Definitions of Medicare Code Edits
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gyn Oncology Colposcopy I. Basic Science/Mechanisms of Disease A
Gyn Oncology Colposcopy I. Basic Science/Mechanisms of Disease A. Genetics 1. Describe the clinical relevance of viral oncogenes. 2. Describe the role of aneuploidy in the pathogenesis of neoplasia. 3. Describe the inheritance patterns for malignancies of the pelvic organs and breast. 4. Describe the cell replication cycle, and identify the phases of the cycle most sensitive to radiation and chemotherapy. 5. Describe the genetic basis for tumor immunotherapy. B. Physiology 1. Describe the ability of vital organ systems to tolerate cancer therapy. 2. Describe the changes in cellular physiology that result from injury due to radiation and chemotherapy. 3. Describe the metabolic changes that occur in patients with a malignancy of the pelvic organs or breast. C. Embroyology 1. Describe the embryology of gonadal migration and its role in the pathogenesis of epithelial cell tumors. 2. Describe the pathogenesis of gonadal tumors in patients with gonadal dysgenesis. 3. Describe the embryologic precursors of ovarian germ cell tumors. D. Anatomy 1. Describe the gross histologic anatomy of the pelvic organs and breast. 2. Describe the vascular, lymphatic, and nerve supply to each of the pelvic organs. 3. Describe the anatomic relationship between the reproductive organs and other viscera, such as bladder, ureters, and bowel. 4. Describe the likely changes in the anatomic relationships of the pelvic and abdominal viscera created by surgical or radiation treatment for malignancy. E. Pharmacology 1. List major chemotherapeutic agents used for treatment of malignancies of the reproductive organs and breast. 2. Describe the principal adverse effects of the major chemotherapeutic agents. 3. Describe the medications of most value in treatment of complications resulting from chemotherapy and irradiation, such as: a. -

Physiology of Female Sexual Function and Dysfunction
International Journal of Impotence Research (2005) 17, S44–S51 & 2005 Nature Publishing Group All rights reserved 0955-9930/05 $30.00 www.nature.com/ijir Physiology of female sexual function and dysfunction JR Berman1* 1Director Female Urology and Female Sexual Medicine, Rodeo Drive Women’s Health Center, Beverly Hills, California, USA Female sexual dysfunction is age-related, progressive, and highly prevalent, affecting 30–50% of American women. While there are emotional and relational elements to female sexual function and response, female sexual dysfunction can occur secondary to medical problems and have an organic basis. This paper addresses anatomy and physiology of normal female sexual function as well as the pathophysiology of female sexual dysfunction. Although the female sexual response is inherently difficult to evaluate in the clinical setting, a variety of instruments have been developed for assessing subjective measures of sexual arousal and function. Objective measurements used in conjunction with the subjective assessment help diagnose potential physiologic/organic abnormal- ities. Therapeutic options for the treatment of female sexual dysfunction, including hormonal, and pharmacological, are also addressed. International Journal of Impotence Research (2005) 17, S44–S51. doi:10.1038/sj.ijir.3901428 Keywords: female sexual dysfunction; anatomy; physiology; pathophysiology; evaluation; treatment Incidence of female sexual dysfunction updated the definitions and classifications based upon current research and clinical practice. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
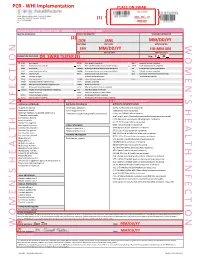
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

AAGL Practice Report: Practice Guidelines for Management of Intrauterine Synechiae
Special Article AAGL Practice Report: Practice Guidelines for Management of Intrauterine Synechiae AAGL ADVANCING MINIMALLY INVASIVE GYNECOLOGY WORLDWIDE Background The search was not restricted to English language literature; committee members fluent in languages other than English re- Intrauterine adhesions (IUAs) have been recognized as viewed relevant articles and provided the committee with rel- a cause of secondary amenorrhea since the end of the 19th ative information translated into English. Because of the century [1], and in the mid-20th century, Asherman further paucity of data in this area, all published works were included described the eponymous condition occurring after preg- for the electronic database searches, and relevant articles not nancy [2]. The terms ‘‘Asherman syndrome’’ and IUAs are available in electronic sources (e.g., published before the be- often used interchangeably, although the syndrome requires ginning of electronic database commencement) were cross- the constellation of signs and symptoms (in this case, pain, referenced from hand-searched bibliographies and included menstrual disturbance, and subfertility in any combination) in the literature review. When necessary, authors were con- and the presence of IUAs [2]. The presence of IUAs in the tacted directly for clarification of points published. absence of symptoms may be best referred to as asymptom- atic IUAs or synechiae. Diagnosis Identification and Assessment of Evidence In women with suspected IUAs, physical examination usually fails to reveal abnormalities [3,4]. Blind transcervical This AAGL Practice Guideline was produced after elec- sounding of the uterus may reveal cervical obstruction at or tronic resources including Medline, PubMed, CINAHL, the near the level of the internal os [3]. -
OBGYN Student Guide 2014.Pdf
TABLE OF CONTENTS COMMON ABBREVIATIONS • 3 COMMON PRESCRIPTIONS • 4 OBSTETRICS • 5 What is a normal morning like on OB? • 5 What are good questions to ask a post-op/post-partum patient in the morning? • 6 How do I manage a post-partum patient? • 7 How should I organize and write my post-partum note? • 8 How do I present a patient on rounds? • 9 How do I evaluate a patient in triage/L&D? • 9 What are the most common complaints presented at triage/L&D? • 10 How should I organize and write my note for a triage H&P? • 12 What are the most common reasons people are admitted? • 13 How do I deliver a baby? • 13 What is my role as a student in a Cesarean section or tubal ligation procedure? • 15 How do I write up post-op orders? • 15 GYNECOLOGY/GYNECOLOGY ONCOLOGY • 17 What should I do to prepare for a GYN surgery? • 17 How do I manage a Gynecology/Gynecology Oncology patient? • 17 How should I organize and write my post-op GYN note? • 18 How do I write admit orders? • 19 What do routine post-op orders (Day #1) look like? • 19 What are the most common causes of post-operative fever? • 20 CLINIC • 21 What is my role as a student in clinic? • 21 What should I include in my prenatal clinic note? • 21 What should I include in my GYN clinic note? • 22 COMMON PIMP QUESTIONS • 23 2 COMMON ABBREVIATIONS 1°LTCS- primary low transverse cesarean LOF- leakage of fluid section NST- nonstress test AFI- amniotic fluid index NSVD- normal spontaneous vaginal delivery AROM- artificial rupture of membranes NT/NE- non-tender/non-engorged (breast BPP- biophysical -

Culdocentesis in Diagnosis of Disturbed Ectopic Pregnancy Still a Useful Procedure in Developing Countries
CULDOCENTESIS IN DIAGNOSIS OF DISTURBED ECTOPIC PREGNANCY STILL A USEFUL PROCEDURE IN DEVELOPING COUNTRIES Pages with reference to book, From 5 To 6 Tasneem Aslam Tariq ( Department of Obstetrics and Gynaecology, Jinnah Postgraduate Medical Centre, Karachi. ) Razia Korejo ( Department of Obstetrics and Gynaecology, Jinnah Postgraduate Medical Centre, Karachi. ) ABSTRACT Over a period of 5 years culdocentesis was carried out in 156 cases of suspected ectopic pregnancy using needle aspiration through the pouch of Douglas. The result was positive in 134 cases, with 131 being true positive and 3 false positive. In 22 cases the result was negative, 6 of which were false negative. It is concluded that culdocentesis is an effective method of diagnosing disturbed ectopic pregnancy (JPMA 42: 5, 1992). INTRODUCTION Ectopic pregnancy, a clinical diagnosis in majority of cases is infrequently seen in our hospital. Since it can present with varied symptoms, diagnosis can be difficult in some cases. To increase the accuracy rate of preoperative diagnosis in suspected cases of ectopic pregnancy, various diagnostic procedures have been employed over the years. The purpose of this study was to evaluate the efficacy of culdocentesis for the diagnosis of ectopic pregnancy. PATIENTS AND METHOD The present study included 156 suspected cases of ectopic pregnancy admitted to the Department of Obstetrics and Gynaecology between January, 1985 to December 1989. Culdocentesis was done in the operating theatre under aseptic precautions with or without general anaesthesia depending on the certainty of the diagnosis. Urinary bladder was catheterized and gentle bimanual vaginal examination was done to confirm the previous vaginal findings. Sims speculum was introduced in the vagina and posterior lip of cervix was held gently with a Vulsellum forceps, pulled upwards and forwards exposing the posterior fornix. -

Women's Health Course Guide
Course Guide for Women’s Health 1 Approach to the Patient The OB/GYN History Rationale: A gynecological evaluation is an important part of primary health care and preventive medicine for women. A gynecological assessment should be a part of every woman’s general medical history and physical examination. Certain questions must be asked of every woman, whereas other questions are specific to particular problems. To accomplish these objectives, optimal communication must be achieved between patient and physician. The student will demonstrate the ability to: A. Perform a thorough obstetric-gynecologic history as a portion of a general medical history, including: 1. Chief complaint 2. Present illness 3. Menstrual history 4. Obstetric history 5. Gynecologic history 6. Contraceptive history 7. Sexual history 8. Family history 9. Social history B. Interact with the patient to gain her confidence and to develop an appreciation of the effect of her age, racial and cultural background, and economic status on her health; C. Communicate the results of the obstetric-gynecologic and general medical history by well-organized written and oral reports. The OB/GYN Examination Rationale: An accurate examination complements the history, provides additional information and helps determine diagnosis and guide management. It also provides an opportunity to educate and reassure the patient. The student will demonstrate the ability to: A. Interact with the patient to gain her confidence and cooperation, and assure her comfort and modesty B. Perform a painless obstetric-gynecologic examination as part of a woman’s general medical examination, including: 1. Breast examination 2. Abdominal examination 3. Complete pelvic examination 4. -

Female Pelvic Relaxation
FEMALE PELVIC RELAXATION A Primer for Women with Pelvic Organ Prolapse Written by: ANDREW SIEGEL, M.D. An educational service provided by: BERGEN UROLOGICAL ASSOCIATES N.J. CENTER FOR PROSTATE CANCER & UROLOGY Andrew Siegel, M.D. • Martin Goldstein, M.D. Vincent Lanteri, M.D. • Michael Esposito, M.D. • Mutahar Ahmed, M.D. Gregory Lovallo, M.D. • Thomas Christiano, M.D. 255 Spring Valley Avenue Maywood, N.J. 07607 www.bergenurological.com www.roboticurology.com Table of Contents INTRODUCTION .................................................................1 WHY A UROLOGIST? ..........................................................2 PELVIC ANATOMY ..............................................................4 PROLAPSE URETHRA ....................................................................7 BLADDER .....................................................................7 RECTUM ......................................................................8 PERINEUM ..................................................................9 SMALL INTESTINE .....................................................9 VAGINAL VAULT .......................................................10 UTERUS .....................................................................11 EVALUATION OF PROLAPSE ............................................11 SURGICAL REPAIR OF PELVIC PROLAPSE .....................15 STRESS INCONTINENCE .........................................16 CYSTOCELE ..............................................................18 RECTOCELE/PERINEAL LAXITY .............................19 -

Comparison of Curettage and Hysteroscopy Plus Curettage After Uterine Arterial Embolization in the Treatment of Cesarean Scar Pregnancy
Comparison of Curettage and Hysteroscopy Plus Curettage After Uterine Arterial Embolization in the Treatment of Cesarean Scar Pregnancy Lili Cao Women's Hospital, Zhejiang University School of Medicine Zhida Qian Women's Hospital, Zhejiang University School of Medicine Lili Huang ( [email protected] ) Women's Hospital, Zhejiang University School of Medicine https://orcid.org/0000-0002-5919-3172 Research article Keywords: Cesarean scar pregnancy, Hysteroscopy, Curettage, Uterine artery embolization Posted Date: July 2nd, 2020 DOI: https://doi.org/10.21203/rs.3.rs-39244/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/11 Abstract Background: Caesarean scar pregnancy (CSP) stands for the advanced stage severe complication secondary to cesarean section, and its incidence shows an increasing trend recently. However, no consensus has been reached about the optimal CSP treatment. Methods: The childbearing CSP patients with a cesarean section history were evaluated by ultrasonography, with a gestational age of less than 10 weeks. 34 patients receiving dilation and curettage (D&C) and uterine artery embolization (UAE) were enrolled into the D&C group, while 46 undergoing hysteroscopy (H/S) and D&C after UAE were enrolled into the H/S+D&C group. Results: Differences in success rate and decrease in the β-hCG level in serum on the second day of surgery were not signicant between D&C and H/S+D&C groups (P>0.05). Also, differences in side effect rate, intraoperative blood loss amount, postoperative bleeding time, and total length of stay were not signicant between both groups (P>0.05). -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -

Types and Efficacy of Diagnostic Modalities of Ectopic Pregnancy
Jebmh.com Original Research Article Types and Efficacy of Diagnostic Modalities of Ectopic Pregnancy Pavani Pinjala1 1Department of Obstetrics and Gynaecology Mahavir Institute of Medical Sciences, Vikarabad, Hyderabad, Telangana, India. ABSTRACT BACKGROUND Ectopic pregnancy is not only the gynaecologist’s most critical emergency but also Corresponding Author: one of the major problems because of its difficulties in diagnosis, increased risks Dr. Pavani Pinjala, of mortality, and its profound implications with regard to future reproductive Block – D - 206, Vazhraa Nirmaan Pushpak Apartments, performance. We wanted to study the types and accuracy of various diagnostic Blooming Dale Road, Nizampet, modalities, and effect of various management modalities of ectopic pregnancy. Hyderabad – 500090, Telangana, India. E-mail: [email protected] METHODS This study was conducted at Meenakshi Medical College Hospital and Research DOI: 10.18410/jebmh/2020/568 Institute, Kanchipuram, for a period of 32 months from May 2010 to October 2012. During the same period, there were 2602 reported pregnancies. How to Cite This Article: Pinjala P. Types and efficacy of diagnostic modalities of ectopic RESULTS pregnancy. J Evid Based Med Healthc The incidence of ectopic pregnancy in the study is 15.3 / 1000 reported 2020; 7(47), 2767-2771. DOI: pregnancies. The incidence of ectopic pregnancy in patients with prior abdominal 10.18410/jebmh/2020/568 surgery was 86.6 %. Only 77.5 % patients gave history of typical amenorrhea. Submission 20-08-2020, 22.5 % patients gave history suggestive of atypical amenorrhoea. It was noted Peer Review 28-08-2020, that 55 % cases presented as tubal rupture, 7.5 % as tubal abortion, 35 % cases Acceptance 05-10-2020, presented with intact tubal pregnancy and 2.5 % cases presented as ovarian Published 23-11-2020.