Bowel and Bladder Care IHSS Education
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The 007Th Minute Ebook Edition
“What a load of crap. Next time, mate, keep your drug tripping private.” JACQUES A person on Facebook. STEWART “What utter drivel” Another person on Facebook. “I may be in the minority here, but I find these editorial pieces to be completely unreadable garbage.” Guess where that one came from. “No, you’re not. Honestly, I think of this the same Bond thinks of his obituary by M.” Chap above’s made a chum. This might be what Facebook is for. That’s rather lovely. Isn’t the internet super? “I don’t get it either and I don’t have the guts to say it because I fear their rhetoric or they’d might just ignore me. After reading one of these I feel like I’ve walked in on a Specter round table meeting of which I do not belong. I suppose I’m less a Bond fan because I haven’t read all the novels. I just figured these were for the fans who’ve read all the novels including the continuation ones, fan’s of literary Bond instead of the films. They leave me wondering if I can even read or if I even have a grasp of the language itself.” No comment. This ebook is not for sale but only available as a free download at Commanderbond.net. If you downloaded this ebook and want to give something in return, please make a donation to UNICEF, or any other cause of your personal choice. BOOK Trespassers will be masticated. Fnarr. BOOK a commanderbond.net ebook COMMANDERBOND.NET BROUGHT TO YOU BY COMMANDERBOND.NET a commanderbond.net book Jacques I. -

Minnesotan Invented Life-Saving Catheter « Access Press
Access Press - Minnesota's Disability Community Newspaper Minnesotan invented life-saving catheter by Jane McClure // June 10th, 2011 A medical device which has made life easier for countless people with disabilities and illness has ties to Minnesota. The Foley catheter was invented by St. Cloud native Frederic Foley. A Foley catheter is a flexible tube that is passed through the urethra and into the bladder. The tube has two separated lumens. One lumen is open at both ends, and allows urine to drain out into a collection bag. The other lumen has a valve on the outside end and connects to a balloon at the tip. The balloon is inflated with sterile saline when it lies inside the bladder, in order to stop it from slipping out. Born in St. Cloud in 1891, Foley earned his bachelor’s degree at Yale University, and then attended Johns Hopkins School of Medicine. After graduating from medical school in 1918, Foley worked on the East Coast. He was on the junior surgical staff at Boston’s Peter Brigham Hospital. He was certified by the American Board of Urology in 1937, although several histories note that there are no records of Foley having formal training in urology. He worked as an urologist in Boston until becoming chief of urology at Ancker Hospital in St. Paul. Ancker later became St. Paul-Ramsey Medical Center and is now Regions Hospital. Ancker Hospital was located on the Mississippi River bluff in St. Paul’s West End neighborhood. The site is now occupied by St. Paul Public Schools administration. -

HSOA Archives of Urology a Pilot Study of Foley Catheter Balloon Volumes and Pullout Forces in Females Cadavers
Greenberg JA and Ito TE, Arch Urol 2018 1: 002 HSOA Archives of Urology Pilot Study A Pilot Study of Foley Catheter Introduction Indwelling Foley catheters are used around the world in every Balloon Volumes and Pullout healthcare setting as a means for draining the bladder. Simplified, the Foley catheter is a flexible, hollow tube with an inflatable balloon on Forces in Females Cadavers the indwelling end that functions to keep the catheter from falling James A Greenberg1* and Traci E Ito2 out after it has been placed into the bladder. Despite the ubiquity of this device, the scientifically derived data regarding its use is limited. 1Harvard Medical School, Brigham & Women’s Hospital, Boston, USA As one example, manufacturer guidelines for use of a 16 Fr Foley 2Department of Minimally Invasive Gynecology Surgery, University of catheter with a 5 mL balloon recommends filling the balloon with Louisville Hospital, Louisville, USA 10 mL of sterile water [1]. The 10 mL inflation volume has become an almost universal standard though it is unclear on how this recom- mendation was derived. A search of the literature revealed only one study investigating balloon fill volumes and pull out forces [2]. This study was performed with three male cadavers. While these data may seem trivial, unnecessarily high catheter balloon volumes may influ- ence catheter-associated patient discomfort, leakage around catheter, catheters related trauma to bladder mucosa or urethra, and possibly Catheter-Associated Urinary Tract Infections (CAUTI’s). While the most effective method of reducing Foley catheter relat- Abstract ed complications is by avoiding unnecessary placement, this cannot always be prevented. -

Catheter Associated Urinary Tract Infection (CAUTI) Prevention
Catheter Associated Urinary Tract Infection (CAUTI) Prevention System CAUTI Prevention Team 1 Objectives At the end of this module, the participant will be able to: Identify risk factors for CAUTI Explain the relationship between catheter duration and CAUTI risk List the appropriate indications for urinary catheter insertion and continued use Implement evidence-based nursing practice to decrease the risk and incidence of CAUTI 2 The Problem All patients with an indwelling urinary catheter are at risk for developing a CAUTI. CAUTI increases pain and suffering, morbidity & mortality, length of stay, and healthcare costs. Appropriate indwelling catheter use can prevent about 400,000 infections and 9,000 deaths every year! (APIC, 2008; Gould et al, 2009) 3 2012 National Patient Safety Goal Implement evidence-based practices to prevent indwelling catheter associated urinary tract infections (CAUTI) Insert indwelling urinary catheters according to evidence-based guidelines Limit catheter use and duration Use aseptic technique for site preparation, equipment, and supplies (The Joint Commission (TJC), 2011) 4 2012 National Patient Safety Goal Manage indwelling urinary catheters according to evidence-based guidelines Secure catheters for unobstructed urine flow and drainage Maintain the sterility of the urine collection system Replace the urine collection system when required Collect urine samples using aseptic technique (TJC, 2011) 5 Sources of CAUTI Microorganisms Endogenous Meatal, rectal, or vaginal colonization Exogenous -

Instructions for Clean Catch Urine Collection for Diagnostic Testing
INSTRUCTIONS FOR CLEAN CATCH URINE COLLECTION FOR DIAGNOSTIC TESTING. IMPORTANT CAUTION: PLEASE READ AND FOLLOW ALL DIRECTIONS CAREFULLY. IT IS IMPORTANT THAT THE SPECIMEN BE AS CLEAN AS POSSIBLE FOR ACCURATE RESULTS. Male 1. Thoroughly wash and dry hands. 2. Unscrew cap of the urine specimen cup. To avoid contamination, do not touch inside of cup or cap. Place cap on the counter with the inside facing up. 3. Cleanse external areas as follows: Wipe head of penis in a single motion with first towelette. If not circumcised hold foreskin back before cleansing. 4. Hold the sterile cup in one hand. First urinate a small amount into toilet, then catch the rest of the urine directly into the sterile container without stopping the urine stream. (Urinating a small amount into the toilet first flushes out any contaminating organism). 5. Collect specimen until cup is at least half full. 6. Finish voiding in toilet or bedpan. 7. Replace cap on cup and tighten securely. Female 1. Thoroughly wash and dry hands. 2. Unscrew cap of the urine specimen cup. To avoid contamination, do not touch inside of cup or cap. Place cap on the counter with the inside facing up. 3. Cleanse external areas as follows: With one hand spread the labia and keep spread until the specimen is collected. Wipe inner labia folds front to back in a single motion with the first towelette. Repeat with the second towelette. 4. Keep the labia separated and hold the sterile container with the other hand. Urinate a small amount into toilet, then catch the rest of the urine directly into the sterile container without stopping the urine stream. -

Water Stream in Bidet Toilet Commode As A
Ann Colorectal Res. 2017 March; 5(1):e46479. doi: 10.5812/acr.46479. Published online 2017 March 25. Research Article Water Stream in Bidet Toilet Commode as a Cause of Anterior Anal Fissure: A Case-Control Study Pankaj Garg,1,2,* and Pratiksha Singh2 1Colorectal Surgery Division, Indus Super Specialty Hospital, Mohali, Punjab, India 2Garg Fistula Research Institute, Panchkula, Haryana, India *Corresponding author: Pankaj Garg, Garg Fistula Research Institute, 1042, Sector-15, Panchkula, Haryana, India. Tel: +91-9501011000, Fax: +91-1722594556, E-mail: [email protected] Received 2017 January 09; Revised 2017 February 06; Accepted 2017 March 08. Abstract Background: Water used as a single sharp stream in toilet commode for post defecation cleansing is a common practice in sev- eral countries across the globe including India. Repeated hitting of the anus by water stream could potentially cause injury to the anal canal epithelium and lead to development of fissure-in-ano. As the water stream is emanating from the backside of the toilet commode, the possible injury, if any, would be on the anterior anal canal. Objectives: The present study aimed at determining whether water stream usage in toilet commodes increased the incidence of anterior fissure-in-ano; this was determined by the incidence of anterior fissure-in-ano the study and control groups. Methods: All consecutive fissure-in-ano patients referring to a colorectal clinic from February 2012 to 2015 were included in the study. The patients were classified as a study group (who were using water stream for cleansing purposes in toilet commodes) and a control group (patients who were not using water stream). -

X-EFFECT® BOWL CLEANER Disinfects, Cleans, and Deodorizes with a Fresh Lavender Scent
X-EFFECT® BOWL CLEANER Disinfects, cleans, and deodorizes with a fresh lavender scent X-EFFECT Bowl Cleaner cleans and disinfects toilets, com- modes, and urinals. Bacteria and viruses found in public restrooms can cause odors and create an unsafe environment for building occupants. X-EFFECT Bowl Cleaner offers a con- venient and effective solution for removing bacteria and viruses while leaving a fresh lavender fragrance. For best results, use with common scent products like Airlift® Ultra-Fragrant Urinal Screens, Commode Clips, and Odor Eliminators. EPA Registration Number: 5741-18 Providing quality maintenance and chemical specialty solutions with unparalleled customer service since 1956 X-EFFECT® BOWL CLEANER FEATURES DIRECTIONS FOR USE • Ready-to-use disinfectant cleaner ONE-STEP DISINFECTING AND CLEANING TOILET • Kills the virus that causes COVID-191,2 BOWLS AND URINALS Remove visible soil before disinfection. Empty toilet bowl or urinal and ap- • Broad-spectrum, hospital-grade disinfectant ply product to exposed surfaces with a brush or swab mop. Brush or swab • Formulated for use in daily maintenance programs thoroughly, especially under the rim. Let stand for 10 minutes, then flush. ONE-STEP DISINFECTING CERAMIC TILE, PORCE- BENEFITS LAIN, SHOWER WALLS, FLOORS, AND OTHER HARD, • Cleans as it disinfects NON-POROUS SURFACES • Features a fresh lavender fragrance Remove visible soil before disinfection. Apply X-EFFECT Bowl Cleaner with a cloth, mop, sponge, or coarse sprayer. Treated surfaces must • Ready-to-use formula ensures proper ppm required for disinfection remain wet for 10 minutes. Rinse thoroughly with water. • Pre-labeled, pre-filled quarts offer the ultimate safety and convenience GENERAL DEODORIZING AND CLEANING 1 SARS-Related Coronavirus 2 Dilute X-EFFECT Bowl Cleaner 1:10 (12 oz/gal of water) for general 2 On hard, non-porous surfaces deodorizing and cleaning of hard, nonporous bathroom surfaces. -

Bedpan Management Teleclass Slides, May.12.11
The Faecal Quandary – Bedpan Management in a Modern Age Gertie van Knippenberg-Gordebeke, Netherlands Sponsored by Meiko (www.meiko.de) The Faecal Quandary Disclaimer/Disclosure The findings and conclusions in this presentation are those of the author "Bedpan Management in a Modern Age" Consultant current & past for: Diversey the Netherlands, Hakerman Turkey, Medwaste Control the Netherlands Gertie van Knippenberg-Gordebeke, RN, CCIP Meiko Germany, SCA Hygiene Products Sweden, Sigex Brazil Consultant Infection Prevention [email protected] ΄T Like “It‘s what I “I DON to do DO Best” A Tribute to All Nurses in the Bedpans” Sponsored by: world Webber Teleclass& 10 year Anniversary www.meiko.de Hosted by Paul Webber [email protected] 2 www.webbertraining.com April 12, 2011 Florence Nightingale ‘Lady with the lamp’ (12-05-1820 – 03-08-1910) Do No Harm 12 May International Nursing Day Florence Nightingale & Hippocrates 2011 • Founder professional nursing Healthcare Associated Infections (HAI) • Advocate improvement of care & hygiene ± 10% in Hospitals (Netherlands 6,2%) • Improvement reduced mortality rate from 42% to 2% • Author books & manuscripts* > 25% on Intensive Care > 25% in Low income countries * Notes on Nursing: What is and what is not * Notes on Hospitals: Sanitary techniques to medical facilities Harm what could be prevented 3 4 Risk Factors HAI • Antimicrobial resistance • Human behaviour • Staff-shortage Breaking the chain with basic precautions Nr.1 • Difference in medical- and nursing care structure • Resource availability -
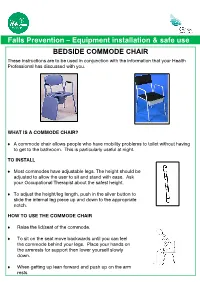
Bedside Commode Chair
Falls Prevention – Equipment installation & safe use BEDSIDE COMMODE CHAIR These instructions are to be used in conjunction with the information that your Health Professional has discussed with you. WHAT IS A COMMODE CHAIR? A commode chair allows people who have mobility problems to toilet without having to get to the bathroom. This is particularly useful at night. TO INSTALL Most commodes have adjustable legs. The height should be adjusted to allow the user to sit and stand with ease. Ask your Occupational Therapist about the safest height. To adjust the height/leg length, push in the silver button to slide the internal leg piece up and down to the appropriate notch. HOW TO USE THE COMMODE CHAIR Raise the lid/seat of the commode. To sit on the seat move backwards until you can feel the commode behind your legs. Place your hands on the armrests for support then lower yourself slowly down. When getting up lean forward and push up on the arm rests PRECAUTIONS & SAFETY Ensure that the commode chair is stable on the floor and cannot slide or tip over Ensure legs of the commode chair are adjusted to the correct height Ensure the toilet paper is situated within easy reach Ensure the pan is emptied regularly Ensure there is adequate space around the commode chair to enable safe movement on, off & around the commode MAINTENANCE & CLEANING Ensure that you regularly clean the commode chair and bucket with a mild disinfectant. For a standard commode, lift the toilet seat and pick up the bucket using the handle. -

Urological Supplies Requirements
Pharmacy & Medical Supplies Urological Supplies DOCUMENTATION IN MEDICAL RECORDS REQUIRED BY CMS Documentation Requirements Key Items to Address Duration of patient’s condition Why does the patient require the item? Clinical course Do the physical examination findings support the need for the item? Prognosis Signs and symptoms that indicate the need for the item Nature and extent of functional limitations Diagnoses that are responsible for these signs and symptoms Other therapeutic interventions and results Other diagnoses that may relate to the need for the item Medical records should contain: Urinary catheters and external urinary collection devices Medical records support the beneficiary has permanent urinary incontinence or permanent urinary retention that is not expected to be medically or surgically corrected within 3 months Indwelling catheters (A4311 – A4316, A4338 – A4346) No more than one catheter per month for routine catheter maintenance Non-routine indwelling catheter changes are covered for the following indications: • Catheter is accidentally removed (e.g., pulled out by beneficiary) • Malfunction of catheter (e.g., balloon does not stay inflated, hole in catheter) • Catheter is obstructed by encrustation, mucous plug, or blood clot • History of recurrent obstruction or urinary tract infection for which it has been established that an acuteevent is s prevented by a scheduled change frequency of more than once per month Specialty indwelling catheter (A4340) or all silicone catheter (A4344, A4312, or A4315) Criteria for an -

Cruising Game Space
CRUISING GAME SPACE Game Level Design, Gay Cruising and the Queer Gothic in The Rawlings By Tommy Ting A thesis exhibition presented to OCAD University in partial fulfillment of the requirements for the degree of Master of Fine Arts in Digital Futures Toronto Media Arts Centre 32 Lisgar Street., April 12, 13, 14 Toronto, Ontario, Canada April 2019 Tommy Ting 2019 This work is licensed under the Creative Commons Attribution-Non Commercial-ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc- sa/4.0/ or send a letter to Creative Commons, 444 Castro Street, Suite 900, Mountain View, California, 94041, USA. Copyright Notice Author’s Declaration This work is licensed under the Creative Commons Attribution-NonCommercial- ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/ or send a letter to Creative Commons, 444 Castro Street, Suite 900, Mountain View, California, 94041, USA. You are free to: Share – copy and redistribute the material in any medium or format Adapt – remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms. Under the follower terms: Attribution – You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. NonCommericial – You may not use the material for commercial purposes. ShareAlike – If you remix, transform, or build upon the material, you must distribute you contributions under the same license as the original. -

Part 3: Toilet Design Considerations: Micro Level
PLANNING FOR PUBLIC TOILETS PART 3: MICRO LEVEL: TOILET DESIGN CONSIDERATIONS: Inclusive Design for Different Types of User Groups ' To a good doctor there is no physical or mental aspect of his patient which should embarrass him. He may be worried or shocked by what his diagnosis reveals, but if he's any good, he is not embarrassed. Correspondingly, therefore, there should be no type of building, and no human function related to it which should embarrass the architect!' (Architects Journal, 1953, No.117). This section looks at the 'micro' level of detailed toilet design. However, the emphasis is upon principles, and upon 'seeing' how the different components of the toilet cubicle 'work' together, because, as they say, 'the devil is in the detail'. The emphasis is again upon the user, the range of user types, and the social and qualitative factors involved, rather than upon the technical plumbing and engineering aspects dealt with elsewhere in this course programme. There is also a longer optional explanation of the issues in the second part of the paper. A PowerPoint accompanies and illustrates Part 3. Part 3 is longer because detailed issues are so important. A fuller bibliography, list of references is given at the end. In fact Part 3 may be used as a module in its own right on inclusive design. People are Important There are many detailed design guides on the precise dimensions and locations of rails, toilet pans, washbasins, mirrors etc and so it is not the purpose of this chapter to give precise guidance on these. 'The problem' is that some toilet manuals deal with each component without seeing how they inter-relate with each other spatially.