year of Academics 2020 16th Annual Scientific Symposium JIC 25th Year of Academics January 3-5, 2020 LOCAL ORGANIZING COMMITTEE Conference Chairman : Dr. Keyur Parikh CIMS Hospital, Ahmedabad Conference Patron : Dr. Nitin Vora GMERS, Sola, Ahmedabad Chairman, Scientific Committee : Dr. Milan Chag CIMS Hospital, Ahmedabad Organizing Secretary : Dr. Satya Gupta CIMS Hospital, Ahmedabad : Dr. Tejas V. Patel CIMS Hospital, Ahmedabad Conference Advisor : Dr. R.M. Jitea GMERS, Sola, Ahmedabad Dr. Ajesh Desai GMERS, Sola, Ahmedabad Dr. H.R. Jadav GMERS, Sola, Ahmedabad ASSOCIATION OF PHYSICIANS OF AHMEDABAD Dr. Ashvin Gadhavi President (APA) Dr. Anil Kulshrestha Hon Secretary (APA) Conference Directors & Co-ordinators Dr. Hemang Baxi Dr. Hiren Dholakia Dr. Pranav Modi Dr. Jayesh V. Patel Dr. Jignesh Shah Dr. Sneha Baxi Dr. Manish Gandhi Dr. Ajay Naik Dr. Mayur Patil Dr. Pranav Shah Dr. Sagar Betai Dr. T.K.B. Ganpathy Dr. Dhaval Naik Dr. Ashka Prajapati Dr. Manisha Shah Dr. Darshan Bhansali Dr. Sneha Gohil Dr. Parth Parekh Dr. Hardik R. Shah Dr. Nitesh Shah Dr. Niren Bhavsar Dr. Parth Goyal Dr. Maulik Parmar Dr. Divyesh Sadadiwala Dr. Deepa Shah Dr. Devang Bhavsar Dr. Kishor Gupta Dr. Gunvant Patel Dr. Vineet Sankhla Dr. Kirtan Shah Dr. Maulik Bhensdadia Dr. Krunal H. Patel Dr. Chandni Patel Dr. Praveen Sarda Dr. Rupesh Shah Dr. Parloop Bhatt Dr. Rajiv Harshe Dr. Vivek Patel Dr. Urmil Shah Dr. Nimish Sharma Dr. Reena Sharma Dr. Keyur Buch Dr. Abhinav Jain Dr. Prashant Patel Dr. Dhiren Shah Dr. -
Dr. Jitendra N. Patel Dr. Devendra R. Patel
Dr. Jitendra N. Patel Dr. Devendra R. Patel Dr. Mahadev Desai Dr. Shivangi A. Patel Dr. Atul P. Kansara Dr. Jitesh A. Desai Dr. Amit P. Shah Dr. Pravinaben M. Santwani Dr. Mukund M. Prabhakar Dr. Pankaj Modi Dr. Tushar Patel Dr. Niyat Pandya Dr. Haresh Doshi Dr. Manish G. Shah Dr. Bhavesh Patel Ahmedabad Ahmedabad Zone Dr. Kailashben Parikh Vadodara Vadodara Zpme Dr. Kishor Ruparelia Surat Surat Zone Dr. Vikram Patel Mehsana Central Zone Dr. Bhavesh Devani Morbi West Zone Dr. Rajesh C. Rohit Dadranagar Sourth Zone 9 I.M.A.G.S.B. NEWS BULLETIN / DECEMBER - 2013 Vol. 8 No. 12 Dear colleagues, Health is a forefront issue of the society. Unhealthy people will surely lead to unhealthy society and a burden to family,society and to the economy. As a doctor it is our prime responsibility to keep society healthy and fit. We should keep our self updated in latest development in the field of medicine. The function of the medical professions does not mean only high technology of the curative medicine; the comparable importance goes to the health education, health promotion, disease prevention and rehabilitation as well as the sustainability of the actions. To reach the ultimate goal of healthy world, medical professions needed to be involved in so many issues such as environment preservation, family life styles, pollution control and so on, which are also the issues amongst the public and policy makers. Therefore, it is our duty to be united and share our information, knowledge, and experience to prevent and find proper solutions to overcome or to suppress the risks of spreading diseases and illnesses. -
Compendium of Instructions for Covid 19 Testing Laboratory Second Edition Volume 2
COMPENDIUM OF INSTRUCTIONS FOR COVID-19 TESTING LABORATORY Medical Education and Drugs Department Government of Maharashtra SECOND EDITION VOLUME 2 06 July 2020 Medical Education and Drugs Department COMPENDIUM OF INSTRUCTIONS FOR COVID-19 TESTING LABORATORY SECOND EDITION VOLUME 2 Editor -in -chief Dr. Sanjay Mukherjee, IAS Secretary Medical Education and Drugs Department Government of Maharashtra Editors Dr. Rajesh Karyakarte, Dr. Sachin Mulkutkar, Professor Professor B.J. Government Medical College, Grant Government Medical College, Pune Mumbai Co-Editors Dr. Rakesh Waghmare, Dr. Mandar Sadawarte, Associate Professor Assistant Professor Grant Government Medical College, Grant Government Medical College, Mumbai Mumbai FOREWORD As you are aware, COVID – 19 is widely spreading across the country, rising beyond 600000 rd positive cases in the 23 week. In order to manage and contain the spread of COVID – 19 any further, both Centre and State Government and Associated Departments have come out with Guidelines and Instructions for COVID-19 Testing to be adopted across the country and in each state. This Compendium is a compilation of instructions & guidelines for operating a Covid-19 Testing Laboratory issued by Ministry of Health & Family Welfare, Indian Council of Medical Research, Government of India and instructions issued by Public Health Department and Medical Education and Drugs Department of Government of Maharashtra. All the information provided in this Compendium is available in publicly available sources. We hope that this compilation helps Laboratory In-charges, Administrators and all people involved in Testing of COVID – 19 cases. This Compendium is updated with the information issued till 6th July, 2020. The Editorial Board shall be updating this on a regular basis. -
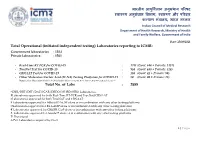
Total Operational (Initiated Independent Testing) Laboratories Reporting to ICMR
भारतीय आयु셍वज्ञि ान अनुसंधान पररषद वा्य अनुसंधान 셍वभाग, वा्य और पररवार क쥍याण मंत्रालय, भारत सरकार Indian Council of Medical Research Department of Health Research, Ministry of Health and Family Welfare, Government of India Date: 25/08/2021 Total Operational (initiated independent testing) Laboratories reporting to ICMR: Government laboratories : 1324 Private laboratories : 1561 - Real-Time RT PCR for COVID-19 : 1781 (Govt: 644 + Private: 1137) - TrueNat Test for COVID-19 : 954 (Govt: 630 + Private: 324) - CBNAAT Test for COVID-19 : 130 (Govt: 42 + Private: 88) - Other Molecular-Nucleic Acid (M-NA) Testing Platforms for COVID-19 : 20 (Govt: 08 + Private: 12) Note: Other Molecular-Nucleic Acid includes Abbott ID NOW, RT-LAMP, CRISPR-Cas9 and Accula™ Total No. of Labs : 2885 *CSIR/DBT/DST/DAE/ICAR/DRDO/MHRD/ISRO Laboratories. #Laboratories approved for both Real-Time RT-PCR and TrueNat/CBNAAT $Laboratories approved for both TrueNAT and CBNAAT ¥ Laboratories approved for Abbott ID NOW alone or in combination with any other testing platforms @Laboratories approved for RT-LAMP alone or in combination with any other testing platforms € Laboratories approved for CRISPR-Cas9 alone or in combination with any other testing platforms δ Laboratories approved for Accula™ alone or in combination with any other testing platforms P: Provisional Δ Pvt. Laboratories acquired by Govt. 1 | P a g e S. Test Names of States Names of Government Institutes Names of Private Institutes No. Category 1. Andhra Pradesh RT-PCR 1. Sri Venkateswara Institute of Medical 1. Manipal Hospital, Tadepalli, Guntur (134) Sciences, Tirupati 2. -
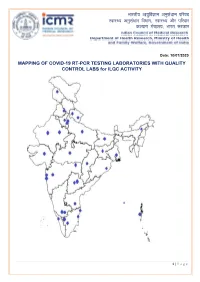
MAPPING of COVID-19 RT-PCR TESTING LABORATORIES with QUALITY CONTROL LABS for ILQC ACTIVITY
भारतीय आयुर्विज्ञान अनुसंधान पर्रषद वा्य अनुसंधान र्वभाग, वा्य और पर्रवार क쥍याण मंत्रालय, भारत सरकार Date: 10/07/2020 MAPPING OF COVID-19 RT-PCR TESTING LABORATORIES WITH QUALITY CONTROL LABS for ILQC ACTIVITY 1 | P a g e QC labs across India State Name of QC Lab Telangana Gandhi Medical College, Secunderabad Osmania Medical College, Hyderabad Andhra Pradesh Sri Venkateshwara Institute of Medical Sciences, Tirupati Uttar Pradesh King George Medical University, Lucknow Uttarakhand All India Institute of Medical Sciences, Rishikesh Govt. Medical College, Haldwani West Bengal National Institute of Cholera and Enteric Diseases, Kolkata Assam, Arunachal Pradesh, Manipur, Regional Medical Research Centre, Dibrugarh Meghalaya, Mizoram, Nagaland, Tripura Bihar ICMR-Rajendra Memorial Research Institute of Medical Sciences, Patna Chandigarh, Himachal Pradesh and Post Graduate Institute of Medical Education & Research, Punjab Chandigarh Chhattisgarh All India Institute of Medical Sciences, Raipur Delhi All India Institute Medical Sciences, Delhi Maulana Azad Medical College, Delhi Gujarat BJ Medical College, Ahmedabad Maharashtra ICMR-National Institute of Virology, Pune ICMR-National Institute of Virology Field Unit, Mumbai Kasturba Hospital for Infectious Diseases, Mumbai All India Institute of Medical Sciences, Nagpur Haryana BPS Govt. Medical College, Sonipat Ladakh Sher-i-Kashmir Institute of Medical Sciences, Srinagar Jharkhand Rajendra Institute of Medical Sciences, Ranchi Karnataka Bangalore Medical College & Research Institute, Bengaluru ICMR-National Institute of Virology, Bangalore Field Unit, Bengaluru Kerala ICMR-National Institute of Virology, Field Unit, Allapuzzha Madhya Pradesh All India Institute of Medical Sciences, Bhopal Odisha ICMR-Regional Medical Research Centre, Bhubaneshwar Puducherry Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry Rajasthan Sawai Man Singh Medical College, Jaipur All India Institute of Medical Sciences, Jodhpur Tamil Nadu King Institute of Preventive Medicine & Research, Chennai Govt. -
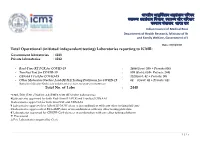
Total Operational (Initiated Independent Testin Total No. of Labs वा य अनुसंधान Ted Independent Testing) L
भारतीय आयुवान अनसु धं ान परषद वाय अअनुसंधाननुसधं ान िवभाग, वाय और परवार कयाण मंालय, भारत सरकार Indian Council of Medical Research Department of Health Research, Ministry of Health and Family Welfare, Government of India Date: 01/04/2021 Total Operational (initiated independent testing) Laboratories reporting to ICMR: Government laboratories : 1228 Private laboratories : 1212 - Real-Time RT PCR for COVID-19 : 1406(Govt: 550 + Private:856) - TrueNat Test for COVID-19 : 898 (Govt: 634+ Private: 264) - CBNAAT Test for COVID-19 : 132(Govt: 42 + Private: 90) - Other Molecular-Nucleic Acid (M-NA)Testing Platforms for COVID-19 : 04 (Govt: 02 + Private: 02) Note:Other Molecular-Nucleic Acid includes Abbott ID NOW, RT-LAMP and CRISPR-Cas9 Total No. of Labs : 2440 *CSIR/DBT/DST/DAE/ICAR/DRDO/MHRD/ISRO Laboratories. #Laboratories approved for both Real-Time RT-PCR and TrueNat/CBNAAT $Laboratories approved for both TrueNAT and CBNAAT ¥ Laboratories approved for Abbott ID NOW alone or in combination with any other testing platforms @Laboratories approved for RT-LAMP alone or in combination with any other testing platforms € Laboratories approved for CRISPR-Cas9 alone or in combination with any other testing platforms P: Provisional Δ Pvt. Laboratories acquired by Govt. 1 | Page S. Names of Test Names of Government Institutes Names of Private Institutes No. States Category 1. Andhra RT-PCR 1. Sri Venkateswara Institute of 1. Manipal Hospital, Tadepalli, Guntur Pradesh (124) Medical Sciences, Tirupati 2. PathGene Health Care Pvt 2. Sri Venkateswara Medical Ltd#2nd Floor, Srinivasapuram, Govt: 78 College, Tirupati Tiruchanoor Road, Opp LV Private: 46 3. -

Smt. NHL Municipal Medical College, Ahmedabad Regional Centre in Medical Education Technologies First Basic Course Workshop
Smt. NHL Municipal Medical College, Ahmedabad Regional Centre in Medical Education Technologies First Basic Course Workshop Date of Workshop: July 1- 3, 2009 Name of Observer: Nil List of Participants Sr. Name of Designation and Official Contact E-mail ID No. Participant Department Address Details (Tel./ Fax/Mobile) 1. Dr. Kiran Assistant Professor, S.B.K.S. Medical 9427320782 [email protected] Tripathi Department of Institute & Microbiology Research Centre, Pipariya 2. Dr. Dimple Assistant Professor, S.B.K.S. Medical 0265 - [email protected] Darad Department of Institute & 2322858 Pathology Research Centre, 9825288185 Pipariya 3. Dr. U.I. Sr. Tutor, S.B.K.S. Medical 904840340 NA Bhatt Department of Institute & Physiology Research Centre, Pipariya 4. Dr. Jitendra Assistant Professor, S.B.K.S. Medical 9426759749 [email protected] Zaveri Department of Institute & Pharmacology Research Centre, Pipariya 5. Dr. Niraj Associate Professor, S.B.K.S. Medical 9825371135 [email protected] Pandit Department of Institute & Community Research Centre, Medicine Pipariya 6. Dr. Hetal Associate Professor, S.B.K.S. Medical 9998055159 [email protected] Pandya Department of Institute & Medicine Research Centre, Pipariya 7. Dr. Chaitri Assistant Professor, S.B.K.S. Medical 9924110147 [email protected] Shah Department of Institute & Medicine Research Centre, Pipariya 8. Dr. Lakhan Assistant Professor, S.B.K.S. Medical 9426334561 [email protected] Kataria Department of Institute & Psychiatry Research Centre, Pipaliy 9. Dr. Vijoy Professor, S.B.K.S. Medical 02668 - [email protected] Singh Department of Institute & 245028 Surgery Research Centre, 9974005726 Pipariya 10. Dr. -

AMC Medical Education Trust EST.No, 1806
--- \___l --- - AMC MET AMC Medical Education Trust EST.No, 1806 ORDER As per the recommendation of Departmental Promotion Committee dl, 22/08120L9 and approval of Chairman, AMC Medical Education Trust dt. 22108120f9 following teaching faculty at AMC MET is being promoted to the post and grade as follow from ,mmed iate effect. Sr. Name of Doctor Present Design ation & Design ation After Posting at No H osp ita I Promotion & Pay 5ca le Co llege/ Hospita I 1 Dr. U rvish Parikh Asst. Professor Asso. Professor N HL/SV P Hos pita I (Practicing) (Pra cticing) on the vacant post of (Peadiatric Surgery) (Pea d iatric Sur8ery) Dr, Sud h ir Chandna NHL/SVP Hospita I Rs. 25,000/- Fix (Monthly) Conditions of Promotion: 1. This appointment is subiect to confirmation of Governing Body of AMC Medical Education Trust. 2. The other terms and conditions will remain same as per her/his previous appointment order. 3. The service will be subiect to the rules and regulation of this institution in force and to be changed from time to time. 4. One month notice period required at the time of resignation. This order comes into force with immediate effect. sd/- (Dr. Ku ldeep Arya) ot.:26/08120L9 Secretary AMC MET CCto: 1) Dean, NHL MedicalCollege for information 2l Dean, AMC MET Medical College for information 3) Medical Superintendent, 5VP Hospital 4) Dr. Urvish Parikh, SVP Hospital s) Co n cern Bill Clerk AIII\lEDABAO I\lUNICIPAL CORPOf,ATION (Pat h ik C.Shah) D irecto r AMCMET Registered Otfice: Ahmedabad Municipal Corporation, Dr.