Fascial Dysfunction As Origin of Myoskeletal Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Back-To-Basics: the Intricacies of Muscle Contraction
Back-to- MIOTA Basics: The CONFERENCE OCTOBER 11, Intricacies 2019 CHERI RAMIREZ, MS, of Muscle OTRL Contraction OBJECTIVES: 1.Review the anatomical structure of a skeletal muscle. 2.Review and understand the process and relationship between skeletal muscle contraction with the vital components of the nervous system, endocrine system, and skeletal system. 3.Review the basic similarities and differences between skeletal muscle tissue, smooth muscle tissue, and cardiac muscle tissue. 4.Review the names, locations, origins, and insertions of the skeletal muscles found in the human body. 5.Apply the information learned to enhance clinical practice and understanding of the intricacies and complexity of the skeletal muscle system. 6.Apply the information learned to further educate clients on the importance of skeletal muscle movement, posture, and coordination in the process of rehabilitation, healing, and functional return. 1. Epithelial Four Basic Tissue Categories 2. Muscle 3. Nervous 4. Connective A. Loose Connective B. Bone C. Cartilage D. Blood Introduction There are 3 types of muscle tissue in the muscular system: . Skeletal muscle: Attached to bones of skeleton. Voluntary. Striated. Tubular shape. Cardiac muscle: Makes up most of the wall of the heart. Involuntary. Striated with intercalated discs. Branched shape. Smooth muscle: Found in walls of internal organs and walls of vascular system. Involuntary. Non-striated. Spindle shape. 4 Structure of a Skeletal Muscle Skeletal Muscles: Skeletal muscles are composed of: • Skeletal muscle tissue • Nervous tissue • Blood • Connective tissues 5 Connective Tissue Coverings Connective tissue coverings over skeletal muscles: .Fascia .Tendons .Aponeuroses 6 Fascia: Definition: Layers of dense connective tissue that separates muscle from adjacent muscles, by surrounding each muscle belly. -

A Device to Measure Tensile Forces in the Deep Fascia of the Human Abdominal Wall
A Device to Measure Tensile Forces in the Deep Fascia of the Human Abdominal Wall Sponsored by Dr. Raymond Dunn of the University of Massachusetts Medical School A Major Qualifying Report Submitted to the Faculty Of the WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of the requirements for the Degree of Bachelor of Science By Olivia Doane _______________________ Claudia Lee _______________________ Meredith Saucier _______________________ April 18, 2013 Advisor: Professor Kristen Billiar _______________________ Co-Advisor: Dr. Raymond Dunn _______________________ Table of Contents Table of Figures ............................................................................................................................. iv List of Tables ................................................................................................................................. vi Authorship Page ............................................................................................................................ vii Acknowledgements ...................................................................................................................... viii Abstract .......................................................................................................................................... ix Chapter 1: Introduction ................................................................................................................... 1 Chapter 2: Literature Review ......................................................................................................... -

Fascial Contraction Fascia Can Be Divided Into Two General Categories: Sub Cutaneous Fascia and Deep Fascia, Also Known As Muscu Lar Fascia
by joe muscolino body mechanics Bodywork and movement therapy can help with contracted fascial tissue. fascial contraction Fascia can be divided into two general categories: sub- examples of deep fibrous fascia, as cutaneous fascia and deep fascia, also known as muscu- are ligaments and intermuscular lar fascia. Subcutaneous fascia, as the name implies, is septa. The loosely packed struc- located immediately deep to the skin. It is largely com- ture of subcutaneous fascia allows www.amtamassage.org/mtj posed of adipose (fat) cells, giving it its gel-like consis- for a healthy blood supply, giving it tency. Collagen fibers and fibroblast cells are embedded strong reparative properties when within this mix of adipose cells. Deep fascia is located injured. Alternatively, the dense ar- deeper in the body and is primarily comprised of dense- rangement of fibrous fascia does not ly packed collagen fibers, accounting for its description allow adequate room for blood ves- as fibrous fascia. Fibroblasts are located between these sels; therefore, fibrous fascia has a collagen fibers (Figure 1). poor blood supply and does not heal Endomysium, perimysium and epimysium, which well when injured. In addition to 145 create the tendons and aponeuroses of muscles, are collagen fibers and fibroblasts, both body mechanics Recent research suggests that fascia does and stretched, having the ability to transfer these pull- ing forces to other tissues. For example, when a muscle not function only in a belly contracts and pulls upon its tendons, these fibrous passive tensile manner, tissue tendons transfer that pulling force to the bony at- tachments of the muscle. -

Biology 218 – Human Anatomy RIDDELL
Biology 218 – Human Anatomy RIDDELL Chapter 10 Adapted form Tortora 10th ed. LECTURE OUTLINE A. Introduction (p. 265) 1. Bones provide leverage and form the framework of the body, but motion results from alternating contraction (shortening) and relaxation of muscles. 2. Muscle tissue also stabilizes the body’s position, regulates organ volume, generates heat, and propels fluids and food through various body systems. 3. The study of muscles is called myology. B. Overview of Muscle Tissue (p. 266) 1. There are three types of muscle tissue (see Table 10.2): i. Skeletal muscle tissue a. moves bones (and, in some cases, skin and other soft tissues) b. striated c. voluntary ii. Cardiac muscle tissue a. forms most of the wall of the heart b. striated c. involuntary d. some cells have autorhythmicity iii. Smooth muscle tissue a. located in the walls of hollow internal structures (and arrector pili muscles) b. nonstriated, i.e., smooth c. involuntary d. some cells have autorhythmicity 2. Muscle tissue has four major functions: i. producing body movements ii. stabilizing body positions iii. storing and moving substances within the body iv. producing heat 3. Muscle tissue has four major characteristics that enable it to perform its functions: i. Electrical excitability is the ability to respond to certain stimuli by producing electrical signals called action potentials (impulses) ii. Contractility is the ability to shorten, thus developing tension (force of contraction) a. in an isometric contraction, a muscle develops tension but does not shorten b. in an isotonic contraction, tension remains relatively constant while the muscle shortens iii. -

Histological Characteristics of the Deep Fascia of the Upper Limb
it. j. anat. embryol. Vol. 111, n. 2: 105-110, 2006 Histological characteristics of the deep fascia of the upper limb Carla Stecco 1,2 M.D., Andrea Porzionato 1 M.D., Veronica Macchi 1 M.D., Cesare Tiengo 1 M.D., Anna Parenti 3 M.D., Roberto Aldegheri 2 M.D., Vincent Delmas 4 M.D. and Raffaele De Caro 1 M.D. 1 Section of Anatomy, Department of Human Anatomy and Physiology, University of Padova, Italy 2 Section of Orthopedics, Department of Medical Surgical Specialities, University of Padova, Italy 3 Section of Pathologic Anatomy, Department of Oncological and Surgical Sciences, University of Padova, Italy 4 Normal Anatomy Institute, Rene´Descartes University, Paris Key words: fascia, collagen, proprioception, myokinetic chain, motor coordination, over-use syndrome. SUMMARY Post-mortem specimens taken from the antebrachial and brachial fasciae of 20 upper limbs were studied by histological and immunohistochemical staining in order to evaluate collagen fibre bundle arrangement, the presence of elastic fibres, and the density of innervation in deep muscular fascia. The study demonstrated that the fasciae are formed of numerous layers of undulating colla- gen fibre bundles. In each layer, the bundles are parallel to each other, whereas adjacent layers show different orientations. Each layer is separated from the adjacent one by a thin layer of adipose tissue, like plywood. Many elastic fibres and a variety of both free and encapsulated nerve endings, espe- cially Ruffini and Pacini corpuscles, are also present, suggesting a proprioceptive capacity of the deep fascia. Thanks to the undulating collagen fibre bundles and elastic fibres, the fasciae can adapt to stretching, but this is only possible within certain limits, beyond which nerve terminations are acti- vated by stretching. -

Evidence of a New Hidden Neural Network Into Deep Fasciae
www.nature.com/scientificreports OPEN Evidence of a new hidden neural network into deep fasciae Caterina Fede1,2*, Lucia Petrelli1,2, Diego Guidolin1, Andrea Porzionato1, Carmelo Pirri1, Chenglei Fan1, Rafaele De Caro1 & Carla Stecco1 It is recognized that diferent fasciae have diferent type of innervation, but actually nothing is known about the specifc innervation of the two types of deep fascia, aponeurotic and epymisial fascia. In this work the aponeurotic thoracolumbar fascia and the epymisial gluteal fascia of seven adult C57-BL mice were analysed by Transmission Electron Microscopy and foating immunohistochemistry with the aim to study the organization of nerve fbers, the presence of nerve corpuscles and the amount of autonomic innervation. The antibodies used were Anti-S100, Anti-Tyrosine Hydroxylase and Anti- PGP, specifc for the Schwann cells forming myelin, the sympathetic nerve fbers, and the peripheral nerve fbers, respectively. The results showed that the fascial tissue is pervaded by a rhomboid and dense network of nerves. The innervation was statistically signifcantly lower in the gluteal fascia (2.78 ± 0.6% of positive area, 140.3 ± 31.6/mm2 branching points, nerves with 3.2 ± 0.6 mm length and 4.9 ± 0.2 µm thickness) with respect to the thoracolumbar fascia (9.01 ± 0.98% of innervated area, 500.9 ± 43.1 branching points/mm2, length of 87.1 ± 1.0 mm, thickness of 5.8 ± 0.2 µm). Both fasciae revealed the same density of autonomic nerve fbers (0.08%). Lastly, corpuscles were not found in thoracolumbar fascia. Based on these results, it is suggested that the two fasciae have diferent roles in proprioception and pain perception: the free nerve endings inside thoracolumbar fascia may function as proprioceptors, regulating the tensions coming from associated muscles and having a role in nonspecifc low back pain, whereas the epymisial fasciae works to coordinate the actions of the various motor units of the underlying muscle. -

Fascial Anatomy in Manual Therapy: Introducing a New Biomechanical Julie Ann Day, PT Model
Fascial Anatomy in Manual Therapy: Introducing a New Biomechanical Julie Ann Day, PT Model Centro Socio Sanitario dei Colli, Physiotherapy, Padova, Italy ABSTRACT detailed studies pertaining to specific areas suggested.17 Deep fascia is a well-vascular- Background and Purpose: Fascial of fascia are important, they do not pro- ized tissue often employed for plastic sur- anatomy studies are influencing our under- vide a vision of the human fascial system as gery flaps,18 and it responds to mechanical standing of musculoskeletal dysfunctions. an interrelated, tensional network of con- traction induced by muscular activity in dif- However, evidenced-based models for nective tissue. A few authors consider its ferent regions.19 It has an ectoskeletal role manual therapists working with move- 3-dimensional (3D) continuity8-10 but these and can potentially store mechanical energy ment dysfunction and pain are still devel- holistic models do not always provide spe- and distribute it in a uniform manner for oping. This review presents a synthesis of cific indications for treatment. A functional harmonious movement. The mechanical one biomechanical model and discusses model for the entire human fascial system properties of the fascial extracellular matrix underlying hypotheses in reference to some that correlates dysfunctional movement itself can be altered by external mechanical current trends in musculoskeletal research. and pain is in its infancy with regards to stimuli that stimulate protein turnover and Method: The author conducted principally evidence-based investigations and studies. fibroblastic activity.20,21 These characteris- a search of the health sciences literature This paper will examine a 3D bio- tics and the reported abundant innervation available on PubMed for the years 1995 to mechanical model for the human fascial of deep fascia indicate that it could have 2011, and consulted published texts con- system that takes into account movement the capacity to perceive mechanosensitive cerning this model. -

Superficial Fascia • Fascia Can Be Divided Into Different Types
Fascia The Under Appreciated Tissue Skin (Integument) Overview of the Skin • Largest organ of the body (15% of body weight) • Skin thickness variable, normally 1‐2 mm • Protection – chemical barrier (waterproof) – physical barrier (tough) – immune system activator • Body temperature regulation – blood flow through the skin – sweat glands – hairs • Sensation – sense touch, temperature and pain • provides information outside of the body Assessment of Skin Color • Cyanosis is a bluish discoloration of the skin or mucous membranes •caused by lack of oxygen in the blood. • Yellowish color •may indicate cirrhosis of the liver due to accumulating bile pigments in body tissue • Pallor or Blanching: •can be sign of anemia or emotional or physical stress • Black and Blues: •Bruises caused by blood escapes circulation and clots underneath the skin. • Red color( erythema) • indicate fever, allergy, infection inflammation and embarrassment. Fascia • Connective tissues that plays an important role in human function. – 16% of total body weight and stores 23% of total water composition • It connects all the tissues of the human body together including the muscles, organs nerves and vessels of the body. • Fascia is a dynamic connective tissue that changes based on the stresses placed on it. Roles of Fascia • The fascia plays a major role in circulation of blood and lymph. – The fascia is important for the nutrition and metabolism of every cell in the body. ( vise versa) • The fascia is the first line of defense in immune function. • Disruptions and restrictions within the fascia are associated with disease and movement impairments. – Interrupts the flow of blood and lymph – Can cause pain and poor compensatory patterns. -

Tendon Fascia Continuity, the Glenoid Labrum: an Adaptable Dynamic Ring
Tendon fascia continuity, the glenoid labrum: An adaptable dynamic ring Karl Jacobs - University of applied science Amsterdam / University of Amsterdam Introduction/Background Traditionally the glenoid labrum, the tendon of the long head of biceps and triceps have all been discussed as independent anatomical structures in their own right. Traditional literature has approached these structures as being unique entities (1), which inadequately explains the functional stability of the shoulder and is at odds with findings on dissection. This research aims to explain the functional anatomy of the shoulder joint by demonstrating that the glenoid labrum and the tendons of the long heads of the biceps and triceps is a continuous fascial structure. The results provide new insights in explaining the stabilising abilities of the shoulder joint as a consequence of tendon fascia continuity. Methods Dissection was performed, respecting fascia continuity, on a formalin-fixed female cadaver, with no known medical history. The glenoid labrum has a vital role in shoulder joint stability; this region was dissected to establish whether the “labrum” acts as a single structure or as a continuum, formed by the tendons of the long heads of the biceps and triceps. Results A continuation of tendon fascia was identified, starting from the tendon of the long head of the Biceps through the glenoid labrum and towards the tendon of the long head of the triceps. This continuity is a result of the continuation of the fascicular investing muscular fascia (endo, peri, epi, -mysium) with its tendon (endo, peri, para -tendon) fascia. This continuity, instead of continuing within adjacent muscle or bone, continues within the glenoid labrum creating a dynamic ring. -

Fascia: a Morphological Description and Classification System Based on a Literature Review Myroslava Kumka, MD, Phd* Jason Bonar, Bsckin, DC
0008-3194/2012/179–191/$2.00/©JCCA 2012 Fascia: a morphological description and classification system based on a literature review Myroslava Kumka, MD, PhD* Jason Bonar, BScKin, DC Fascia is virtually inseparable from all structures in Le fascia est pratiquement inséparable de toutes les the body and acts to create continuity amongst tissues structures du corps, et il sert à créer une continuité to enhance function and support. In the past fascia entre les tissus afin d’en améliorer la fonction et le has been difficult to study leading to ambiguities in soutien. Il a déjà été difficile d’étudier le fascia, ce qui nomenclature, which have only recently been addressed. a donné lieu à des ambiguïtés dans la nomenclature, Through review of the available literature, advances qui n’ont été abordées que récemment. Grâce à un in fascia research were compiled, and issues related examen de la documentation disponible, les avancées to terminology, descriptions, and clinical relevance of dans la recherche sur le fascia ont été compilées, fascia were addressed. Our multimodal search strategy et les problèmes relevant de la terminologie, des was conducted in Medline and PubMed databases, with descriptions et de la pertinence clinique du fascia ont été other targeted searches in Google Scholar and by hand, traités. Nous avons adopté une stratégie de recherche utilizing reference lists and conference proceedings. multimodale pour nos recherches dans les bases de In an effort to organize nomenclature for fascial données Medline et PubMed, avec des recherches ciblées structures provided by the Federative International dans Google Scholar et manuelles, au moyen de listes de Committee on Anatomical Terminology (FICAT), we références et de comptes rendus de congrès. -

Characteristics of Fascia in Reference to Treatment Possibilities of Chosen Hand Diseases
Mini Review ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2020.29.004874 Characteristics of Fascia in Reference to Treatment Possibilities of Chosen Hand Diseases Alicja Jurecka1*, Maciej Papież2 and Artur Gądek1 1Jagiellonian University Medical College, Faculty of Health Sciences, Department of Orthopedics and Physiotherapy, Poland 2Emirates Specialty Hospital, Dubai Healthcare City, Dubai *Corresponding author: Alicja Jurecka, Jagiellonian University Medical College, Faculty of Health Sciences, Department of Orthopedics and Physiotherapy, Poland ARTICLE INFO ABSTRACT Received: August 13, 2020 The patomechanism of changes encountered in many movement system dysfunctions gives a basis for applying manual techniques, which have an impact on fascia’s structure, Published: August 31, 2020 onKeywords: treatment Fascia; of chosen Orthopedics; orthopedics Hand afflictions. diseases; Myofascial therapy; Physiotherapy Citation: Reference Alicjato Treatment Jurecka, PossibilitiesMaciej Papież, of ChosenArtur Gądek. Hand Diseases.Characteristics Biomed of J SciFascia & Tech in Res 29(5)-2020. BJSTR. MS.ID.004874. Introduction and plastic, and also resistant to mechanic stimulus. The current An architecture of fascia and its precise connections with many od movement system components creates a basis for putting transmission [5]. Collagen layers of the fascia are separated from forward presumptions of prospects of applying a fascial modelling definition of the fascia emphasizes its meaning in tensional force each other by fatty tissue [2]. The outermost layer of the fascia is Three-dimensional fascial web covers and penetrates such as an important element in many orthopedic afflictions treatment. is the investing fascia, also known as the deep fascia [6]. The structures as: muscles, intermuscular septum’s, tendons, ligaments, known as pinnacular or superficial. -
Microsoft Powerpoint
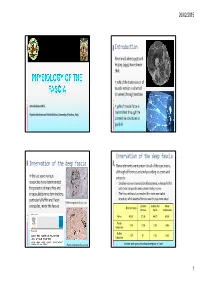
26/02/2015 Introduction Patel and Lieber (1997) and Huijing (1999) have shown that: 70% of the transmission of muscle tension is directed (in series) through tendons Antonio Stecco M.D. 30% of muscle force is Physical Medicine and Rehabilitation, University of Padova, Italy transmitted through the connective structures in parallel Innervation of the deep fascia Innervation of the deep fascia . Nerve elements were present in all of the specimens, although differences existed according to zones and In the last years various subjects: researches have demonstrated Small nerves were revealed in all specimens, whereas Ruffini the presence of many free and and Pacini corpuscles were present only in some. encapsulated nerve terminations, The flexor retinaculum resulted the more innervated particularly Ruffini and Pacini structure, while lacertus fibrosus was the less innervated Ruffini corpuscles (S100, 200x) Lacertus Antibrachial Flexor corpuscles, inside the fasciae Brachial fascia fibrosus fascia retinaculum Nerve 48.57 27.36 44.37 53.55 Pacini 0.43 0.26 0.26 0.66 Corpuscle Ruffini 0.29 0.1 0.26 0.55 Corpuscle 2 Pacini corpuscles (S100, 100x) Number and types of mechanoreceptors in 1 cm 1 26/02/2015 Relationships among nerves and fascia Large nerve fibres and deep fascia The capsules of the corpuscles and the free nerve The larger nerve fibres are often endings are connected to the surrounding collagen fibres surrounded by different layers of loose connective tissue that preserves the nerve from traction Stretching of the deep fascia