Cross-Reactivity of Sulfonamide Drugs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019): a Cross-Sectional Study
Tropical Medicine and Infectious Disease Article National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019): A Cross-Sectional Study Joseph Sam Kanu 1,2,* , Mohammed Khogali 3, Katrina Hann 4 , Wenjing Tao 5, Shuwary Barlatt 6,7, James Komeh 6, Joy Johnson 6, Mohamed Sesay 6, Mohamed Alex Vandi 8, Hannock Tweya 9, Collins Timire 10, Onome Thomas Abiri 6,11 , Fawzi Thomas 6, Ahmed Sankoh-Hughes 12, Bailah Molleh 4, Anna Maruta 13 and Anthony D. Harries 10,14 1 National Disease Surveillance Programme, Sierra Leone National Public Health Emergency Operations Centre, Ministry of Health and Sanitation, Cockerill, Wilkinson Road, Freetown, Sierra Leone 2 Department of Community Health, Faculty of Clinical Sciences, College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown, Sierra Leone 3 Special Programme for Research and Training in Tropical Diseases (TDR), World Health Organization, 1211 Geneva, Switzerland; [email protected] 4 Sustainable Health Systems, Freetown, Sierra Leone; [email protected] (K.H.); [email protected] (B.M.) 5 Unit for Antibiotics and Infection Control, Public Health Agency of Sweden, Folkhalsomyndigheten, SE-171 82 Stockholm, Sweden; [email protected] 6 Pharmacy Board of Sierra Leone, Central Medical Stores, New England Ville, Freetown, Sierra Leone; [email protected] (S.B.); [email protected] (J.K.); [email protected] (J.J.); [email protected] (M.S.); [email protected] (O.T.A.); [email protected] (F.T.) Citation: Kanu, J.S.; Khogali, M.; 7 Department of Pharmaceutics and Clinical Pharmacy & Therapeutics, Faculty of Pharmaceutical Sciences, Hann, K.; Tao, W.; Barlatt, S.; Komeh, College of Medicine and Allied Health Sciences, University of Sierra Leone, Freetown 0000, Sierra Leone 8 J.; Johnson, J.; Sesay, M.; Vandi, M.A.; Directorate of Health Security & Emergencies, Ministry of Health and Sanitation, Sierra Leone National Tweya, H.; et al. -

Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications
International Journal of Molecular Sciences Review Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications Daniel Fernández-Villa 1, Maria Rosa Aguilar 1,2 and Luis Rojo 1,2,* 1 Instituto de Ciencia y Tecnología de Polímeros, Consejo Superior de Investigaciones Científicas, CSIC, 28006 Madrid, Spain; [email protected] (D.F.-V.); [email protected] (M.R.A.) 2 Consorcio Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-915-622-900 Received: 18 September 2019; Accepted: 7 October 2019; Published: 9 October 2019 Abstract: Bacterial, protozoan and other microbial infections share an accelerated metabolic rate. In order to ensure a proper functioning of cell replication and proteins and nucleic acids synthesis processes, folate metabolism rate is also increased in these cases. For this reason, folic acid antagonists have been used since their discovery to treat different kinds of microbial infections, taking advantage of this metabolic difference when compared with human cells. However, resistances to these compounds have emerged since then and only combined therapies are currently used in clinic. In addition, some of these compounds have been found to have an immunomodulatory behavior that allows clinicians using them as anti-inflammatory or immunosuppressive drugs. Therefore, the aim of this review is to provide an updated state-of-the-art on the use of antifolates as antibacterial and immunomodulating agents in the clinical setting, as well as to present their action mechanisms and currently investigated biomedical applications. Keywords: folic acid antagonists; antifolates; antibiotics; antibacterials; immunomodulation; sulfonamides; antimalarial 1. -
Rash During Procedural Sedation for Trimalleolar Fracture
Rash during Procedural Sedation for Trimalleolar Fracture Saint John, Emergency Medicine Case Rounds – 10 October, 2017 Dr. Jacqueline Hiob, BScPharm MD PGY1, FRCP Emergency Medicine Learning points for discussion around… • Response to possible drug reaction during procedural sedation • Options for avoiding or mitigating histamine release reactions to opioids Case 14 y/o M, healthy Fall from bicycle ~ 1 hour prior to presentation to ED No head injury, no LOC c/o pain and swelling R. ankle Unable to ambulate Transport by EMS – pt splinted on route, extremity NVI, Entonox for analgesia Case In the ED…. - Entonox Acetaminophen, Fentanyl - closed R. ankle injury, remains NVI - BP 145/72, P 90, S 96% RA, T 36.8 - off to xray he goes…. Imaging - Comminuted fractures, distal tibia + fibula - Apex medial and posterior angulation - Ankle and growth plate intact Case - Ortho consulted - Ortho R3 arrives in ED to assist with reduction - Full team: ED attending, ED resident, Emerg CC3, Ortho resident, RN, RN (training), RT, RT (student), LPN, X-Ray Tech Case Balanced Procedural Sedation with…. - Fentanyl - Ketamine - Propofol Case - ~ 20 minutes into procedure, macular rash noted over patients chest, progressing over abdomen - - no airway involvement, no hypotension or tachycardia - - decision made to treat with IV diphenhydramine and have epinephrine on hand ** smaller area of involvement than pictured - meds for anaphylaxis not immediately available and nurse sent to retrieve Case - Reduction completed within few minutes of rash presentation - Rash -

Eslicarbazepine Acetate Longer Procedure No
European Medicines Agency London, 19 February 2009 Doc. Ref.: EMEA/135697/2009 CHMP ASSESSMENT REPORT FOR authorised Exalief International Nonproprietary Name: eslicarbazepine acetate longer Procedure No. EMEA/H/C/000987 no Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted. product Medicinal 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) 74 18 84 16 E-mail: [email protected] http://www.emea.europa.eu TABLE OF CONTENTS 1. BACKGROUND INFORMATION ON THE PROCEDURE........................................... 3 1.1. Submission of the dossier ...................................................................................................... 3 1.2. Steps taken for the assessment of the product..................................................................... 3 2. SCIENTIFIC DISCUSSION................................................................................................. 4 2.1. Introduction............................................................................................................................ 4 2.2. Quality aspects ....................................................................................................................... 5 2.3. Non-clinical aspects................................................................................................................ 8 2.4. Clinical aspects.................................................................................................................... -

The Local Use of the Sulfonamide Drugs
THE LOCAL USE OF THE SULFONAMIDE DRUGS GEORGE CRILE Jr., M.D. Since the introduction of sulfanilamide and its derivatives, the reliance upon chemotherapy for the control of acute surgical infections has temporarily overshadowed the importance of sound surgical princi- ples and often has resulted in the administration of inefficient or inade- quate treatment. Too often, the physician fails to recognize the limita- tions of chemotherapy and vainly attempts to control the infection well beyond the optimum time for surgical intervention. Chemotherapy is very effective in controlling infections from hemo- lytic streptococcus; is moderately effective in controlling staphylococcic infections; but is of slight value when administered systemically in patients infected with the nonhemolytic streptococcus or colon bacillus. However, even in infections caused by the hemolytic streptococcus or the staphylococcus, sulfanilamide and sulfathiazole cannot replace surgery after suppuration has taken place and mechanical drainage of an abscess is required. It is in the treatment of lymphangitis and cellulitis, not in the treatment of abscesses, that chemotherapy has been of the greatest value. The work of Lockwood1 and others has indicated that the products of proteolysis in vitro interfere with the bacteriostatic and bacteriocidal powers of sulfanilamide. The presence of similar substances in undrained abscess cavities probably interferes with the destruction of the organ- isms by chemotherapy. Accordingly, the sulfonamide drugs should supplement rather than replace early and adequate surgical drainage, especially in the presence of suppuration. The local application of the sulfonamide drugs is based upon the principle that the local concentration of the drug in the tissues is ten to twenty times as high as that which can be obtained by any method of systemic administration. -

Infection Prevention in Combat-Related Injuries CPG ID: 24 APPENDIX B: POST-INJURY ANTIMICROBIAL AGENT SELECTION and DURATION BASED UPON INJURY PATTERN
Infection Prevention in Combat-Related Injuries CPG ID: 24 APPENDIX B: POST-INJURY ANTIMICROBIAL AGENT SELECTION AND DURATION BASED UPON INJURY PATTERN INJURY PREFERRED AGENT(S) ALTERNATE AGENT(S) DURATION EXTREMITY WOUNDS (INCLUDES SKIN, SOFT TISSUE, BONE) Skin, soft tissue, no open fractures Cefazolin, 2 gm IV q6-8h†‡ Clindamycin (300-450 mg PO TID or 600 mg IV q8h) 1-3 days Skin, soft tissue, with open Cefazolin 2 gm IV q6-8h†‡§ Clindamycin 600 mg IV q8h 1-3 days fractures, exposed bone, or open joints THORACIC WOUNDS Penetrating chest injury without Cefazolin, 2 gm IV q6-8h†‡ Clindamycin (300-450 mg PO TID or 600 mg IV q8h) 1 day esophageal disruption Penetrating chest injury with Cefazolin 2 gm IVq 6-8h†‡ PLUS metronidazole 500 Ertapenem 1 gm IV x 1 dose, OR moxifloxacin 400 mg 1 day after definitive esophageal disruption mg IV q8-12h IV x 1 dose washout ABDOMINAL WOUNDS Penetrating abdominal injury with Cefazolin 2 gm IV q 6-8h†‡ PLUS metronidazole 500 Ertapenem 1 gm IV x 1 dose, OR moxifloxacin 400 mg 1 day after definitive suspected/known hollow viscus mg IV q8-12h IV x 1 dose washout injury and soilage; may apply to rectal/perineal injuries as well MAXILLOFACIAL AND NECK WOUNDS Open maxillofacial fractures, or Cefazolin 2 gm IV q6-8h†‡ Clindamycin 600 mg IV q8h 1 day maxillofacial fractures with foreign body or fixation device CENTRAL NERVOUS SYSTEM WOUNDS Penetrating brain injury Cefazolin 2 gm IV q6-8h.†‡ Consider adding Ceftriaxone 2 gm IV q24h. Consider adding 5 days or until CSF metronidazole 500 mg IV q8-12h if gross metronidazole 500 mg IV q8-12h if gross contamination with organic debris contamination with organic debris. -

The Impact of Saccharin on Saccharomyces Cerevisiae Yeast
Journal of Undergraduate Biology Laboratory Investigations 2018 The Impact of Saccharin on Saccharomyces Cerevisiae Yeast Fermentation Parker Brown, Megan Hanson, Edison Huo, Derica Smith, and Bianca Galletti * 1 University of Oklahoma, Department of Biology, 730 Van Vleet Oval, Room 314 Norman, OK 73019 _________________________________________________________________________________________ Previous research has shown that mammals struggle to metabolize sugar substitutes such as saccharin. But these results are less clear when it comes to microorganisms such as yeast. Because many animals cannot metabolize saccharin, we hypothesize that yeast growth will be less in saccharin dominate solutions as compared to glucose dominate solutions. To test this, differing solutions of glucose and saccharin were fed to Saccharomyces cerevisiae, a yeast type which uses the Crabtree Effect to carry out alcoholic fermentation in the presence of glucose. Like in animals, it was found that saccharin also negatively impacts the growth of yeast meaning that saccharin could not be used in industrial processes wishing to use yeast to make ethanol. _________________________________________________________________________________________ Introduction sugars in processes requiring yeast growth such as In the last several decades, sugar substitutes the alcoholic beverage industry. have become more common in the food and Because yeast is a commonly used organism beverage industry as they allow “healthier” low in the food industry, the process of yeast calorie foods to be produced and marketed to fermentation has been well established. In certain consumers. However, these sugar substitutes have types of yeast, such as Saccharomyces cerevisiae, not been introduced without controversy with past yeast can utilize glucose to undergo alcoholic research voicing their harmful impacts and others fermentation in what is called the Crabtree Effect revealing no deleterious impacts (Sharma et. -
Xifaxan® (Rifaximin)
Wednesday, October 14, 2015 4 p.m. Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review Board Members FROM: Bethany Holderread, Pharm.D. SUBJECT: Packet Contents for Board Meeting – October 14, 2015 DATE: October 1, 2015 NOTE: The DUR Board will meet at 4:00 p.m. The meeting will be held at 4345 N Lincoln Blvd. Enclosed are the following items related to the October meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Action Item – Vote on 2016 Meeting Dates – Appendix B Update on Medication Coverage Authorization Unit/Bowel Preparation Medication Post-Educational Mailing – Appendix C Action Item – Vote to Prior Authorize Tykerb® (Lapatinib), Halaven® (Eribulin), Ixempra® (Ixabepilone), Kadcyla® (Ado-Trastuzumab), Afinitor® (Everolimus), & Perjeta® (Pertuzumab) – Appendix D Action Item – Vote to Prior Authorize Orkambi™ (Lumacaftor/Ivacaftor) – Appendix E Action Item – Vote to Prior Authorize Savaysa® (Edoxaban) – Appendix F Action Item – Vote to Prior Authorize Epanova® (Omega-3-Carboxylic Acids), Praluent® (Alirocumab), & Repatha™ (Evolocumab) – Appendix G Annual Review of Constipation and Diarrhea Medications and 30-Day Notice to Prior Authorize Movantik™ (Naloxegol), Viberzi™ (Eluxadoline), & Xifaxan® (Rifaximin) – Appendix H 30-Day Notice to Prior Authorize Daraprim® (Pyrimethamine) – Appendix I Annual Review of Allergy Immunotherapies and 30-Day Notice to Prior Authorize Oralair® (Sweet Vernal, Orchard, Perennial Rye, Timothy, & Kentucky Blue Grass Mixed Pollens Allergen Extract) – Appendix J Annual Review of Non-Steroidal Anti-Inflammatory Drugs and 30-Day Notice to Prior Authorize Dyloject™ (Diclofenac Sodium) – Appendix K ORI-4403 • P.O. -

Belgian Veterinary Surveillance of Antibacterial Consumption
Belgian Veterinary Surveillance of Antibacterial Consumption National consumption report 2013 1 Summary This fifth BelVetSAC report, covers the results of the data collection on veterinary antibacterial consumption in Belgium in the year 2013. Data consist of all veterinary antibacterials sold to a veterinarian or pharmacist in Belgium and of antibacterial premixes incorporated in medicated feed intended to be used in Belgium for the year 2013. It includes thus consumption data for farm animals as well as companion animals. The denominator for animal production was the biomass (in kg) calculated as the sum of the amount of beef, pork and poultry meat produced in 2013, plus the number of dairy cattle present in Belgium times 500 kg of metabolic weight per head. As the usage data are concerned, this report shows for the second year in a row a decrease in the total consumption of antibacterial compounds in veterinary medicine of -6,6% between 2012 and 2013. Due to the relative stable animal production (expressed in biomass -0,3%) the decrease expressed in mg/kg biomass is -6,3%. When using 2011 as a reference, a reduction of -12,7% (expressed in mg/kg biomass) was achieved between 2011 and 2013, distributed over a reduction of -13,3% in antibacterial pharmaceuticals and -10,2% in antibacterial premixes. When looking more in detail to the different types of antibacterials used, it is observed that the penicillines (31,1%), sulphonamides (28,7%), and tetracyclines (24,1%) remain the three most used antibacterial classes. This year a substantial decrease in sulphonamide plus trimethoprim use and a limited decrease in penicillin and tetracycline use was observed. -
Blood Cell Changes in Complement Activation- Related Pseudoallergy
Eur. J. Nanomed. 2015; 7(3): 233–244 Mini Review Zsófia Patkó* and János Szebeni Blood cell changes in complement activation- related pseudoallergy DOI 10.1515/ejnm-2015-0021 Introduction Received April 13, 2015; accepted May 19, 2015 Complement activation-related pseudoallergy (CARPA), as the name implies, is a non-Ig-E-mediated (pseudo- Abstract: The characteristic physiological changes allergic) hypersensitivity reaction (HSR) that is triggered in complement (C) activation-related pseudoallergy by C activation, or C activation plays a major contributing (CARPA) include thrombocytopenia, leukocytosis and role. CARPA is best known in the context of nanotoxicity, leukopenia with or without compensatory leukocytosis. since nanomedicines, i.e. particulate drugs and agents in In the background of these phenomena it is known that the nano (10−9–10 −6 m) size range often cause such reac- anaphylatoxins, the triggers of CARPA, can activate white tions. As reviewed earlier (1–8), and also discussed in blood cells (WBCs) and platelets, and that this activation other papers of this issue, the phenomenon represents can lead to the binding of these cells to each other and an immune barrier to the clinical use of many promising also to capillary endothelial cells, entailing microthrom- nanomedicines. In essence, CARPA may be perceived as bus formation and circulatory blockage mainly in the pul- a biological stress on blood that arises as a consequence monary and coronary microcirculation. These changes of the similarity of nanomedicines to viruses, between are key contributors to the hemodynamic alterations in which the immune system cannot make difference (8). CARPA, and can lead to anaphylactic shock. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -
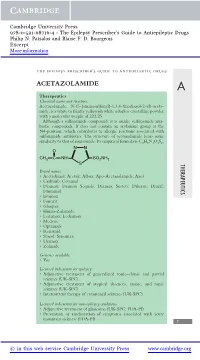
Acetazolamide
Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N. Patsalos and Blaise F. D. Bourgeois Excerpt More information the epilepsy prescriber’s guide to antiepileptic drugs ACETAZOLAMIDE A Therapeutics Chemical name and structure: Acetazolamide, N-(5-(aminosulfonyl)-1,3,4-thiadiazol-2-yl)-aceta- mide, is a white to faintly yellowish white odorless crystalline powder with a molecular weight of 222.25. Although a sulfonamide compound, it is unlike sulfonamide anti- biotic compounds. It does not contain an arylamine group at the N4-position, which contributes to allergic reactions associated with sulfonamide antibiotics. The structure of acetazolamide bears some similarity to that of zonisamide. Its empirical formula is C4H6N4O3S2. NN O CH3 CNH SO2NH2 S THERAPEUTICS Brand names: r Acetadiazol; Acetak; Albox; Apo-Acetazolamide; Azol r Carbinib; Cetamid r Diamox; Diamox Sequals; Diamox Sustets; Diluran; Diural; Diuramid r Evamox r Fonurit r Glaupax r Huma-Zolamide r Ledamox; Lediamox r Medene r Optamide r Renamid r Stazol; Synomax r Uramox r Zolmide Generics available: r Yes Licensed indications for epilepsy: r Adjunctive treatment of generalized tonic–clonic and partial seizures (UK-SPC) r Adjunctive treatment of atypical absences, atonic, and tonic seizures (UK-SPC) r Intermittent therapy of catamenial seizures (UK-SPC) Licensed indications for non-epilepsy conditions: r Adjunctive treatment of glaucoma (UK-SPC; FDA-PI) r Prevention or amelioration of symptoms associated with acute mountain sickness (FDA-PI) 1 © in this web service Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-68716-4 - The Epilepsy Prescriber’s Guide to Antiepileptic Drugs Philip N.