Clinicopathological Correlation of Serum Ascites Albumin Gradient With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines on the Diagnosis and Management of Pericardial
European Heart Journal (2004) Ã, 1–28 ESC Guidelines Guidelines on the Diagnosis and Management of Pericardial Diseases Full Text The Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology Task Force members, Bernhard Maisch, Chairperson* (Germany), Petar M. Seferovic (Serbia and Montenegro), Arsen D. Ristic (Serbia and Montenegro), Raimund Erbel (Germany), Reiner Rienmuller€ (Austria), Yehuda Adler (Israel), Witold Z. Tomkowski (Poland), Gaetano Thiene (Italy), Magdi H. Yacoub (UK) ESC Committee for Practice Guidelines (CPG), Silvia G. Priori (Chairperson) (Italy), Maria Angeles Alonso Garcia (Spain), Jean-Jacques Blanc (France), Andrzej Budaj (Poland), Martin Cowie (UK), Veronica Dean (France), Jaap Deckers (The Netherlands), Enrique Fernandez Burgos (Spain), John Lekakis (Greece), Bertil Lindahl (Sweden), Gianfranco Mazzotta (Italy), Joa~o Morais (Portugal), Ali Oto (Turkey), Otto A. Smiseth (Norway) Document Reviewers, Gianfranco Mazzotta, CPG Review Coordinator (Italy), Jean Acar (France), Eloisa Arbustini (Italy), Anton E. Becker (The Netherlands), Giacomo Chiaranda (Italy), Yonathan Hasin (Israel), Rolf Jenni (Switzerland), Werner Klein (Austria), Irene Lang (Austria), Thomas F. Luscher€ (Switzerland), Fausto J. Pinto (Portugal), Ralph Shabetai (USA), Maarten L. Simoons (The Netherlands), Jordi Soler Soler (Spain), David H. Spodick (USA) Table of contents Constrictive pericarditis . 9 Pericardial cysts . 13 Preamble . 2 Specific forms of pericarditis . 13 Introduction. 2 Viral pericarditis . 13 Aetiology and classification of pericardial disease. 2 Bacterial pericarditis . 14 Pericardial syndromes . ..................... 2 Tuberculous pericarditis . 14 Congenital defects of the pericardium . 2 Pericarditis in renal failure . 16 Acute pericarditis . 2 Autoreactive pericarditis and pericardial Chronic pericarditis . 6 involvement in systemic autoimmune Recurrent pericarditis . 6 diseases . 16 Pericardial effusion and cardiac tamponade . -

Hepatic Hydrothorax Without Apparent Ascites and Dyspnea - a Case Report
Case Report DOI: 10.7860/JCDR/2018/37185.12181 I nternal Medicine Hepatic Hydrothorax without Apparent S ection Ascites and Dyspnea - A Case Report JING HE1, RASHA HAYKAL2, HONGCHUAN COVILLE3, JAYA PRAKASH GADIKOTA4, CHRISTOPHER BRAY5 ABSTRACT A 78-year-old female with a past medical history of alcoholic cirrhosis was hospitalised with recurrent lower gastrointestinal bleeding due to rectal ulcers. The ulcers were successfully treated with cautery and placement of clips. However, a recurrent large right-sided pleural effusion without apparent ascites and dyspnea were found incidentally during the hospitalisation. The initial fluid analysis was exudate based on Light’s criteria with high protein. The fluid analysis was repeated five days later, after rapid reaccumulation which revealed transudates. Other causes of pleural effusion like heart failure, renal failure or primary pulmonary diseases were excluded. Hepatic hydrothorax was considered and the patient was started with the treatment of Furosemide and Spironolactone. The atypical presentation of hepatic hydrothorax may disguise the diagnosis and delay the treatment. Therefore, for a patient with recurrent, unexplained unilateral pleural effusions, even with atypical fluid characterisation and in the absence of ascites, hepatic hydrothorax should still remain on the top differential with underlying cirrhosis to ensure optimal treatment. Keywords: Cirrhosis, Light criteria, Liver, Pleural effusion CASE REPORT Haemogram Levels Normal range A 78-year-old Caucasian female, with a past medical history of alcoholic cirrhosis, admitted for recurrent rectal bleeding secondary WBC 6.9 (4.5-11.0 thousands/mm3) to rectal ulcers and was successfully treated with cautery and Neutrophils % 78 H (50.0-75.0 %) placement of clips. -

Assessing Acute Collapse for Presentation Powerpoint and Handouts
“I’ve Fallen and [email protected] I Can’t Get Up” Assessing Acute Collapse For Presentation PowerPoint and Handouts: http://wendyblount.com Wendy Blount, DVM Kinds of Shock [email protected] Anaphylactic Shock •Obstructed airway •Acute allergic reaction •Lung Disease •Mast Cell Tumor Degranulation •Pleural air or effusion Cardiovascular Shock Neurogenic shock •Arrhythmia •Forebrain and brainstem - For Presentation PowerPoint •Left Heart Failure decreased consciousness •Right Heart Failure •Spinal cord – flaccid paralysis and Handouts: •Pericardial Disease Septic Shock http://wendyblount.com Hypovolemic Shock •Overwhelming infection •Dehydration Traumatic Shock •Hemorrhage •Due to pain •Hypoproteinemia Toxic Shock Hypoxic Shock •Due to inflammatory mediators, •Anemia endogenous and exogenous •Hemoglobin Pathology toxins Collapse Other Than Shock Assessment of Inability or Unwillingness to get up Collapse Profound Weakness Ataxia – lack of coordination •Metabolic weakness •Vestibular ataxia Quick Assessment •Hypercalcemia •Cerebellar ataxia Life Saving Treatment •Hypokalemia •Sensory ataxia •Hypoglycemia Paresis - loss of voluntary Physical Exam •Neurotoxins motor Emergency Diagnostics •Polyneuropathy •Lower Motor Neuron •Junctionopathy •CNS Lesion at level of History •Myopathy paresis Pain •Flaccid paresis In House Diagnostics •Spinal Cord/Nerve Pain •Upper Motor Neuron •Orthopedic Pain •CNS Lesion above paresis •Muscular Pain •Spastic paresis 1 Assessment of Assessment of Collapse Collapse Quick Assessment Life Saving Treatment -

6. Fluid and Hemodynamic Disorders
6. Fluid and hemodynamic disorders Background Total Body Water [Fig. 6-1] • Human body is 60 % fluid (water) by weight – Total Body Water (TBW) = 42 liters (70kg M) • Body has two major compartments (inside cell or outside) • 2/3 of TBW is located inside cells – intracellular fluid compartment [28 l] • 1/3 of TBW is located outside cells – extra-cellular fluid compartment [14 l] • 1/4 ECF is located inside blood vessels (intra-vascular) [3.5 l] • 3/4 ECF is located in extra-vascular (interstitial) space [9.5 l] Movement of fluid • Distribution of water between ICF and ECF compartments is determined by distribution of electrolytes • Distribution of water within the ECF between the intra-vascular and interstitial space is determined by proteins • Fluid constantly moves between compartments – fluid moves out of capillaries due to hydrostatic pressure in the capillary and osmotic pressure in ECF – fluid moves into capillaries due to oncotic pressure in the vessel and hydrostatic pressure in the ECF • Lymphatics remove excess fluid not returned to vessels Fluid and hemodynamic disorders Edema • Edema is the accumulation of excess fluid in ECF space – edema may be localized or systemic – edema fluid may be a Transudate or an Exudate • Exudate – an exudate has a high protein content and lots of white blood cells – an exudate forms due to inflammation • Transudate – a transudate has a low protein content and few white blood cells – a transudate forms due to imbalance of forces across vessel walls • The cause of edema is often multifactorial • Terminology – anasarca is severe generalized edema – ascites is excess fluid in abdominal cavity – hydrothorax is excess fluid in pleural cavity – hydrocardia is excess fluid in pericardial cavity • Edema may have serious consequences – cerebral edema may result in herniation of the brain and death – pulmonary edema may result in impaired air exchange and death Fluid and hemodynamic disorders Edema pathogenesis [Fig. -

Evaluation of Pleural Effusion Type Determination Based on Light's and Heffner's Criteria
PAGE 76 2019 Nov; 26(1): 1-128 p-ISSN 0854-4263 e-ISSN 2477-4685 Available at www.indonesianjournalofclinicalpathology.org EVALUATION OF PLEURAL EFFUSION TYPE DETERMINATION BASED ON LIGHT'S AND HEFFNER'S CRITERIA Nordjannah1, Ani Kartini2, Darmawaty ER3 1 Specialization Program of Medical Pathology, Faculty of Medicine, University of Hassanudin/Dr. Wahidin Sudirohusodo General Hospital, Makassar, Indonesia. E-mail: [email protected] 2 Department of Clinical Pathology, Faculty of Medicine, University of Hassanudin/Labuang Baji Hospital Makassar, Indonesia 3 Department of Clinical Pathology, Faculty of Medicine, University of Hassanudin/Islamic Faisal General Hospital, Makassar, Indonesia ABSTRACT Pleural effusion is an abnormal accumulation of pleural fluid in the pleural cavity due to excessive transudation or exudation. Light's criteria is used as the standard method to distinguish between exudates and transudates. Some recent studies reported misclassifications which led to development of several alternative criteria, such as Heffner's criteria. The purpose of this study was to determine the sensitivity and specificity of Heffner's criteria to determine the type of pleural effusion. This research was an observational study with a cross-sectional method using a pleural effusion of patients at the Clinical Pathology Laboratory Installation at the Wahidin Sudirohusodo Hospital in July 2018. Total protein, LDH, and cholesterol levels were measured in all samples that met the inclusion and exclusion criteria. There were 45 pleural effusion samples that consisted of 30 transudate and 15 exudate samples. Based on clinical diagnosis, the Light's criteria showed 3 misclassifications and Heffner's criteria obtained showed 2 misclassifications. Based on the data above, the statistical data showed that Light's criteria had a sensitivity of 96.7% and specificity of 86.7%. -

An Unusual Case of Postpartum Anasarca an Unusual Case of Postpartum Anasarca
JSAFOG CASE REPORT An Unusual Case of Postpartum Anasarca An Unusual Case of Postpartum Anasarca 1Jai Inder Singh, 2Randhir Puri, 3KG Kiran 1Major, Graded Specialist, Medicine, Military Hospital, Belgaum, Karnataka, India 2Colonel, Department of Obstetrics and Gynecology, Military Hospital, Belgaum, Karnataka, India 3Colonel, Commanding Officer, Military Hospital, Belgaum, Karnataka, India Correspondence: Major, Jai Inder Singh, Medical specialist, Military Hospital, Belgaum Camp, Karnataka-590009, India Phone: +919343979290, +918312423852, e-mail: [email protected] Abstract A 21-year-old lady, primipara presented with breathlessness on exertion and generalized swelling of three weeks duration. Clinical examination revealed anasarca and features of cardiac failure. After evaluation, a diagnosis of peripartum cardiomyopathy was established based on echocardiographic findings of dilated cardiac chambers and poor left ventricular function. She responded well to treatment. The case is being reported for the diagnostic dilemma and rarity. Keywords: Anasarca, peripartum cardiomyopathy, systolic dysfunction, echocardiography. INTRODUCTION pleural effusion, ascites and mild hepatomegaly. Laboratory examination revealed microcytic hypochromic anemia (Hb = Peripartum cardiomyopathy (PPCM) is a type of dilated 8.2 gm/dl). Urine analysis showed presence of albumin 2 +, 8-10 cardiomyopathy in women with no past history of cardiac pus cells and 4-6 RBC’s/hpf. Twenty four hour urine protein disease and requires a high index of suspicion for diagnosis. was 1.12 gm and urine culture was sterile. Renal/liver function It is a disease of uncertain etiology and can worsen during tests, serum proteins, albumin and cholesterol were within normal future pregnancies. Symptomatic patients should receive limits. Chest X-ray showed cardiomegaly and bilateral pleural therapy for cardiac failure. -

Lymphedema: a Review and Case Profiles October 2004
Lymphedema: A Review and Case Profiles October 2004 Lymphedema of the extremities remains a therapeutic challenge. As a result many different treatments have been devised but none have been routinely effective. Two types of lymphedema occur, primary and secondary. Primary lymphedema is rare, the result of a congenital abnormality of the lymphatic system. Secondary lymphedema, the most common form, may be acute or chronic. It results from obstruction or interruption of the lymphatic channels. Fluids and proteins, transudate from cells or exudate from both lymphatic and vascular channels collects in the superficial connective tissues and fails to be absorbed by the lymphatic system. Duration varies from weeks to years. The acute form generally follows trauma and is easily resolved by conventional methods. The chronic version is a more vexing problem, only minimally improved by existing technologies with rapid recurrence when therapy ceases. Chronic lymphedema most frequently occurs post-mastectomy or subsequent to a variety of other surgical procedures that involve resection of the lymph channels and nodes. It can also be a complication secondary to congestive heart failure, chronic liver disease, thrombophlebitis, systemic infections and gravitational dependency. In its late stages it is characterized by firm induration with accompanying cyanosis as arterial compression occurs. Lymphedema Etiology Acute Chronic • Trauma • Thrombophlebitis • Surgery • Congestive Cardiac Failure • Burns • Immobilization • Dependency • Post Radiation • Renal Failure • Hepatic Disease • Systemic Infection • Developmental Conventional Therapies 1. Elevation of extremity above level of heart 2. Variety of compression techniques Pumps Bandages Fitted garments 3. Manual Procedures Massage Compression It should be noted that there is no effective drug therapy available. -
Unit 3 - Transudates and Exudates
Unit 3 - Transudates and exudates Session 11 Identification, differentiation of transudates and exudates and different examples B.M.C.Randika Wimalasiri B.Sc in MLS(Peradeniya) Lecturer(Probationary) Department of Medical Laboratory Sciences Introduction • Effusions- fluids which accumulate in cavities • Pleural, pericardial, and peritoneal cavities (ascites) • Determine the reason for the accumulation of the fluid. • All effusions are classified as exudates or a transudates 11.1 Definition and identification of transudates and exudates • Classifying help clinicians to determine the disease process responsible for the accumulation of fluid. • Thus, help in treating the disease with the idea of curing or minimizing complications depending on the disease involved. • Outer linings of tissues and organs –protection • Selective membrane permeability allows the transfer of fluids, proteins, and other metabolites that are important in continuing metabolic processes occur inside these organs Transudates • Malfunctioning membranes causes fluid accumulates in the body cavities. • This fluid is referred to as a transudate. • Regulation of amount of fluid in these cavities is done by the lymphatic system. • Malfunctioning of membranes cause transudate formation due to a disease process in an organ or the lymphatic sysem. • Mechanism- disrupt the balance between the formation and its uptake by the lymphatic system causing fluid accumulation in one side of the membrane. • Examples of transudate formation- 1. Liver 2. Pancreas 3. Heart (e.g. congestive heart failure - A weakness of the heart that leads to a buildup of fluid in the lungs and surrounding body tissues). Exudates • An exudate is a fluid with a high content of protein and cellular debris which has escaped from blood vessels and has been deposited in tissues. -

Hepatic Hydrothorax
Hepatic Hydrothorax. , 2018; 17 (1): 33-46 33 CONCISE REVIEW January-February, Vol. 17 No. 1, 2018: 33-46 The Official Journal of the Mexican Association of Hepatology, the Latin-American Association for Study of the Liver and the Canadian Association for the Study of the Liver Hepatic Hydrothorax Yong Lv,* Guohong Han,* Daiming Fan** * Department of Liver Diseases and Digestive Interventional Radiology, National Clinical Research Center for Digestive Diseases and Xijing Hospital of Digestive Diseases, Fourth Military Medical University, Xi'an 710032, China. ** State Key Laboratory of Cancer Biology, National Clinical Research Center for Digestive Diseases and Xijing Hospital of Digestive Diseases, Fourth Military Medical University, Xi'an 710032, China. ABSTRACT Hepatic hydrothorax (HH) is a pleural effusion that develops in a patient with cirrhosis and portal hypertension in the absence of car- diopulmonary disease. Although the development of HH remains incompletely understood, the most acceptable explanation is that the pleural effusion is a result of a direct passage of ascitic fluid into the pleural cavity through a defect in the diaphragm due to the raised abdominal pressure and the negative pressure within the pleural space. Patients with HH can be asymptomatic or present with pulmonary symptoms such as shortness of breath, cough, hypoxemia, or respiratory failure associated with large pleural effusions. The diagnosis is established clinically by finding a serous transudate after exclusion of cardiopulmonary disease and is confirmed by radionuclide imaging demonstrating communication between the peritoneal and pleural spaces when necessary. Spontaneous bacteri- al empyema is serious complication of HH, which manifest by increased pleural fluid neutrophils or a positive bacterial culture and will require antibiotic therapy. -
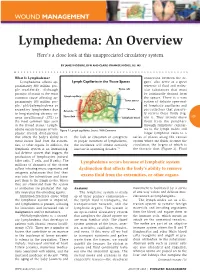
Lymphedema: an Overview Here’S a Close Look at This Unappreciated Circulatory System
WOUND MANAGEMENT Lymphedema: An Overview Here’s a close look at this unappreciated circulatory system. BY JAMES MCGUIRE, DPM AND CLAIRE-IPHANISE MICHEL, BS, MS What Is Lymphedema? connection between the or- Lymphedema affects ap- Lymph Capillaries in the Tissue Spaces gans—also serve as a great proximately 300 million peo- reservoir of fluid and molec- ple worldwide. Although Tissue cells ular substances that must parasitic filariasis is the most be continually drained from common cause affecting ap- Lymph capillary the spaces. There is a vast proximately 100 million peo- Tissue spaces system of delicate open-end- ple,1 phlebolymphedema or ed lymphatic capillaries and Venule secondary lymphedema due Arteriole pre-collectors that passive- to long-standing chronic ve- ly receive these fluids (Fig- Tissue fluid nous insufficiency (CVI) is Lymphatic vessel ure 1). They actively move 109 the most common type seen them from the periphery in the United States.2 Lymph- through lymphatic capillar- edema occurs because of lym- Figure 1: Lymph capillaries. Source: Wiki Commons ies to the lymph nodes and phatic system dysfunction larger lymphatic veins to a that affects the body’s ability to re- the lack of education of caregivers series of places along the venous move excess fluid from the extremi- in proper treatment of lymphedema, system where the fluids re-enter the ties, or other organs. In addition, the the incidence will almost certainly circulation, the largest of which is lymphatic system is an immunolog- increase in upcoming decades.”2 the thoracic duct (Figure 2). Fluid ical defense system that triggers the production of lymphocytes (natural killer cells, T cells, and B cells). -

Differential Diagnosis of Pleural Effusions
Review Article Differential Diagnosis of Pleural Effusions JMAJ 49(9 •10): 315–319, 2006 Tetsuo Sato*1 Abstract A variety of disease states are associated with the development of pleural effusions, which sometimes makes the differential diagnosis problematic. Pleural effusions can be classified into two categories, transudative and exudative, based on the characteristics of the pleural fluid. While transudative effusions are the result of changes in hydrostatic or oncotic pressure with no pathological change in the structure of the pleural membrane or condition of the vascular wall, exudative effusions collect in the pleural cavity as a result of pathological changes or structural breakdown of the pleura. In recent years, Light’s diagnostic criteria have been most commonly used to differentiate between these two categories of pleural effusion and to help delineate the underlying cause, including malignant tumors, infectious diseases (such as tuberculosis), collagen vascular disease, liver disease, pancreatic disease, iatrogenic causes, and gynecological diseases. Pleural mesothelioma secondary to asbestos exposure has been recognized as a cause of pleural effusion, but diagnostic confirmation is difficult in some cases. When pleural effusion cannot be controlled despite treatment of the underlying cause, pleurodesis can be performed as a potentially permanent method of treatment. Key words Pleura, Effusion, Transudate, Exudate, Mesothelioma, Thoracentesis Introduction can go undetected when the pleural effusions are large, CT imaging should be repeated once the A variety of disease states are associated with the fluid has been drained. Further, special attention development of pleural effusions (Table 1), and should be paid to the rate and volume of fluid depending on the disease, the pleural effusion can aspiration during thoracentesis, as rapid or large either exhibit specific or nonspecific characteris- volume drainage may result in re-expansion pul- tics. -

Human Albumin Therapy in Hypoalbuminemic Dogs
OCTOBER 2006 VOL 8.9 Peer Reviewed Editorial Mission Human Albumin Therapy To provide busy practitioners with concise, peer-reviewed recommendations in Hypoalbuminemic Dogs on current treatment standards drawn from published veterinary medical literature. Michelle Savigny, DVM Resident, Emergency and Critical Care Douglass K. Macintire, DVM, MS, DACVIM, DACVECC This publication acknowledges that Professor standards may vary according to individual Department of Clinical Sciences experience and practices or regional College of Veterinary Medicine differences. The publisher is not responsible Auburn University for author errors. lbumin is a crucial protein in the body, comprising approximately half of the Reviewed 2015 for significant advances plasma total protein. Albumin is synthesized exclusively by the liver. Under in medicine since the date of original normal conditions, production occurs at one-third maximum capacity, meaning A publication. No revisions have been that in times of need, the liver has reserve capacity to increase albumin production. Stimulus for production is mainly the colloid osmotic pressure (COP) of the blood, made to the original text. but other factors, such as nutritional state, intracellular potassium, and certain hormones, also play a role. Synthetic substances such as hetastarch and dextrans can also be recognized by the Editor-in-Chief hepatic osmoreceptors and affect albumin synthesis. If these synthetic substances are Douglass K. Macintire, DVM, MS, used to increase COP to or above a normal level (20–40 mm Hg), they can actually DACVIM, DACVECC turn off the signal to the liver to produce more albumin. Degradation occurs at a rate directly related to concentration, with decreased degradation in times of hypo - Editorial Review Board albuminemia.