Benzodiazepine Dependence Studies in Animals: an Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
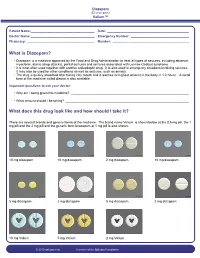
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -
Drug & Alcohol Testing Program
Pottawattmie County Drug & Alcohol Testing Program Appendix A Table of Contents POLICY STATEMENT ...................................................................................................................................... 3 SCOPE ............................................................................................................................................................ 4 EDUCATION AND TRAINING .......................................................................................................................... 4 DESIGNATED EMPLOYER REPRESENTATIVE (DER): ....................................................................................... 5 DUTY TO COOPERATE ................................................................................................................................... 5 EMPLOYEE ADMISSION OF ALCOHOL AND CONTROLLED SUBSTANCE USE: (49 CFR Part 382.121) ... 6 PROHIBITED DRUGS AND ILLEGALLY USED CONTROLLED SUBSTANCES: ..................................................... 7 PROHIBITED BEHAVIOR AND CONDUCT: ...................................................................................................... 8 DRUG & ALCOHOL TESTING REQUIREMENTS (49 CFR, Part 40 & 382) ............................................... 10 DRUG & ALCOHOL TESTING CIRCUMSTANCES (49 CFR Part 40 & 382) .............................................. 12 A. Pre-Employment Testing: .................................................................................................... 12 B. Reasonable Suspicion Testing: ......................................................................................... -

Journal of Pharmacology and Experimental Therapeutics
Journal of Pharmacology and Experimental Therapeutics Molecular Determinants of Ligand Selectivity for the Human Multidrug And Toxin Extrusion Proteins, MATE1 and MATE-2K Bethzaida Astorga, Sean Ekins, Mark Morales and Stephen H Wright Department of Physiology, University of Arizona, Tucson, AZ 85724, USA (B.A., M.M., and S.H.W.) Collaborations in Chemistry, 5616 Hilltop Needmore Road, Fuquay-Varina NC 27526, USA (S.E.) Supplemental Table 1. Compounds selected by the common features pharmacophore after searching a database of 2690 FDA approved compounds (www.collaborativedrug.com). FitValue Common Name Indication 3.93897 PYRIMETHAMINE Antimalarial 3.3167 naloxone Antidote Naloxone Hydrochloride 3.27622 DEXMEDETOMIDINE Anxiolytic 3.2407 Chlordantoin Antifungal 3.1776 NALORPHINE Antidote Nalorphine Hydrochloride 3.15108 Perfosfamide Antineoplastic 3.11759 Cinchonidine Sulfate Antimalarial Cinchonidine 3.10352 Cinchonine Sulfate Antimalarial Cinchonine 3.07469 METHOHEXITAL Anesthetic 3.06799 PROGUANIL Antimalarial PROGUANIL HYDROCHLORIDE 100MG 3.05018 TOPIRAMATE Anticonvulsant 3.04366 MIDODRINE Antihypotensive Midodrine Hydrochloride 2.98558 Chlorbetamide Antiamebic 2.98463 TRIMETHOPRIM Antibiotic Antibacterial 2.98457 ZILEUTON Antiinflammatory 2.94205 AMINOMETRADINE Diuretic 2.89284 SCOPOLAMINE Antispasmodic ScopolamineHydrobromide 2.88791 ARTICAINE Anesthetic 2.84534 RITODRINE Tocolytic 2.82357 MITOBRONITOL Antineoplastic Mitolactol 2.81033 LORAZEPAM Anxiolytic 2.74943 ETHOHEXADIOL Insecticide 2.64902 METHOXAMINE Antihypotensive Methoxamine -

(12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn Et Al
US 2004O224012A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn et al. (43) Pub. Date: Nov. 11, 2004 (54) TOPICAL APPLICATION AND METHODS Related U.S. Application Data FOR ADMINISTRATION OF ACTIVE AGENTS USING LIPOSOME MACRO-BEADS (63) Continuation-in-part of application No. 10/264,205, filed on Oct. 3, 2002. (76) Inventors: Pichit Suvanprakorn, Bangkok (TH); (60) Provisional application No. 60/327,643, filed on Oct. Tanusin Ploysangam, Bangkok (TH); 5, 2001. Lerson Tanasugarn, Bangkok (TH); Suwalee Chandrkrachang, Bangkok Publication Classification (TH); Nardo Zaias, Miami Beach, FL (US) (51) Int. CI.7. A61K 9/127; A61K 9/14 (52) U.S. Cl. ............................................ 424/450; 424/489 Correspondence Address: (57) ABSTRACT Eric G. Masamori 6520 Ridgewood Drive A topical application and methods for administration of Castro Valley, CA 94.552 (US) active agents encapsulated within non-permeable macro beads to enable a wider range of delivery vehicles, to provide longer product shelf-life, to allow multiple active (21) Appl. No.: 10/864,149 agents within the composition, to allow the controlled use of the active agents, to provide protected and designable release features and to provide visual inspection for damage (22) Filed: Jun. 9, 2004 and inconsistency. US 2004/0224012 A1 Nov. 11, 2004 TOPCAL APPLICATION AND METHODS FOR 0006 Various limitations on the shelf-life and use of ADMINISTRATION OF ACTIVE AGENTS USING liposome compounds exist due to the relatively fragile LPOSOME MACRO-BEADS nature of liposomes. Major problems encountered during liposome drug Storage in vesicular Suspension are the chemi CROSS REFERENCE TO OTHER cal alterations of the lipoSome compounds, Such as phos APPLICATIONS pholipids, cholesterols, ceramides, leading to potentially toxic degradation of the products, leakage of the drug from 0001) This application claims the benefit of U.S. -
Definition of Controlled Substance Schedules
UPDATED MARCH 2018 DEFINITION OF CONTROLLED SUBSTANCE SCHEDULES Drugs and other substances that are considered controlled substances under the Controlled Substances Act (CSA) are divided into five schedules. An updated and complete list of the schedules is published annually in Title 21 Code of Federal Regulations (C.F.R.) §§ 1308.11 through 1308.15. Substances are placed in their respective schedules based on whether they have a currently accepted medical use in treatment in the U.S., their relative abuse potential, and likelihood of causing dependence when abused. Examples of the drugs in each schedule are listed below. Schedule I Controlled Substances Substances in this schedule have no currently accepted medical use in the United States, a lack of accepted safety for use under medical supervision, and a high potential for abuse. Some examples of substances listed in Schedule I are: heroin, lysergic acid diethylamide (LSD), marijuana (cannabis), peyote, methaqualone, and 3,4- methylenedioxymethamphetamine ("Ecstasy"). Schedule II/IIN Controlled Substances (2/2N) Substances in this schedule have a high potential for abuse which may lead to severe psychological or physical dependence. Examples of Schedule II narcotics include: hydromorphone (Dilaudid®), methadone (Dolophine®), meperidine (Demerol®), oxycodone (OxyContin®, Percocet®), and fentanyl (Sublimaze®, Duragesic®). Other Schedule II narcotics include: morphine, opium, codeine, and hydrocodone. Examples of Schedule IIN stimulants include: amphetamine (Dexedrine®, Adderall®), methamphetamine (Desoxyn®), and methylphenidate (Ritalin®). Other Schedule II substances include: amobarbital, glutethimide, and pentobarbital. 1 Schedule III/IIIN Controlled Substances (3/3N) Substances in this schedule have a potential for abuse less than substances in Schedules I or II and abuse may lead to moderate or low physical dependence or high psychological dependence. -

Pentameric Ligand-Gated Ion Channel ELIC Is Activated by GABA And
Pentameric ligand-gated ion channel ELIC is activated PNAS PLUS by GABA and modulated by benzodiazepines Radovan Spurnya, Joachim Ramerstorferb, Kerry Pricec, Marijke Bramsa, Margot Ernstb, Hugues Nuryd, Mark Verheije, Pierre Legrandf, Daniel Bertrandg, Sonia Bertrandg, Dennis A. Doughertyh, Iwan J. P. de Esche, Pierre-Jean Corringerd, Werner Sieghartb, Sarah C. R. Lummisc, and Chris Ulensa,1 aDepartment of Cellular and Molecular Medicine, Laboratory of Structural Neurobiology, Catholic University of Leuven, 3000 Leuven, Belgium; bDepartment of Biochemistry and Molecular Biology of the Nervous System, Medical University of Vienna, A-1090 Vienna, Austria; cDepartment of Biochemistry, University of Cambridge, Cambridge CB2 1QW, United Kingdom; dPasteur Institute, G5 Group of Channel-Receptor, Centre National de la Recherche Scientifique, 75724 Paris, France; eDepartment of Medicinal Chemistry, VU University Amsterdam, 1081 HV, Amsterdam, The Netherlands; fSOLEIL Synchrotron, 91192 Gif sur Yvette, France; gHiQScreen, CH-1211 Geneva, Switzerland; and hCalifornia Institute of Technology, Pasadena, CA 91125 Edited* by Jean-Pierre Changeux, Institut Pasteur, Paris Cedex 15, France, and approved September 10, 2012 (received for review May 24, 2012) GABAA receptors are pentameric ligand-gated ion channels in- marized in SI Appendix, Table S1). In addition, it has been volved in fast inhibitory neurotransmission and are allosterically suggested that the GABA carboxylate group is stabilized through modulated by the anxiolytic, anticonvulsant, and sedative-hypnotic electrostatic interactions with Arg residues on the principal and benzodiazepines. Here we show that the prokaryotic homolog ELIC complementary faces of the binding site (4, 7–9). For benzo- also is activated by GABA and is modulated by benzodiazepines diazepines, the individual contributions of residues in loops A–F with effects comparable to those at GABAA receptors. -

WO 2015/072852 Al 21 May 2015 (21.05.2015) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2015/072852 Al 21 May 2015 (21.05.2015) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 36/84 (2006.01) A61K 31/5513 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/045 (2006.01) A61P 31/22 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/522 (2006.01) A61K 45/06 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, PCT/NL20 14/050780 KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (22) International Filing Date: MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, 13 November 2014 (13.1 1.2014) PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (25) Filing Language: English TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/903,430 13 November 2013 (13. 11.2013) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, (71) Applicant: RJG DEVELOPMENTS B.V. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Pharmacological Treatments in Insomnia
Pharmacological treatments in insomnia Sue Wilson Centre for Neuropsychopharmacology, Division of Brain Sciences, Imperial College, London Drugs used in insomnia Licensed for insomnia •GABA-A positive allosteric modulators •melatonin (modified release) •promethazine •diphenhydramine •doxepin (USA) Unlicensed prescribed frequently •antihistamines (and OTC) •antidepressants Sometimes prescribed drugs for psychosis Some GABA-A positive allosteric modulators Drugs acting at the GABA-A benzodiazepine receptor zopiclone zolpidem zaleplon benzodiazepines eg temazepam, lorazepam (safe in overdose, as long as no other drug involved) Drugs acting at the barbiturate/alcohol receptor chloral hydrate/chloral betaine clomethiazole (dangerous in overdose) GABA calms the brain Gamma aminobutyic acid (GABA) is the main inhibitory transmitter in the mammalian central nervous system. It plays the principal role in reducing neuronal excitability and its receptors are prolific throughout the brain, in cortex, limbic system, thalamus and cerebellum sedative Increase anticonvulsant GABA anxiolytic function ataxia, memory effects Effects of GABA-A positive allosteric modulators •These drugs enhance the effect of GABA, the main inhibitory neurotransmitter in the brain •They all produce sedation, sleep promotion, ataxia, muscle relaxation, effects on memory, anticonvulsant effects •Therefore for insomnia the duration of action of the drug is important – these effects are unwanted during the day Effects of these GABA-ergic drugs on sleep EEG/PSG • Appearance of -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drug-Facilitated Sexual Assault Panel, Blood
DRUG-FACILITATED SEXUAL ASSAULT PANEL, BLOOD Blood Specimens (Order Code 70500) Alcohols Analgesics, cont. Anticonvulsants, cont. Antihistamines, cont. Ethanol Phenylbutazone Phenytoin Cyclizine Amphetamines Piroxicam Pregabalin Diphenhydramine Amphetamine Salicylic Acid* Primidone Doxylamine BDB Sulindac* Topiramate Fexofenadine Benzphetamine Tapentadol Zonisamide Guaifenesin Ephedrine Tizanidine Antidepressants Hydroxyzine MDA Tolmetin Amitriptyline Loratadine MDMA Tramadol Amoxapine Oxymetazoline* Mescaline* Anesthetics Bupropion Pyrilamine Methcathinone Benzocaine Citalopram Tetrahydrozoline Methamphetamine Bupivacaine Clomipramine Triprolidine Phentermine Etomidate Desipramine Antipsychotics PMA Ketamine Desmethylclomipramine 9-hydroxyrisperidone Phenylpropanolamine Lidocaine Dosulepin Aripiprazole Pseudoephedrine Mepivacaine Doxepin Buspirone Analgesics Methoxetamine Duloxetine Chlorpromazine Acetaminophen Midazolam Fluoxetine Clozapine Baclofen Norketamine Fluvoxamine Fluphenazine Buprenorphine Pramoxine* Imipramine Haloperidol Carisoprodol Procaine 1,3-chlorophenylpiperazine (mCPP) Mesoridazine Cyclobenzaprine Rocuronium Mianserin* Norclozapine Diclofenac Ropivacaine Mirtazapine Olanzapine Etodolac Antibiotics Nefazodone Perphenazine Fenoprofen Azithromycin* Nordoxepin Pimozide Hydroxychloroquine Chloramphenicol* Norfluoxetine Prochlorperazine Ibuprofen Ciprofloxacin* Norsertraline Quetiapine Ketoprofen Clindamycin* Nortriptyline Risperidone Ketorolac Erythromycin* Norvenlafaxine Thioridazine Meclofenamic Acid* Levofloxacin* Paroxetine