Amiodarone Hydrochloride)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Pharmacology of Amiodarone and Digoxin As Antiarrhythmic Agents
Part I Anaesthesia Refresher Course – 2017 University of Cape Town The Pharmacology of Amiodarone and Digoxin as Antiarrhythmic Agents Dr Adri Vorster UCT Department of Anaesthesia & Perioperative Medicine The heart contains pacemaker, conduction and contractile tissue. Cardiac arrhythmias are caused by either enhancement or depression of cardiac action potential generation by pacemaker cells, or by abnormal conduction of the action potential. The pharmacological treatment of arrhythmias aims to achieve restoration of a normal rhythm and rate. The resting membrane potential of myocytes is around -90 mV, with the inside of the membrane more negative than the outside. The main extracellular ions are Na+ and Cl−, with K+ the main intracellular ion. The cardiac action potential involves a change in voltage across the cell membrane of myocytes, caused by movement of charged ions across the membrane. This voltage change is triggered by pacemaker cells. The action potential is divided into 5 phases (figure 1). Phase 0: Rapid depolarisation Duration < 2ms Threshold potential must be reached (-70 mV) for propagation to occur Rapid positive charge achieved as a result of increased Na+ conductance through voltage-gated Na+ channels in the cell membrane Phase 1: Partial repolarisation Closure of Na+ channels K+ channels open and close, resulting in brief outflow of K+ and a more negative membrane potential Phase 2: Plateau Duration up to 150 ms Absolute refractory period – prevents further depolarisation and myocardial tetany Result of Ca++ influx -

Tricyclic Antidepressant
Princess Margaret Hospital for Children Emergency Department Guideline PAEDIATRIC ACUTE CARE GUIDELINE Poisoning – Tricyclic Antidepressant Scope (Staff): All Emergency Department Clinicians Scope (Area): Emergency Department This document should be read in conjunction with this DISCLAIMER http://kidshealthwa.com/about/disclaimer/ Poisoning – Tricyclic Antidepressant This guideline is a general approach to tricyclic antidepressant poisoning. For specific details please contact Poisons Information: 131126 or refer to the Toxicology Handbook. Agents: Amitriptyline Clomipramine Dothiepin Doxepin Imipramine Nortriptyline Trimipramine Background Tricyclic antidepressants (TCAs) act on a variety of receptors whose actions include: Noradrenaline reuptake inhibition Central and peripheral anticholinergic effect Fast sodium channel blockade in the myocardium Peripheral alpha1-adrenergic receptor blockade The life threatening effects of acute tricyclic antidepressant (TCA) overdose are: Rapid onset of coma Seizures Cardiac dysrhythmias Page 1 of 6 Emergency Department Guideline Poisoning – Tricyclic Antidepressant Hypotension and central and peripheral anticholinergic effects may also be seen Risk Assessment Most acute accidental paediatric exposures do not result in life threatening toxicity A 10kg child can develop life threatening poisoning with the ingestion of a single tablet (e.g. 150mg amitriptyline) Patients who ingest a large dose of TCA usually develop evidence of intoxication within 2-4 hours, and always within 6 hours If their is suspicion -

Amiodarone (As Hydrochloride)
NEW ZEALAND DATA SHEET ARATAC 1. Product Name Aratac, 100 mg and 200 mg tablet. 2. Qualitative and Quantitative Composition Each Aratac tablet contains 100 mg or 200 mg of amiodarone (as hydrochloride). Aratac tablets contain lactose. For the full list of excipients, see section 6.1. Amiodarone hydrochloride is a fine white crystalline powder. It is slightly soluble in water and is soluble in alcohol and chloroform. It is an amphiphilic compound and contains iodine in its formulation. Each 200 mg tablet of amiodarone contains approximately 75 mg organic iodine. In the steady state, metabolism of 300 mg amiodarone yields 9 mg/day of iodine. 3. Pharmaceutical Form Amiodarone 100 mg Tablet: round, normal convex, white tablet, 8.5 mm diameter, imprinted “AM” | “100” on one side and “G” on the other. Amiodarone 200 mg Tablet: round, normal convex, white tablet, 10.0 mm diameter, imprinted “AM” | “200” on one side and “G” on the other. The tablet can be divided into equal doses. 4. Clinical Particulars 4.1 Therapeutic indications Treatment should be initiated only under hospital or specialist supervision. Tachyarrhythmias associated with Wolff-Parkinson-White Syndrome. Atrial flutter and fibrillation when other agents cannot be used. All types of tachyarrhythmias of paroxysmal nature including: supraventricular, nodal and ventricular tachycardias, ventricular fibrillation; when other agents cannot be used. Tablets are used for stabilisation and long term treatment. 4.2 Dose and method of administration Dose Due to poor absorption and wide inter-patient variability of absorption, the initial loading and subsequent maintenance dosage schedules of the medicine in clinical use has to be individually titrated. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

Amiodarone Enhances Anticonvulsive Effect of Oxcarbazepine and Pregabalin in the Mouse Maximal Electroshock Model
International Journal of Molecular Sciences Article Amiodarone Enhances Anticonvulsive Effect of Oxcarbazepine and Pregabalin in the Mouse Maximal Electroshock Model Monika Banach 1 , Monika Rudkowska 1, Agata Sumara 2 and Kinga Borowicz-Reutt 1,* 1 Independent Unit of Experimental Neuropathophysiology, Medical University of Lublin, Jaczewskiego 8b, PL-20-090 Lublin, Poland; [email protected] (M.B.); [email protected] (M.R.) 2 Department of Pathophysiology, Medical University of Lublin, Jaczewskiego 8b, PL-20-090 Lublin, Poland; [email protected] * Correspondence: [email protected] Abstract: Accumulating experimental studies show that antiarrhythmic and antiepileptic drugs share some molecular mechanisms of action and can interact with each other. In this study, the influence of amiodarone (a class III antiarrhythmic drug) on the antiseizure action of four second-generation antiepileptic drugs was evaluated in the maximal electroshock model in mice. Amiodarone, although ineffective in the electroconvulsive threshold test, significantly potentiated the antielectroshock activ- ity of oxcarbazepine and pregabalin. Amiodarone, given alone or in combination with oxcarbazepine, lamotrigine, or topiramate, significantly disturbed long-term memory in the passive-avoidance task in mice. Brain concentrations of antiepileptic drugs were not affected by amiodarone. However, the brain concentration of amiodarone was significantly elevated by oxcarbazepine, topiramate, and pregabalin. Additionally, oxcarbazepine and pregabalin elevated the brain concentration of desethylamiodarone, the main metabolite of amiodarone. In conclusion, potentially beneficial action of amiodarone in epilepsy patients seems to be limited by neurotoxic effects of amiodarone. Although results of this study should still be confirmed in chronic protocols of treatment, special precautions Citation: Banach, M.; Rudkowska, are recommended in clinical conditions. -

Practical Guidelines for Clinicians Who Treat Patients with Amiodarone
SPECIAL ARTICLE Practical Guidelines for Clinicians Who Treat Patients With Amiodarone Nora Goldschlager, MD; Andrew E. Epstein, MD; Gerald Naccarelli, MD; Brian Olshansky, MD; Braman Singh, MD; for the Practice Guidelines Subcommittee, North American Society of Pacing and Electrophysiology miodarone has become an important drug for the treatment of supraventricular and ventricular arrhythmias, in short-term inpatient and outpatient settings. It may also have a role in affecting outcome in patients at high risk for arrhythmic events and sudden death; its place among available therapies is being established in clinical trials. A Arch Intern Med. 2000;160:1741-1748 Patterns of use of amiodarone are not uni- fibrillation (VF) or ventricular tachycar- form, either in academic or in community dia (VT) with hemodynamic instability. settings; overuse and underuse are likely This indication includes the stipula- real phenomena, although data are sparse tion that the arrhythmias are not respon- and largely anecdotal. Guidelines for phy- sive to other available antiarrhythmic sicians who use amiodarone are unavail- agents or that the patients are intolerant able. Because of the potential for serious of them. toxicity with its use, knowledge of drug dos- It is the consensus of this committee ing, beneficial effects, and adverse effects that amiodarone should be used as the an- is essential for proper patient manage- tiarrhythmic agent of choice, in connec- ment. This guideline was created as an ap- tion with other therapies (eg, b block- proach to the use of amiodarone in clini- ers), in patients with sustained ventricular cal practice. The guideline reviews the tachyarrhythmias who have structural indications for use of amiodarone and meth- heart disease, especially left ventricular ods of initiation of therapy, suggests strat- dysfunction, and who are not candidates egies for the follow-up of patients receiv- for an implantable cardioverter-defibrilla- ing amiodarone, and outlines the adverse tor (ICD). -

Cordarone (Amiodarone Hydrochloride)
Cordarone® (amiodarone HCl) TABLETS Rx only DESCRIPTION Cordarone (amiodarone HCl) is a member of a class of antiarrhythmic drugs with predominantly Class III (Vaughan Williams’ classification) effects, available for oral administration as pink, scored tablets containing 200 mg of amiodarone hydrochloride. The inactive ingredients present are colloidal silicon dioxide, lactose, magnesium stearate, povidone, starch, and FD&C Red 40. Cordarone is a benzofuran derivative: 2-butyl-3 benzofuranyl 4-[2-(diethylamino)-ethoxy]-3,5-diiodophenyl ketone hydrochloride. The structural formula is as follows: Amiodarone HCl is a white to cream-colored crystalline powder. It is slightly soluble in water, soluble in alcohol, and freely soluble in chloroform. It contains 37.3% iodine by weight. CLINICAL PHARMACOLOGY Electrophysiology/Mechanisms of Action In animals, Cordarone is effective in the prevention or suppression of experimentally induced arrhythmias. The antiarrhythmic effect of Cordarone may be due to at least two major properties: 1. a prolongation of the myocardial cell-action potential duration and refractory period and 2. noncompetitive α- and β-adrenergic inhibition. Cordarone prolongs the duration of the action potential of all cardiac fibers while causing minimal reduction of dV/dt (maximal upstroke velocity of the action potential). The refractory period is prolonged in all cardiac tissues. Cordarone increases the cardiac refractory period without influencing resting membrane potential, except in automatic cells where the slope of the prepotential is reduced, generally reducing automaticity. These electrophysiologic effects are reflected in a decreased sinus rate of 15 to 20%, increased PR and QT intervals of about 10%, the development of U-waves, and changes in T-wave contour. -

Drug–Drug Interactions Involving Intestinal and Hepatic CYP1A Enzymes
pharmaceutics Review Drug–Drug Interactions Involving Intestinal and Hepatic CYP1A Enzymes Florian Klomp 1, Christoph Wenzel 2 , Marek Drozdzik 3 and Stefan Oswald 1,* 1 Institute of Pharmacology and Toxicology, Rostock University Medical Center, 18057 Rostock, Germany; fl[email protected] 2 Department of Pharmacology, Center of Drug Absorption and Transport, University Medicine Greifswald, 17487 Greifswald, Germany; [email protected] 3 Department of Experimental and Clinical Pharmacology, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] * Correspondence: [email protected]; Tel.: +49-381-494-5894 Received: 9 November 2020; Accepted: 8 December 2020; Published: 11 December 2020 Abstract: Cytochrome P450 (CYP) 1A enzymes are considerably expressed in the human intestine and liver and involved in the biotransformation of about 10% of marketed drugs. Despite this doubtless clinical relevance, CYP1A1 and CYP1A2 are still somewhat underestimated in terms of unwanted side effects and drug–drug interactions of their respective substrates. In contrast to this, many frequently prescribed drugs that are subjected to extensive CYP1A-mediated metabolism show a narrow therapeutic index and serious adverse drug reactions. Consequently, those drugs are vulnerable to any kind of inhibition or induction in the expression and function of CYP1A. However, available in vitro data are not necessarily predictive for the occurrence of clinically relevant drug–drug interactions. Thus, this review aims to provide an up-to-date summary on the expression, regulation, function, and drug–drug interactions of CYP1A enzymes in humans. Keywords: cytochrome P450; CYP1A1; CYP1A2; drug–drug interaction; expression; metabolism; regulation 1. Introduction The oral bioavailability of many drugs is determined by first-pass metabolism taking place in human gut and liver. -
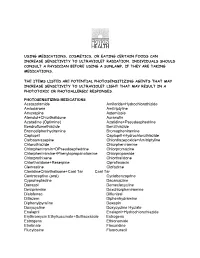
Using Medications, Cosmetics, Or Eating Certain Foods Can Increase Sensitivity to Ultraviolet Radiation
USING MEDICATIONS, COSMETICS, OR EATING CERTAIN FOODS CAN INCREASE SENSITIVITY TO ULTRAVIOLET RADIATION. INDIVIDUALS SHOULD CONSULT A PHYSICIAN BEFORE USING A SUNLAMP, IF THEY ARE TAKING MEDICATIONS. THE ITEMS LISTED ARE POTENTIAL PHOTOSENSITIZING AGENTS THAT MAY INCREASE SENSITIVITY TO ULTRAVIOLET LIGHT THAT MAY RESULT IN A PHOTOTOXIC OR PHOTOALLERGIC RESPONSES. PHOTOSENSITIZING MEDICATIONS Acetazolamide Amiloride+Hydrochlorothizide Amiodarone Amitriptyline Amoxapine Astemizole Atenolol+Chlorthalidone Auranofin Azatadine (Optimine) Azatidine+Pseudoephedrine Bendroflumethiazide Benzthiazide Bromodiphenhydramine Bromopheniramine Captopril Captopril+Hydrochlorothiazide Carbaamazepine Chlordiazepoxide+Amitriptyline Chlorothiazide Chlorpheniramine Chlorpheniramin+DPseudoephedrine Chlorpromazine Chlorpheniramine+Phenylopropanolamine Chlorpropamide Chlorprothixene Chlorthalidone Chlorthalidone+Reserpine Ciprofloxacin Clemastine Clofazime ClonidineChlorthalisone+Coal Tar Coal Tar Contraceptive (oral) Cyclobenzaprine Cyproheptadine Dacarcazine Danazol Demeclocycline Desipramine Dexchlorpheniramine Diclofenac Diflunisal Ditiazem Diphenhydramine Diphenylpyraline Doxepin Doxycycline Doxycycline Hyclate Enalapril Enalapril+Hydrochlorothiazide Erythromycin Ethylsuccinate+Sulfisoxazole Estrogens Estrogens Ethionamide Etretinate Floxuridine Flucytosine Fluorouracil Fluphenazine Flubiprofen Flutamide Gentamicin Glipizide Glyburide Gold Salts (compounds) Gold Sodium Thiomalate Griseofulvin Griseofulvin Ultramicrosize Griseofulvin+Hydrochlorothiazide Haloperidol -

Drug-Induced Parkinsonism
InformationInformation Sheet Sheet Drug-induced Parkinsonism Terms highlighted in bold italic are defined in increases with age, hypertension, diabetes, the glossary at the end of this information sheet. atrial fibrillation, smoking and high cholesterol), because of an increased risk of stroke and What is drug-induced parkinsonism? other cerebrovascular problems. It is unclear About 7% of people with parkinsonism whether there is an increased risk of stroke with have developed their symptoms following quetiapine and clozapine. See the Parkinson’s treatment with particular medications. This UK information sheet Hallucinations and form of parkinsonism is called ‘drug-induced Parkinson’s. parkinsonism’. While these drugs are used primarily as People with idiopathic Parkinson’s disease antipsychotic agents, it is important to note and other causes of parkinsonism may also that they can be used for other non-psychiatric develop worsening symptoms if treated with uses, such as control of nausea and vomiting. such medication inadvertently. For people with Parkinson’s, other anti-sickness drugs such as domperidone (Motilium) or What drugs cause drug-induced ondansetron (Zofran) would be preferable. parkinsonism? Any drug that blocks the action of dopamine As well as neuroleptics, some other drugs (referred to as a dopamine antagonist) is likely can cause drug-induced parkinsonism. to cause parkinsonism. Drugs used to treat These include some older drugs used to treat schizophrenia and other psychotic disorders high blood pressure such as methyldopa such as behaviour disturbances in people (Aldomet); medications for dizziness and with dementia (known as neuroleptic drugs) nausea such as prochlorperazine (Stemetil); are possibly the major cause of drug-induced and metoclopromide (Maxolon), which is parkinsonism worldwide. -

Top Prescription Drugs Older Adults Should Avoid Page 1 of 2
Top Prescription Drugs Older Adults Should Avoid page 1 of 2 Drug Problem Pain relievers amitriptyline (elavil) Amitriptyline can cause dry mouth, constipation, drowsiness, confusion and even hallucinations. indomethacin (indocin) Of all nonsteroidal anti-inflammatory drugs, indomethacin affects the brain the most. It can cause confusion or dizziness. narcotics Propoxyphene (Darvon) These are all opioids. Any opioid can cause constipation, urinary and combination products retention, drowsiness and confusion. However, those listed here that includes it (Darvocet-n) are particularly problematic. Propoxyphene, the main ingredient in Darvon and Darvocet, provides no more pain relief than acetaminophen. It may interfere with sleep and cause confusion. meperidine (Demerol) Meperidine lowers the seizure threshold in older adults, particularly those with renal insufficiency. It may be more likely to cause confusion than other narcotics. Pentazocine (talwin) Pentazocine is more likely to cause confusion and hallucinations than other opioids. antiDePressants Fluoxetine (Prozac) Fluoxetine’s effect lasts a long time. It may cause sleep taken daily disturbances, restlessness and increased agitation. It also may decrease appetite in some older adults who do not need to lose weight. If used, consider once weekly dosing. Doxepin (sinequan) Used to treat depression or sleep. These medications can amitriptyline (elavil) cause sedation, weakness, blood pressure changes, dry mouth, problems with urination, and can lead to falls and fractures. These are rarely the drugs of choice for older adults. clevelandclinic.org/geriatrics 10-GER-004 Top Prescription Drugs Older Adults Should Avoid page 2 of 2 Drug Problem sleeP anD anti-anxiety meDications benzodiazepines (long-acting): The effect of these medications last a long time (often days) Flurazepam (Dalmane) producing prolonged sedation and increasing the incidence of falls Diazepam (valium) and fractures. -

Table 1: Drug-Drug Interactions of Common Cardiac Drugs and Chemotherapeutic Agents*
Table 1: Drug-Drug Interactions of Common Cardiac Drugs and Chemotherapeutic Agents* Cardiac Drug(s) Enzyme/ Chemotherapy Effect of Drug- Suggested Oncologist Suggested Cardiologist Action Drug† Drug Management Management Interaction Beta-Blockers All beta- Additive Ceritinib Additive Avoid using the combination of ceritinib with beta- blockers clinical bradycardia blockers. If concomitant use is necessary and symptomatic effect bradycardia occurs, hold ceritinib, adjust or discontinue the beta-blocker, and upon recovery resume ceritinib at a reduced dose with frequent monitoring of heart rate.‡ Crizotinib Monitor blood pressure and heart rate regularly. Dose reduction or discontinuation of one of the agents may be necessary if clinically significant bradycardia occurs.‡ Carvedilol P-gp Afatinib ↑ Monitor for adverse Consider alternative agent if inhibition chemotherapy effects of afatinib. If possible. (moderate) drug not well-tolerated, concentration decrease afatinib daily dose by 10 mg. Doxorubicin Monitor for adverse Consider alternative agent if Nilotinib effects of possible. If carvedilol is used for Paclitaxel chemotherapy drug if prevention of anthracycline Pazopanib concomitant therapy is cardiotoxicity, individual risk vs. Vincristine necessary. benefit must be considered. If Vinblastine concomitant therapy is necessary and drug-drug interaction involves QT- prolonging chemotherapy drug, ensure appropriate electrocardiographic (ECG) and electrolyte monitoring. Carvedilol; CYP2D6 Imatinib ↑ beta-blocker Monitor blood pressure