Vagus Nerve Stimulation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

6 Ways to Instantly Stimulate Your Vagus Nerve to Relieve Inflammation, Depression, Migraines and More
O 6 WAYS TO INSTANTLY STIMULATE YOUR VAGUS NERVE TO RELIEVE INFLAMMATION, DEPRESSION, MIGRAINES AND MORE I read an article yesterday that has me extremely excited about the implications. The article is called “Hacking the Nervous System” by Gaia Vince (http://mosaicscience.com/story/hacking-nervous-system). In the article, the author describes the experience of a woman who suffered from severe, debilitating rheumatoid arthritis and her eventual treatment with a device which minimized inflammation by simply stimulating the vagus nerve. What this means, is that by activating the vagus nerve which works through the parasympathetic nervous system, we can greatly influence inflammation and the immune system. The role of the brain on body inflammation can be profound. If you suffer from digestive complaints, high blood pressure, depression or any inflammatory condition, please read on. Let me explain the possible implications step by step. What is the vagus nerve? First of all, the vagus nerve is the longest nerve in the body which originates in the brain as cranial nerve ten, travels down the from go the neck and then passes around the digestive system, liver, spleen, pancreas, heart and lungs. This nerve is a major player in the parasympathetic nervous system, which is the ‘rest and digest’ part (opposite to the sympathetic nervous system which is ‘fight of flight’). Vagal tone The tone of the vagus nerve is key to activating the parasympathetic nervous system. Vagal tone is measured by tracking your heart-rate alongside your breathing rate. Your heart-rate speeds up a little when your breathe in, and slows down a little when you breathe out. -

Questions and Answers About Vagus Nerve Stimulation by Jerry Shih, M.D. 1. WHAT IS VAGUS NERVE STIMULATION? Therapeutic Vagus Ne
Questions and Answers About Vagus Nerve Stimulation By Jerry Shih, M.D. 1. WHAT IS VAGUS NERVE STIMULATION? Therapeutic vagus nerve stimulation (VNS) is chronic, intermittent electrical stimulation of the mid-cervical segment of the left vagus nerve. The stimulation occurs automatically at set intervals, during waking and sleep. The electrical pulses are generated by a pacemaker-like device that is implanted below the clavicle and are delivered by a lead wire that is coiled around the vagus nerve. 2. WHAT IS THE EVIDENCE THAT VAGUS NERVE STIMULATION IS EFFECTIVE IN EPILEPSY? The empirical evidence of antiepileptic efficacy arose sequentially from l) experiments in animal models of epilepsy; 2) anecdotal reports and small case series ofearly human trials, and 3) two prospec-tive, double-blind, controlled studies in large groups of patients with complex partial and secondarily generalized seizures. 3. HOW DOES VAGUS NERVE STIMULATION CONTROL SEIZURES? The mechanisms by which therapeutic VNS reduces seizure activity in humans and in experimental models of epilepsy are unknown. 4. WHEN SHOULD ONE CONSIDER VAGUS NERVE STIMULATION? Medically refractory complex partial and secondarily generalized seizures have been efficaciously treated with adjunctive VNS in the large, randomized studies. Children may benefit considerably from VNS, but large-scale, randomized, controlled studies have not been completed in young children. Thus, any adolescent or adult whose complex partial or secondarily generalized seizures have not been controlled with the appropriate first- and second -line antiepileptic drugs may be a good candidate for VNS. The FDA has specifically approved VNS with the Cyberonics device for adjunctive therapy of refractory partial-onset seizures in persons l2 years of age. -

Long-Term Results of Vagal Nerve Stimulation for Adults with Medication-Resistant
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Seizure 22 (2013) 9–13 Contents lists available at SciVerse ScienceDirect Seizure jou rnal homepage: www.elsevier.com/locate/yseiz Long-term results of vagal nerve stimulation for adults with medication-resistant epilepsy who have been on unchanged antiepileptic medication a a, b a c a Eduardo Garcı´a-Navarrete , Cristina V. Torres *, Isabel Gallego , Marta Navas , Jesu´ s Pastor , R.G. Sola a Division of Neurosurgery, Department of Surgery, University Hospital La Princesa, Universidad Auto´noma, Madrid, Spain b Division of Neurosurgery, Hospital Nin˜o Jesu´s, Madrid, Spain c Department of Physiology, University Hospital La Princesa, Madrid, Spain A R T I C L E I N F O A B S T R A C T Article history: Purpose: Several studies suggest that vagal nerve stimulation (VNS) is an effective treatment for Received 15 July 2012 medication-resistant epileptic patients, although patients’ medication was usually modified during the Received in revised form 10 September 2012 assessment period. The purpose of this prospective study was to evaluate the long-term effects of VNS, at Accepted 14 September 2012 18 months of follow-up, on epileptic patients who have been on unchanged antiepileptic medication. Methods: Forty-three patients underwent a complete epilepsy preoperative evaluation protocol, and Keywords: were selected for VNS implantation. After surgery, patients were evaluated on a monthly basis, Vagus nerve increasing stimulation 0.25 mA at each visit, up to 2.5 mA. Medication was unchanged for at least 18 Epilepsy months since the stimulation was started. -

Current Neurosurgical Management of Glossopharyngeal Neuralgia and Technical Nuances for Microvascular Decompression Surgery
Neurosurg Focus 34 (3):E8, 2013 ©AANS, 2013 Current neurosurgical management of glossopharyngeal neuralgia and technical nuances for microvascular decompression surgery ROBERTO REY-DIOS, M.D.,1 AND AARON A. COHEN-GADOL, M.D., M.SC.2 1Department of Neurosurgery, University of Mississippi Medical Center, Jackson, Mississippi; 2Goodman Campbell Brain and Spine, Indiana University Department of Neurological Surgery, Indianapolis, Indiana Glossopharyngeal neuralgia (GPN) is an uncommon facial pain syndrome often misdiagnosed as trigeminal neuralgia. The rarity of this condition and its overlap with other cranial nerve hyperactivity syndromes often leads to a significant delay in diagnosis. The surgical procedures with the highest rates of pain relief for GPN are rhizotomy and microvascular decompression (MVD) of cranial nerves IX and X. Neurovascular conflict at the level of the root exit zone of these cranial nerves is believed to be the cause of this pain syndrome in most cases. Vagus nerve rhizotomy is usually reserved for cases in which vascular conflict is not evident. A review of the literature reveals that although the addition of cranial nerve X rhizotomy may improve the chances of long-term pain control, this maneuver also increases the risk of permanent dysphagia and vocal cord paralysis. The risks of this procedure have to be carefully weighed against its benefits. Based on the authors’ experience, careful patient selection with a thorough exploratory operation most often leads to identification of the site of vascular conflict, obviating the need for cranial nerve X rhizotomy. (http://thejns.org/doi/abs/10.3171/2012.12.FOCUS12391) KEY WORDS • glossopharyngeal neuralgia • microvascular decompression • vagus nerve • rhizotomy • cranial nerve LOSSOPHARYNGEAL neuralgia, or vagoglossopharyn impairment can be found in the distribution of the above geal neuralgia, is a cranial nerve hyperactivity nerves due to structural lesions.20 This classification does pain syndrome leading to severe, transient, sharp not take into consideration associated syncopal events. -

Trans-Auricular Vagus Nerve Stimulation in The
Psychiatria Danubina, 2020; Vol. 32, Suppl. 1, pp 42-46 Conference paper © Medicinska naklada - Zagreb, Croatia TRANS-AURICULAR VAGUS NERVE STIMULATION IN THE TREATMENT OF RECOVERED PATIENTS AFFECTED BY EATING AND FEEDING DISORDERS AND THEIR COMORBIDITIES Yuri Melis1,2, Emanuela Apicella1,2, Marsia Macario1,2, Eugenia Dozio1, Giuseppina Bentivoglio2 & Leonardo Mendolicchio1,2 1Villa Miralago, Therapeutic Community for Eating Disorders, Cuasso al Monte, Italy 2Food for Mind Innovation Hub: Research Center for Eating Disorders, Cuasso al Monte, Italy SUMMARY Introduction: Eating and feeding disorders (EFD’s) represent the psychiatric pathology with the highest mortality rate and one of the major disorders with the highest psychiatric and clinical comorbidity. The vagus nerve represents one of the main components of the sympathetic and parasympathetic nervous system and is involved in important neurophysiological functions. Previous studies have shown that vagal nerve stimulation is effective in the treatment of resistant major depression, epilepsy and anxiety disorders. In EFD’s there are a spectrum of symptoms which with Transcutaneous auricular Vagus Nerve Stimulation (Ta-VNS) therapy could have a therapeutic efficacy. Subjects and methods: Sample subjects is composed by 15 female subjects aged 18-51. Admitted to a psychiatry community having diagnosed in according to DSM-5: anorexia nervosa (AN) (N=9), bulimia nervosa (BN) (N=5), binge eating disorder (BED) (N=1). Psychiatric comorbidities: bipolar disorder type 1 (N=4), bipolar disorder type 2 (N=6), border line disorder (N=5). The protocol included 9 weeks of Ta-VNS stimulation at a frequency of 1.5-3.5 mA for 4 hours per day. The variables detected in four different times (t0, t1, t2, t3, t4) are the following: Heart Rate Variability (HRV), Hamilton Depression Rating Scale (HAMD-HDRS- 17), Body Mass Index (BMI), Beck Anxiety Index (BAI). -
Vagus Nerve Stimulation (PDF)
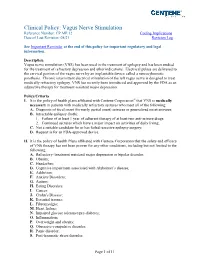
Clinical Policy: Vagus Nerve Stimulation Reference Number: CP.MP.12 Coding Implications Date of Last Revision: 08/21 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Vagus nerve stimulation (VNS) has been used in the treatment of epilepsy and has been studied for the treatment of refractory depression and other indications. Electrical pulses are delivered to the cervical portion of the vagus nerve by an implantable device called a neurocybernetic prosthesis. Chronic intermittent electrical stimulation of the left vagus nerve is designed to treat medically refractory epilepsy. VNS has recently been introduced and approved by the FDA as an adjunctive therapy for treatment-resistant major depression. Policy/Criteria I. It is the policy of health plans affiliated with Centene Corporation® that VNS is medically necessary in patients with medically refractory seizures who meet all of the following: A. Diagnosis of focal onset (formerly partial onset) seizures or generalized onset seizures; B. Intractable epilepsy (both): 1. Failure of at least 1 year of adherent therapy of at least two anti-seizure drugs; 2. Continued seizures which have a major impact on activities of daily living; C. Not a suitable candidate for or has failed resective epilepsy surgery; D. Request is for an FDA-approved device. II. It is the policy of health Plans affiliated with Centene Corporation that the safety and efficacy of VNS therapy has not been proven for any other conditions, including but not limited to the following: A. Refractory (treatment resistant) major depression or bipolar disorder; B. Obesity; C. -

Vagus Nerve Stimulation Therapy for the Treatment of Seizures in Refractory Postencephalitic Epilepsy: a Retrospective Study
fnins-15-685685 August 14, 2021 Time: 15:43 # 1 ORIGINAL RESEARCH published: 19 August 2021 doi: 10.3389/fnins.2021.685685 Vagus Nerve Stimulation Therapy for the Treatment of Seizures in Refractory Postencephalitic Epilepsy: A Retrospective Study Yulin Sun1,2†, Jian Chen1,2†, Tie Fang3†, Lin Wan1,2, Xiuyu Shi1,2,4, Jing Wang1,2, Zhichao Li1,2, Jiaxin Wang1,2, Zhiqiang Cui5, Xin Xu5, Zhipei Ling5, Liping Zou1,2 and Guang Yang1,2,4* 1 Department of Pediatrics, Chinese PLA General Hospital, Beijing, China, 2 Department of Pediatrics, The First Medical Center, Chinese PLA General Hospital, Beijing, China, 3 Department of Functional Neurosurgery, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, China, 4 The Second School of Clinical Medicine, Southern Medical University, Guangzhou, China, 5 Department of Neurosurgery, Chinese PLA General Hospital, Beijing, China Edited by: Eric Meyers, Background: Vagus nerve stimulation (VNS) has been demonstrated to be safe and Battelle, United States effective for patients with refractory epilepsy, but there are few reports on the use of Reviewed by: VNS for postencephalitic epilepsy (PEE). This retrospective study aimed to evaluate the Sabato Santaniello, University of Connecticut, efficacy of VNS for refractory PEE. United States Ismail˙ Devecïoglu,˘ Methods: We retrospectively studied 20 patients with refractory PEE who underwent Namik Kemal University, Turkey VNS between August 2017 and October 2019 in Chinese PLA General Hospital *Correspondence: and Beijing Children’s Hospital. VNS efficacy was evaluated based on seizure Guang Yang reduction, effective rate (percentage of cases with seizure reduction ≥ 50%), McHugh [email protected] classification, modified Early Childhood Epilepsy Severity Scale (E-Chess) score, and †These authors have contributed equally to this work Grand Total EEG (GTE) score. -

7.01.20 Vagus Nerve Stimulation
MEDICAL POLICY – 7.01.20 Vagus Nerve Stimulation BCBSA Ref. Policy: 7.01.20 Effective Date: May 1, 2021 RELATED MEDICAL POLICIES: Last Revised: May 19, 2021 2.01.526 Transcranial Magnetic Stimulation as a Treatment of Depression and Replaces: N/A Other Psychiatric/Neurologic Disorders 7.01.63 Deep Brain Stimulation 7.01.143 Responsive Neurostimulation for the Treatment of Refractory Focal Epilepsy 7.01.516 Bariatric Surgery 7.01.522 Gastric Electrical Stimulation 7.01.546 Spinal Cord and Dorsal Root Ganglion Stimulation Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction The vagus nerve starts in the brain stem and runs down the neck, into the chest, and then down to the stomach area. Stimulating this nerve has been studied as a way to treat several different types of conditions. A small device that generates electricity is surgically placed in a person’s chest. A thin wire leads from the device to the vagus nerve. Vagus nerve stimulation may be used to treat seizures that don’t respond to medication. However, for other conditions it’s considered investigational (unproven). There is not yet enough information in published medical studies to show how well it works for other conditions. Similarly, non-implanted devices to stimulate the vagus nerve for treatment of any condition are also investigational due to lack of evidence that they improve one’s health. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. -

Effects of 12 Months of Vagus Nerve Stimulation in Treatment-Resistant Depression: a Naturalistic Study" (2005)
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln U.S. Department of Veterans Affairs Staff Publications U.S. Department of Veterans Affairs 2005 Effects of 12 Months of Vagus Nerve Stimulation in Treatment- Resistant Depression: A Naturalistic Study A. John Rush University of Texas Southwestern Medical Center, [email protected] Harold A. Sackeim New York State Psychiatric Institute, [email protected] Lauren B. Marangell Baylor College of Medicine Mark S. George Medical University of South Carolina Stephen K. Brannan Cyberonics Inc. See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/veterans Rush, A. John; Sackeim, Harold A.; Marangell, Lauren B.; George, Mark S.; Brannan, Stephen K.; Davis, Sonia M.; Lavori, Phil; Howland, Robert; Kling, Mitchel A.; Rittberg, Barry; Carpenter, Linda; Ninan, Philip; Moreno, Francisco; Schwartz, Thomas; Conway, Charles; Burke, Michael; and Barry, John J., "Effects of 12 Months of Vagus Nerve Stimulation in Treatment-Resistant Depression: A Naturalistic Study" (2005). U.S. Department of Veterans Affairs Staff Publications. 69. https://digitalcommons.unl.edu/veterans/69 This Article is brought to you for free and open access by the U.S. Department of Veterans Affairs at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in U.S. Department of Veterans Affairs Staff Publications by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors A. John Rush, Harold A. Sackeim, Lauren B. Marangell, Mark S. George, Stephen K. Brannan, Sonia M. Davis, Phil Lavori, Robert Howland, Mitchel A. Kling, Barry Rittberg, Linda Carpenter, Philip Ninan, Francisco Moreno, Thomas Schwartz, Charles Conway, Michael Burke, and John J. -

Glossopharyngeal and Vagal Neuralgia
BRITISH 26 August 1967 MEDICAL JOURNAL 529 Br Med J: first published as 10.1136/bmj.3.5564.529 on 26 August 1967. Downloaded from Glossopharyngeal and Vagal Neuralgia JAGDISH C. CHAWLA,* F.R.C.S.; MURRAY A. FALCONERt M.CH. F.R.C.S. Brit. med. J., 1967, 3, 529-531 Tic douloureux involving the glossopharyngeal nerve is rare (1945) did record two cases in which, after intracranial section and when it does occur probably often involves the vagus nerve of the glossopharyngeal nerve alone, pain persisted, but it as well. Many cases are undoubtedly not recognized, and yet disappeared after a second operation in which the upper vagal the condition responds favourably and permanently to intra- rootlets were cut, an experience which Bohm and Strang (1962) cranial section of the glossopharyngeal nerve and upper fila- also shared. Wilson and McAlpine (1946) reported a single ments of the vagus nerve. We therefore propose to review the case in which the glossopharyngeal nerve had been dissected in literature, discuss our own experiences, and try to clarify the its tonsillar bed and avulsed with relief. Our experience, how- clinical syndromes that this condition presents and the surgical ever, suggests that recurrence can arise after this procedure, approach that is required. and has led us to recommend intracranial section of the glosso- pharyngeal nerve plus section of the upper two vagal rootlets. Review of the Literature Present Series The condition of glossopharyngeal neuralgia was first described by Weisenburg (1910), who recognized it in a patient This study is based on a review of 10 patients admitted to with a tumour of the cerebellopontine angle. -

Vagal Nerve Stimulation for Epilepsy and Depression
Vagal Nerve Stimulation for Epilepsy and Depression Draft key questions: public comment and response November 13, 2019 Health Technology Assessment Program (HTA) Washington State Health Care Authority PO Box 42712 Olympia, WA 98504-2712 (360) 725-5126 www.hca.wa.gov/hta [email protected] Vagal Nerve Stimulation for Epilepsy and Depression Draft Key Questions Public Comment and Response Provided by: Center for Evidence-based Policy Oregon Health & Science University November 13, 2019 WA Health Technology Assessment November 13, 2019 Responses to Public Comment on Draft Key Questions The Center for Evidence-based Policy is an independent vendor contracted to produce evidence assessment reports for the Washington Health Technology Assessment (HTA) program. For transparency, all comments received during the public comment periods are included in this response document. Comments related to program decisions, process, or other matters not pertaining to the evidence report are acknowledged through inclusion only. Draft key question document comments received: Edward J. Novotny, Jr., Head, Epilepsy Program, Seattle Children's Hospital, Professor of Neurology, University of Washington, and Chair, Professional Advisory Board of Epilepsy Foundation of Washington Eliza Hagen, U.S. Medical Director, and Ryan Verner, Medical Affairs and Research Manager, Neuromodulation, LivaNova Nicole Curtis, patient Specific responses pertaining to submitted comments are shown in Table 1. Vagal nerve stimulation for epilepsy and depression: draft key questions -

Practical Approaches to Dysphagia Caused by Esophageal Motor Disorders Amindra S
Practical Approaches to Dysphagia Caused by Esophageal Motor Disorders Amindra S. Arora, MB BChir and Jeffrey L. Conklin, MD Address nonspecific esophageal motor disorders (NSMD), diffuse Division of Gastroenterology and Hepatology, Mayo Clinic, esophageal spasm (DES), nutcracker esophagus (NE), 200 First Street SW, Rochester, MN 55905, USA. hypertensive lower esophageal sphincter (hypertensive E-mail: [email protected] LES), and achalasia [1••,3,4••,5•,6]. Out of all of these Current Gastroenterology Reports 2001, 3:191–199 conditions, only achalasia can be recognized by endoscopy Current Science Inc. ISSN 1522-8037 Copyright © 2001 by Current Science Inc. or radiology. In addition, only achalasia has been shown to have an underlying distinct pathologic basis. Recent data suggest that disorders of esophageal motor Dysphagia is a common symptom with which patients function (including LES incompetence) affect nearly present. This review focuses primarily on the esophageal 20% of people aged 60 years or over [7••]. However, the motor disorders that result in dysphagia. Following a brief most clearly defined motility disorder to date is achalasia. description of the normal swallowing mechanisms and the Several studies reinforce the fact that achalasia is a rare messengers involved, more specific motor abnormalities condition [8•,9]. However, no population-based studies are discussed. The importance of achalasia, as the only exist concerning the prevalence of most esophageal motor pathophysiologically defined esophageal motor disorder, disorders, and most estimates are derived from people with is discussed in some detail, including recent developments symptoms of chest pain and dysphagia. A recent review of in pathogenesis and treatment options. Other esophageal the epidemiologic studies of achalasia suggests that the spastic disorders are described, with relevant manometric worldwide incidence of this condition is between 0.03 and tracings included.