Epsom and St Helier University Hospitals NHS Trust: Annual Report and Accounts 2019/20
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Senior Living Urban (Epsom) Ltd Guild Living Care Community Epsom Hospital Woodcote Green Road
SENIOR LIVING URBAN (EPSOM) LTD GUILD LIVING CARE COMMUNITY EPSOM HOSPITAL WOODCOTE GREEN ROAD TRANSPORT ASSESSMENT DECEMBER 2019 SENIOR LIVING URBAN (EPSOM) LTD GUILD LIVING CARE COMMUNITY EPSOM HOSPITAL WOODCOTE GREEN ROAD TRANSPORT ASSESSMENT DECEMBER 2019 Project Code: B/GLEpsom.1 Prepared by: RG Approved by: RG Issue Date: December 2019 Status: Final Mayer Brown Limited, Lion House, Oriental Road, Woking, Surrey GU22 8AR Telephone 01483 750508 Fax 01483 750437 [email protected] www.mayerbrown.co.uk Senior Living Urban (Epsom) Ltd Guild Living Care Community Epsom Hospital Woodcote Green Road Transport Assessment List of Contents Sections 1 Introduction ......................................................................................................... 1 2 Existing Site Context & Accessibility ................................................................... 2 3 Development Proposals .................................................................................... 15 4 Planning Policy Background ............................................................................. 20 5 Traffic Flows & Trip Generation ........................................................................ 28 6 Traffic Impact .................................................................................................... 35 7 Parking Assessment ......................................................................................... 40 8 Accident Analysis ............................................................................................. -
Annual Report and Accounts
Epsom and St Helier University Hospitals NHS Trust Annual Report and Accounts 1st April 2019 to 31st March 2020 Epsom and St Helier University Hospitals NHS Trist Annual Report and Accounts 1st April 2019 to 31st March 2020 Presented to Parliament pursuant to Schedule 7, paragraph 25(4)(a) of the National Health Service Act 2006 Contents 1. Performance Report • Welcome – a message from our Chairman and Chief Executive 5-12 • About Epsom and St Helier University Hospitals NHS Trust 13-15 • Our vision, values and objectives 15-19 • Performance overview 20-24 2. Accountability Report • Annual Governance Statement 26-50 • Statement of Accountable Officers’ Responsibilities 51-52 • Directors’ Report 53-54 3. Annual Report and Accounts 55 Please note, most of the photographs in this report were taken before the rules around social distancing came into force 1.Performance Report -4- • Welcome – a Message from our Chairman and Chief Executive Gillian Norton Daniel Elkeles Chairman Chief Executive Officer We are delighted to present our Annual Report and Accounts for Epsom and St Helier University Hospitals NHS Trust for 2019/20. We must introduce this report by acknowledging the significant impact of COVID-19 at the end of the year under review. Although the majority of our Annual Report focusses on pre-COVID-19 matters, the onset of the pandemic had a major impact on our operations from March onwards. We have been deeply moved by our staff’s response to the COVID-19 pandemic – we have been overawed by the depths of their courage and commitment and would like to pass on a huge THANK YOU – and not only from us. -

Epsom Heritage
EPSOM HERITAGE A Detailed Survey of Epsom with historical context by Thomas H.J. Dethridge HISTORICAL BACKGROUND HIGH STREET (WEST) WEST STREET AND WEST HILL SOUTH STREET AND WOODCOTE HIGH STREET (EAST) UPPER HIGH STREET THE RAILWAY COMES TO EPSOM CHURCH STREET HISTORICAL BACKGROUND Epsom was founded in or about the 6th century (one historian suggests the fifth) as a Saxon settlement close to the Roman road of Stane Street, along which the new arrivals probably travelled. The road ran between Londinium (London) and Noviomagus (Chichester) and the new hamlet was named from the leader called Ebb (or Ebba or Ebbi) - hence Ebb’s hame. Over the centuries there have been a dozen or more renderings until Epsom became the more or less accepted version by the 16th century. The name Ebbisham is of course still to be found locally. The village is mentioned in the Doomsday Book as Evesham with the Abbot of Chertsey as its landlord, a state of affairs that remained the case up to the dissolution of the monasteries under Henry VIII. There were at one time quite separate communities of Woodcote and in the Stamford Green area, but these are now part of Epsom. That Stane Street continued in existence as a major way for some centuries is borne out by the fact that William the Conqueror after the battle of Hastings rode along part of the Surrey section on his advance towards London. There does not appear to be much in the way of definitive archaeological evidence as to the precise routing of Stane Street, at any rate at its northern end, perhaps evidence exists still waiting to be uncovered. -
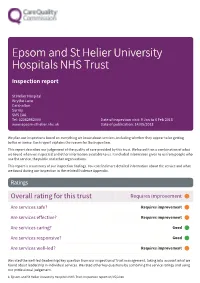
RVR Epsom and St Helier University Hospitals NHS Trust
Epsom and St Helier University Hospitals NHS Trust Inspection report St Helier Hospital Wrythe Lane Carshalton Surrey SM5 1AA Tel: 02082962000 Date of inspection visit: 9 Jan to 6 Feb 2018 www.epsom-sthelier.nhs.uk Date of publication: 14/05/2018 We plan our inspections based on everything we know about services, including whether they appear to be getting better or worse. Each report explains the reason for the inspection. This report describes our judgement of the quality of care provided by this trust. We based it on a combination of what we found when we inspected and other information available to us. It included information given to us from people who use the service, the public and other organisations. This report is a summary of our inspection findings. You can find more detailed information about the service and what we found during our inspection in the related Evidence Appendix. Ratings Overall rating for this trust Requires improvement ––– Are services safe? Requires improvement ––– Are services effective? Requires improvement ––– Are services caring? Good ––– Are services responsive? Good ––– Are services well-led? Requires improvement ––– We rated the well-led (leadership) key question from our inspection of trust management, taking into account what we found about leadership in individual services. We rated other key questions by combining the service ratings and using our professional judgement. 1 Epsom and St Helier University Hospitals NHS Trust Inspection report 14/05/2018 Summary of findings Background to the trust Epsom and St Helier University Hospitals NHS Trust has approximately 870 beds located across two acute locations; Epsom General Hospital which is located in Epsom and St Helier Hospital and Queen Mary’s Hospital for Children which is located in Sutton. -

8961 Medical Multiple
Schedule of Accreditation issued by United Kingdom Accreditation Service 2 Pine Trees, Chertsey Lane, Staines-upon-Thames, TW18 3HR, UK St George’s University Hospitals NHS Foundation Trust Issue No: 005 Issue date: 01 May 2021 SWLP Department of Blood Sciences Contact: Asam Saeed Epsom and St Helier University Hospitals Tel: +44 (0)208296553 St Helier Hospital E-Mail:[email protected] 8961 Wrythe Lane Surrey Accredited to ISO 15189:2012 SM5 1AA Testing performed by the Organisation at the locations specified below Locations covered by the organisation and their relevant activities Laboratory locations: Location details Activity Location code Address Local contact • Routine Haematology Department of Blood sciences Asam Saeed • Blood fridges A St Helier Hospital • Biochemistry Wrythe Lane • Special chemistry Carshalton • Neonatal screening SM5 1AA Department of Blood Sciences Asam Saeed • Routine Haematology Epsom General Hospital • Blood Transfusion B Dorking Road • Blood fridges Epsom • Biochemistry KT18 7EG Blood fridge locations aware from the laboratory: Location details Activity Location code Elective Orthopaedic centre • Blood Fridge C Epsom Hospital Ashtead Hospital, The Warren, Ashtead, • Blood fridge E KT21 2SB Assessment Manager: EWS Page 1 of 13 Schedule of Accreditation issued by United Kingdom Accreditation Service 2 Pine Trees, Chertsey Lane, Staines -u po n - Thames, TW18 3HR, UK St George’s University Hospitals NHS Foundation Trust 8961 Accredited to Issue No: 005 Issue date: 01 May 2021 ISO 15189:2012 Testing performed -

Where to Get Your Blood Test
WHERE TO GET YOUR BLOOD TEST Blood tests can be done at any one of a number of local health centres across Sutton and Merton Monday to Friday. We provide a booked phlebotomy (blood test) service at all locations. You must have a booked appointment to attend this service. MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY St Helier Hospital Ferguson House St Helier Hospital Ferguson House St Helier Hospital Ferguson House St Helier Hospital Ferguson House St Helier Hospital Ferguson House Wrythe Lane Carshalton SM5 1AA Wrythe Lane Carshalton SM5 1AA Wrythe Lane Carshalton SM5 1AA Wrythe Lane Carshalton SM5 1AA Wrythe Lane Carshalton SM5 1AA 07.30 – 4.30 07.30 – 4.30 07.30 – 4.30 07.30 – 4.30 07.30 – 4.30 Epsom Hospital Headley Wing Epsom Hospital Headley Wing Epsom Hospital Headley Wing Epsom Hospital Headley Wing Epsom Hospital Headley Wing Ground floor block A Headley Wing Ground floor block A Headley Wing Ground floor block A Headley Wing Ground floor block A Headley Wing Ground floor block A Headley Wing Dorking Road Epsom KT18 7EG Dorking Road Epsom KT18 7EG Dorking Road Epsom KT18 7EG Dorking Road Epsom KT18 7EG Dorking Road Epsom KT18 7EG 08.30 – 4.30 08.30 – 4.30 08.30 – 4.30 08.30 – 4.30 08.30 – 4.30 Sutton Hospital Malvern Centre Sutton Hospital Malvern Centre Sutton Hospital Malvern Centre Sutton Hospital Malvern Centre Sutton Hospital Malvern Centre Sutton Hospital Sutton Hospital Sutton Hospital Sutton Hospital Sutton Hospital Cotswold Road Sutton SM2 5NF Cotswold Road Sutton SM2 5NF Cotswold Road Sutton SM2 5NF Cotswold Road Sutton -

Introduction in 2002, a Book Was Published Depicting the History of Epsom Coaches. Written by Roy and Andrew Richmond, It Celebr
Introduction In 2002, a book was published depicting the history of Epsom Coaches. Written by Roy and Andrew Richmond, it celebrated the long life of the business and its development over then, 82 years. The book was amply illustrated with historic and modern photographs, of people, occasions and the fleet across the years. Long out of print, the full text and some of the photographs are reproduced here for the first time online. A new history bringing the story up to date, will be published on the centenary of the company’s founding in 2020 and will be previewed on this website. Andrew & Roy Richmond Pictured in 2002 Chapter 1 THE FORMATIVE YEARS Herbert Roderick Richmond, better known as Roddy, was born on 31st August 1891, and was the youngest son of Frederick and Clara Richmond. Frederick Richmond was a farmer in the village of Reepham in Norfolk. Roddy’s brother was a qualified doctor, and his sister was an accomplished pianist who had regular engagements throughout Austria and Germany. Roddy went to Chapmans Academy, a boarding school in Norwich, where he went through the indignity of being a “fag”, attending to the needs of a house prefect. On market days, his father would go to Norwich to buy and sell sheep, and this gave them an opportunity to meet up occasionally during term time. His father was used to dealing in cash for these transactions, a habit that Roddy and to some extent, Roy followed in later years. The practice ceased when Roy took his trousers for dry cleaning one day without checking his pockets! During the school holidays Roddy used to repair the farm machinery out in the fields. -

479 Guildford
Guildford - Little Bookham - Leatherhead - Epsom 479 Arriva Kent & Surrey Timetable effective 01 September 2019 Monday to Friday (except Public Holidays) SD SH SD SH Guildford, Friary Bus Station 0610... ...0750... 58 ... 1258 ...141514201515... Merrow, Church 0619... ...0805... 09 ... 1309 ...142614311527... West Clandon, Crossroads 0622... ...0808... 12 ... 1312 ...142914341530... East Horsley, Duke of Wellington 0627... ...0814... 17 ... 1317 ...143414391536... Howard of Effingham School 0633071407350823... 23 ... 1323 ...1440144515441610 Preston Cross 0636071607380826... and 26 ... 1326 ...1445145015471613 Bookham, Railway Station 06390721074308290859then 29 59 132914091448145315501616 Great Bookham, Old Crown 06430725074708340904 at 34 04 133414141453145815541620 Fetcham,Orchard Close 06490736075808410911these41 11 until134114211500150516011627 Leatherhead, North Street Lidl 06540744080608470917mins47 17 134714271506151116081633 Leatherhead, Railway Station 06580749081108510921past51 21 135114311511151616121638 Leatherhead, All Saints School \ 0753 \ \ \ each \ \ \ \ \ \ \ \ Ashtead, Pond \ 08000819 \ 0929hour \ 29 \ 1439 \ \ \ 1646 Leatherhead, St. Andrews School \ 0815 \ \ \ \ \ \ \ 1520 \ \ \ Ashtead, Pond 0705 \ \ 0859 \ 59 \ 1359 \ \ 15251621 \ Ashtead, The Street 07100824082409030933 03 33 140314431530153016251650 Epsom Hospital, Dorking Road 07140828082809070937 07 37 140714471535153516291654 Epsom, Clock Tower 07170834083409100940 10 40 141014501539153916331658 Monday to Friday (continued) Saturday Guildford, Friary Bus Station -

Epsom General Hospital Quality Report
Epsom and St Helier University Hospitals NHS Trust Epsom General Hospital Quality Report Epsom General Hospital Dorking Road Epsom Date of inspection visit: Announced visit 10 and 13 Surrey November 2015. We also undertook unannounced KT18 7EG visits to the hospital on 21, 23 and 27 November Tel: 01372 735735 2015. Website: : www.epsom-sthelier.nhs.uk Date of publication: 27/05/2016 This report describes our judgement of the quality of care at this hospital. It is based on a combination of what we found when we inspected, information from our ‘Intelligent Monitoring’ system, and information given to us from patients, the public and other organisations. Ratings Overall rating for this hospital Requires improvement ––– Urgent and emergency services Requires improvement ––– Medical care (including older people’s care) Good ––– Surgery Requires improvement ––– Critical care Requires improvement ––– Maternity and gynaecology Requires improvement ––– Services for children and young people Requires improvement ––– End of life care Good ––– Outpatients and diagnostic imaging Good ––– Elective orthopaedic centre Outstanding – 1 Epsom General Hospital Quality Report 27/05/2016 Summary of findings Letter from the Chief Inspector of Hospitals Epsom General Hospital is part of Epsom and St Helier University Hospitals NHS Trust. The trust provides local acute services for people living in the southwest London and northeast Surrey. Epsom General Hospital provides acute hospital services to population of around 180,000. Epsom General Hospital is home to the South West Elective Orthopaedic Centre (SWLEOC), which is one of the largest hip and knee joint replacement centers in the UK. Most of the trust’s elective surgery is undertaken at Epsom General Hospital and the majority of emergency surgery is carried at the trust’s other location, St Helier Hospital and Queen Mary's Hospital for Children. -

Epsom and St Helier University Hospitals NHS Trust: Annual Report
Annual Report 2017 - 2018 If you or someone you know cannot read this document, please contact us and we will do our best to provide the information in a suitable format or language. For more information, contact the Communications Team on 020 8296 4995 or email [email protected]. St Helier Hospital Epsom Hospital Wrythe Lane Dorking Road Carshalton Epsom Surrey Surrey SM5 1AA KT18 7EG Tel: 020 8296 2000 Tel: 01372 735735 These are the main hospitals that we run our services from. However, our doctors, nurses and other staff also work from a number of other sites, as well as nine renal centres for patients needing dialysis. www.epsom-sthelier.nhs.uk twitter.com/epsom_sthelier facebook.com/epsomsthelier Contents PERFORMANCE REPORT 1 Overview: 4 A welcome from our Chairman and Chief Executive 5 About us 8 Our values, objectives and five year strategy 9 2 Performance analysis 16 Deliver safe and effective care with dignity and respect 17 Create a positive experience that meets the expectations of our 22 patients, their families and carers Provide responsive care that delivers the right treatment, in the right 29 place at the right time Maintain financial sustainability 31 Work in partnership with our patients, commissioners, other health 32 providers and local authorities Ensuring we have highly engaged, patient centred and skilled teams 34 that are well-led. ACCOUNTABILITY REPORT 35 3 Corporate Governance Report 36 Governance statement 36 Executive and non-executive directors and the role of the trust board 37 Statement of Accountable Officer’s responsibilities 47 Director’s report 48 Remuneration and staff report 53 The accounts 60 1 Overview PERFORMANCE REPORT - overview Welcome to the 2017-18 Annual Report – a message from our Chairman and Chief Executive As another year comes to a close, we are delighted to be able to share an overview of how the Trust performed during 2017-18. -

Epsom and St Helier University Hospitals NHS Trust
Epsom and St Helier University Hospitals NHS Trust Quality Report Wrythe Lane Carshalton SM5 1AA Date of inspection visit: 10, 11, 12, 13, 21, 23 and 27 Tel: 020 8296 2000 November 2015 Website: www.epsom-sthelier.nhs.uk Date of publication: 27/05/2016 This report describes our judgement of the quality of care at this trust. It is based on a combination of what we found when we inspected, information from our ‘Intelligent Monitoring’ system, and information given to us from patients, the public and other organisations. Ratings Overall rating for this trust Requires improvement ––– Are services at this trust safe? Requires improvement ––– Are services at this trust effective? Requires improvement ––– Are services at this trust caring? Requires improvement ––– Are services at this trust responsive? Requires improvement ––– Are services at this trust well-led? Requires improvement ––– 1 Epsom and St Helier University Hospitals NHS Trust Quality Report 27/05/2016 Summary of findings Letter from the Chief Inspector of Hospitals We carried out a comprehensive inspection of Epsom and We have rated Epsom and St Helier University Hospitals St Helier University Hospitals NHS Trust (the trust) as part NHS Trust overall as ‘requires improvement’. The key of our routine inspection programme. Epsom and St questions of safe, effective, caring, responsive and well- Helier University Hospitals NHS University Hospitals NHS led were all rated as 'requires improvement'. Both Epsom Trust had been identified as having only two elevated and General Hospital and St Helier Hospital were rated as one risk on the Care Quality Commission’s (CQC) ‘requires improvement’. -

Epsom Hospital Site, Dorking Road, Epsom, KT18 7EG Planning Statement
Epsom Hospital Site, Dorking Road, Epsom, KT18 7EG Planning Statement On behalf of Senior Living Urban (Epsom) Limited February 2021 Epsom Hospital Site, Dorking Road, Epsom, KT18 7EG Planning Statement Contents 1 Introduction .............................................................................................................................................. 2 2 The Applicant ............................................................................................................................................ 9 3 The Guild Living Care Community Concept ........................................................................................ 30 4 Site and Surroundings ........................................................................................................................... 11 5 Planning Policy ....................................................................................................................................... 15 6 The Development Proposal ................................................................................................................... 30 7 Planning Considerations ........................................................................................................................ 42 8 Conclusions ............................................................................................................................................. 79 Appendix 1: Site History Appendix 2: NHS Land Sale Press Release Senior Living Urban (Epsom) Limited 1 Epsom Hospital Site, Dorking