Alcohol and Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetes Medications: Oral Medications
Diabetes Medications: Oral Medications Medication Types 1. Biguanides 2. Sulfonylureas 3. Thiazolidinediones (TZDs) 4. Alpha-Glucosidase Inhibitors 5. D-Phenylalanine Meglitinides 6. SGLT-2 inhibitors 7. DPP-4 inhibitors 8. Combination Oral Medications 1. Biguanides This works by lowering blood glucose by reducing the amount of glucose produced by the liver and helping the body respond better to the insulin made in the pancreas Metformin can be used with diet and exercise or with other agents, diet, and exercise. Types of Biguanides: • Metformin (Glucophage) 500mg/1000mg • Metformin (Glucophage XR) 500mg/1000mg • Fortamet (extended release) 500mg/1000mg • Riomet (oral solution) 500mg/5ml Side Effects: • Cramping • Gas • Diarrhea • Taking the pill before meals may decrease stomach upset 2. Sulfonylureas Sulfonylureas stimulate the pancreas to produce insulin and cause the body to respond better to the insulin it does produce. Sulfonylureas can be used alone or in combination with other medications. Types of Sulfonylureas: • Glimepiride (Amaryl) • Glipizide (Glucotrol, Glucotrol XL) • Glyburide (Diabeta, Micronase) • Glyburide, micronized (Glynase) • Tolbutamide (Orinase) 1st generation • Tolazamide (Tolinase) 1st generation • Acetohexamide (Dymelor) 1st generation • Chlorpropamide (Diabinese) 1st generation Side Effects: • Hypoglycemia • Upset stomach • Weight gain • Skin rash 3. Thiazolidinediones (TZDs) TZDs primarily reduce insulin resistance by improving target cell response (sensitivity) to insulin. They also can decrease glucose output from the liver and increase glucose disposal in the skeletal muscles. Types of TZDs: • Pioglitazione (Actos) 15-45 mg Actos may be taken with or without food • Avandia—off the market Side Effects: • Jaundice • Nausea and vomiting • Stomach pain • Dark urine • Swelling • These medicines are generally safe and do not cause hypoglycemia when used alone. -

Orange Book Patent Listing Dispute List
Patent Listing Disputes Current through September 10, 2021 Established Drug Product Due Date for NDA Holder NDA Holder NDA Number NDA Holder Strength(s) Relevant U.S. Patent Number(s) Type of Patent Claim Original Use Code (if applicable) Revised Use Code (if applicable) Dispute Outcome Name Response Response Date Disputes Not Related to epinephrine 205029 Belcher 1mg/mL 10,004,700 and 10,039,728 N/A N/A 7/24/2021 Pending Pending Use Code 7 mg 14 mg 8,168,209, 8,173,708, 8,283,379, Disputes Not Related to memantine hydrochloride 22525 Allergan Sales LLC N/A N/A 5/28/2021 5/28/2021 Patent Listing Updated 21 mg 8,329,752, 8,362,085 and 8,598,233 Use Code 28 mg 0.1 mg Disputes Not Related to epinephrine 201739 Kaleo Inc 0.15 mg 10,824,938 N/A N/A 2/28/2021 2/3/2021 Patent Listing Updated Use Code 0.3 mg Disputes Not Related to netarsudil and latanoprost 208259 Aerie Pharms Inc 0.02%/0.005% 10,654,844 N/A N/A 11/18/2020 10/30/2020 Patent Listing Updated Use Code Disputes Not Related to netarsudil 208254 Aerie Pharms Inc 0.02% 10,654,844 N/A N/A 11/18/2020 10/30/2020 Patent Listing Updated Use Code U-2869: IV Administration of cangrelor before U-2979: Method comprising IV administration PCI and continuous infusion for at least 2 of cangrelor before PCI then continuous hours or the duration of the PCI and, during infusion for at least 2 hours or the duration of cangrelor 204958 Chiesi 50 mg/vial 8,680,052 Method of Use 11/8/2020 11/3/2020 Patent Listing Updated or after the continuous infusion, PCI and, during or after continuous infusion, -

Association Between Serious Hypoglycemia and Calcium-Channel Blockers Used Concomitantly with Insulin Secretagogues
Research Letter | Diabetes and Endocrinology Association Between Serious Hypoglycemia and Calcium-Channel Blockers Used Concomitantly With Insulin Secretagogues Young Hee Nam, PhD; Colleen M. Brensinger, MS; Warren B. Bilker, PhD; James H. Flory, MD; Charles E. Leonard, MSCE, PharmD; Sean Hennessy, PhD, PharmD Introduction + Supplemental content Serious hypoglycemia is a major, potentially fatal adverse event caused by insulin secretagogues.1 Author affiliations and article information are Previous case reports suggested that calcium-channel blockers (CCBs) might reduce the risk of listed at the end of this article. serious hypoglycemia in patients with hyperinsulinemic hypoglycemia.2,3 However, the association of serious hypoglycemia and CCBs used with insulin secretagogues has remained unclear. Because insulin secretion by the pancreas is mediated by calcium influx in beta cells through calcium channels,4 we conducted a population-based observational study on the hypothesis that concomitant use of CCBs may be associated with reduced rates of serious hypoglycemia in insulin secretagogue users. Methods This self-controlled case series study was approved by the institutional review board of the University of Pennsylvania, which waived the requirement for informed consent because the use or disclosure of the protected health information involved no more than minimal risk to the privacy of individuals, and the research could not practicably be conducted without the waiver or alteration and without access to and use of the protected health information. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. We used claims data from the Medicaid programs of 5 US states (California, Florida, New York, Ohio, and Pennsylvania, encompassing more than a third of the nationwide Medicaid population), supplemented with Medicare claims for dual enrollees, from January 1, 1999, to December 31, 2011, and used the self- controlled case series design. -

Oregon Drug Use Review / Pharmacy & Therapeutics Committee
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program OHA Division of Medical Assistance Programs 500 Summer Street NE, E35; Salem, OR 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Oregon Drug Use Review / Pharmacy & Therapeutics Committee Thursday, July 26, 2018 1:00 - 5:00 PM HP Conference Room 4070 27th Ct. SE Salem, OR 97302 MEETING AGENDA NOTE: Any agenda items discussed by the DUR/P&T Committee may result in changes to utilization control recommendations to the OHA. Timing, sequence and inclusion of agenda items presented to the Committee may change at the discretion of the OHA, P&T Committee and staff. The DUR/P&T Committee functions as the Rules Advisory Committee to the Oregon Health Plan for adoption into Oregon Administrative Rules 410-121-0030 & 410-121-0040 as required by 414.325(9). I. CALL TO ORDER 1:00 PM A. Roll Call & Introductions R. Citron (OSU) B. Conflict of Interest Declaration R. Citron (OSU) C. Approval of Agenda and Minutes T. Klein (Chair) D. Department Update T. Douglass (OHA) E. Legislative Update T. Douglass (OHA) F. Mental Health Clinical Advisory Group Discussion K. Shirley (MHCAG) 1:40 PM II. CONSENT AGENDA TOPICS T. Klein (Chair) A. P&T Methods B. CMS and State Annual Reports C. Quarterly Utilization Reports 1. Public Comment III. DUR ACTIVITIES 1:45 PM A. ProDUR Report R. Holsapple (DXC) B. RetroDUR Report D. Engen (OSU) C. Oregon State Drug Reviews K. Sentena (OSU) 1. A Review of Implications of FDA Expedited Approval Pathways, Including the Breakthrough Therapy Designation IV. -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -
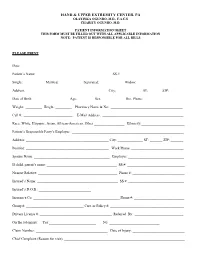
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________ -

Download Product Insert (PDF)
PRODUCT INFORMATION Nateglinide Item No. 23320 CAS Registry No.: 105816-04-4 Formal Name: N-[[trans-4-(1-methylethyl)cyclohexyl] O OH carbonyl]-D-phenylalanine Synonyms: A-4166, SDZ-DJN 608 O MF: C H NO 19 27 3 N FW: 317.4 Purity: ≥98% H UV/Vis.: λmax: 207 nm Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Nateglinide is supplied as a crystalline solid. A stock solution may be made by dissolving the nateglinide in the solvent of choice. Nateglinide is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide, which should be purged with an inert gas. The solubility of nateglinide in these solvents is approximately 30 mg/ml. Description Nateglinide is a hypoglycemic agent.1-3 It induces insulin and somatostatin release from perfused rat pancreas when used at concentrations ranging from 0.03 to 3 μM.1 Nateglinide (3 µM) increases intracellular calcium levels in isolated rat pancreatic β cells, an effect that can be inhibited by the L-type calcium channel blocker nitrendipine (Item No. 17549). Nateglinide-induced secretion of insulin and somatostatin and calcium influx is also reversed by the potassium channel activator diazoxide (Item No. 14576). Oral administration of nateglinide (1.6 mg/kg) reduces blood glucose levels by 20% in fasted mice.2 It also decreases blood glucose levels in an oral glucose tolerance test in normal rats, genetically diabetic KK mice, and a rat model of diabetes induced by streptozotocin (STZ; Item No. -

Ambetter 90-Day-Maintenance Drug List- 2020
Ambetter 90-Day-Maintenance Drug List Guide to this list: What is Ambetter 90‐Day‐Maintenance Drug List? Ambetter 90‐Day‐Supply Maintenance Drug List is a list of maintenance medications that are available for 90 day supply through mail order or through our Extended Day Supply Network. How do I find a pharmacy that is participating in Extended Day Supply Network? To find a retail pharmacy that is participating in our Extended Day Supply Network please consult information available under Pharmacy Resources tab on our webpage. Alternatively, you can utilize our mail order pharmacy. Information on mail order pharmacy is available in Pharmacy Resources tab on our webpage. Are all formulary drugs covered for 90 day supply? No, certain specialty and non‐specialty drugs are excluded from 90 day supply. Please consult 90‐Day‐ Supply Maintenance Drug List for information if your drug is included. A Amitriptyline HCl Acamprosate Calcium Amlodipine Besylate Acarbose Amlodipine Besylate-Atorvastatin Calcium Acebutolol HCl Amlodipine Besylate-Benazepril HCl Acetazolamide Amlodipine Besylate-Olmesartan Medoxomil Albuterol Sulfate Amlodipine Besylate-Valsartan Alendronate Sodium Amlodipine-Valsartan-Hydrochlorothiazide Alendronate Sodium-Cholecalciferol Amoxapine Alfuzosin HCl Amphetamine-Dextroamphetamine Aliskiren Fumarate Anagrelide HCl Allopurinol Anastrozole Alogliptin Benzoate Apixaban Alosetron HCl Arformoterol Tartrate Amantadine HCl Aripiprazole Amiloride & Hydrochlorothiazide Armodafinil Amiloride HCl Asenapine Maleate Amiodarone HCl Aspirin-Dipyridamole -

Unusual Case of Necrotizing Pneumonia Rajapriya Manickam*, Kabir Oladipo Olaniran and Raghu Loganathan
Manickam et al. Int J Respir Pulm Med 2015, 2:2 International Journal of ISSN: 2378-3516 Respiratory and Pulmonary Medicine Case Report : Open Access Unusual Case of Necrotizing Pneumonia Rajapriya Manickam*, Kabir Oladipo Olaniran and Raghu Loganathan Division of Pulmonary and Critical care Medicine, Lincoln Medical and Mental Health Center, USA *Corresponding author: Rajapriya Manickam, Division of Pulmonary and Critical care Medicine, Lincoln Medical and Mental Health Center, Bronx, New York, USA, Tel: 917-375-5626; E-mail: [email protected] Abstract Coccidioidomycosis is caused by inhalation of Coccidoides spores which is endemic in south western parts of USA and an uncommon cause of pneumonia in non-endemic areas. We report a young Hispanic man who lives in New York presenting with diabetic ketoacidosis and severe pulmonary Coccidioidomycosis. Through this case report and review we want to familiarize clinicians from non-endemic area to this unusual cause for necrotizing pneumonia, its association with diabetes mellitus, other risk factors for dissemination and the management strategy. Introduction Pulmonary Coccidioidomycosis is an uncommon cause of necrotizing pneumonia in non-endemic areas. We report a case of severe pulmonary Coccidioidomycosis in a young immigrant who lives in New York and discuss the association with diabetes mellitus. Hospital Course A young 32 year old Hispanic man presented with 4-weeks history of polyuria, polyphagia and weight loss and 2-weeks history Figure 1: Chest radiograph showing right upper lobe consolidation and of hemoptysis and shortness of breath. He denied fever, chills, night retraction of horizntal fissure. sweats, sick contacts, skin rash, glandular swelling or recent travel. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Pharmacovigilance - Post
PHARMACOVIGILANCE - POST MARKETING SURVEILLANCE NEWS Vol. 7 No. 3: Third Quarter Newsletter 2014 Editor’s Note I wish to thank all our numerous stakeholders who have been working tirelessly with the National Pharmacovigilance Centre (NPC) to ensure the safe use of medicines in Nigeria. The NPC is committed to sending quarterly newsletter to its stakeholders. The objectives of the Newsletter are to disseminate information on pharmacovigilance activities nationally and globally, to educate stakeholders on medicine safety issues, to promote rational use of drugs and to promote spontaneous reporting. This third quarter Newsletter focuses on Pharmacovigilance of Antidiabetic Drugs. We encourage all Health Care Professionals, Marketing Authorization Holders and other stakeholders to continue to report all adverse drug reactions. Your valued comments and acknowledgement of receipt of this issue through our email addresses ([email protected]; pharmacovigilance@nafdac,gov.ng ) would be most appreciated. Pharm. (Mrs.) Osakwe Director/NationalCoordinator, National Pharmacovigilance Centre (NPC) National Agency for Food and Drug Administration and Control (NAFDAC) Plot 2032 Olusegun Obasanjo Way Wuse Zone 7 Abuja PMB 5032 Wuse Abuja. Telephone 07098211221, 08086899571 E-mail: [email protected]; [email protected]; [email protected]; Website :www.nafdac.gov.ng Text any DRUG RELATED PROBLEM to SHORT CODE 20543 (for free on MTN, GLO and Etisalat) for action by the Pharmacovigilance Centre 1 PHARMACOVIGILANCE OF ANTIDIABETIC DRUGS Diabetes is one of the major causes of illnesses and deaths globally, and it affects many regardless of age or race. This disease can contribute to other health complications such as heart disease, kidney disease and blindness if not properly treated.