Clinical Validation of the Comprehensive Complication Index in Colon Cancer Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2017 Procedure-Specific Measure Updates and Specifications Report Hospital-Level Risk-Standardized Complication Measure
2017 Procedure-Specific Measure Updates and Specifications Report Hospital-Level Risk-Standardized Complication Measure Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) – Version 6.0 Submitted By: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE) Prepared For: Centers for Medicare & Medicaid Services (CMS) March 2017 Table of Contents LIST OF TABLES ..................................................................................................................................3 LIST OF FIGURES .................................................................................................................................4 1. HOW TO USE THIS REPORT ............................................................................................................6 2. BACKGROUND AND OVERVIEW OF MEASURE METHODOLOGY .......................................................7 2.1 Background on the Complication Measure ........................................................................ 7 2.2 Overview of Measure Methodology ................................................................................... 7 2.2.1 Cohort ...................................................................................................................... 7 2.2.2 Outcome .................................................................................................................. 9 2.2.3 Risk-Adjustment Variables.................................................................................... -

Capricious Suntime
[Physics in daily life] I L.J.F. (Jo) Hermans - Leiden University, e Netherlands - [email protected] - DOI: 10.1051/epn/2011202 Capricious suntime t what time of the day does the sun reach its is that the solar time will gradually deviate from the time highest point, or culmination point, when on our watch. We expect this‘eccentricity effect’ to show a its position is exactly in the South? e ans - sine-like behaviour with a period of a year. A wer to this question is not so trivial. For ere is a second, even more important complication. It is one thing, it depends on our location within our time due to the fact that the rotational axis of the earth is not zone. For Berlin, which is near the Eastern end of the perpendicular to the ecliptic, but is tilted by about 23.5 Central European time zone, it may happen around degrees. is is, aer all, the cause of our seasons. To noon, whereas in Paris it may be close to 1 p.m. (we understand this ‘tilt effect’ we must realise that what mat - ignore the daylight saving ters for the deviation in time time which adds an extra is the variation of the sun’s hour in the summer). horizontal motion against But even for a fixed loca - the stellar background tion, the time at which the during the year. In mid- sun reaches its culmination summer and mid-winter, point varies throughout the when the sun reaches its year in a surprising way. -

Grand Complication No. 97912 Fetches $2,251,750
PRESS RELEASE | N E W Y O R K | 1 1 JUNE 2013 FOR IMMEDIATE RELEASE CHRISTIE’S NEW YORK IMPORTANT WATCHES AUCTION TOTALS $7,927,663 The Stephen S. Palmer PATEK PHILIPPE GRAND COMPLICATION NO. 97912 FETCHES $2,251,750 WORLD AUCTION RECORD FOR A PATEK PHILIPPE GRAND COMPLICATION * THE HIGHEST TOTAL ACHIEVED FOR ANY WATCH AT CHRISTIE’S NEW YORK THE HIGHEST PRICE ACHIEVED FOR ANY WATCH THUS FAR IN 2013 CHRISTIE’S CONTINUES TO LEAD THE MARKET FOR POCKETWATCHES AND WRISTWATCHES WITH US$50.3 MILLION IN AUCTION SALES ACHIEVED ACROSS 3 SALE SITES New York – On 11 June 2013, Christie’s New York auction of Important Watches achieved a total result of US$7,927,663 (£5,073,704 / €5,945,747), selling 87% by lot and 94% by value. The star lot of the day-long auction was the history changing Stephen S. Palmer Patek Philippe Grand Complication No. 97912 which achieved an impressive $2,251,750. Manufactured in 1898, this 18k pink gold openface minute repeating perpetual calendar split-seconds chronograph clockwatch with grande and petite sonnerie, and moon phases is a spectacular addition to scholarship surrounding Patek Philippe and Grand Complications in general. Aurel Bacs, International Head of Watches, commented: “Today’s auction marked an unparalleled event at Christie’s New York flagship saleroom in Rockefeller Center. The sale of Stephen S. Palmer Patek Philippe Grand Complication, No. 97912 cements Christie’s leadership in the category of the world’s most exceptional and rare timepieces. We were thrilled to see such active participation across 30 countries, 5 continents and over 250 Christie’s LIVE™ bidders demonstrating the ever increasing demand of our exceptionally curated sales.” WORLD AUCTION RECORD FOR ROLEX REFERENCE 5036 The Rolex, Reference 5036, a fine and rare 18K pink gold triple calendar chronograph wristwatch featuring a two-toned silvered dial with two apertures for day and month in French, circa 1949 sold for $171,750 / £109,920 / €128,813, establishing a new world auction record for the reference. -

Unprecedented Collecting Opportunites at SPRING 2012 IMPORTANT WATCHES AUCTION
For Immediate Release 3 May 2012 Contact: Luyang Jiang (Hong Kong) +852 2978 9919 [email protected] Belinda Chen (Beijing) +8610 6500 6517 [email protected] CHRISTIE‟S HONG KONG PRESENTS: Unprecedented Collecting Opportunites at SPRING 2012 IMPORTANT WATCHES AUCTION Offering More than 500 timepieces valued in excess of HK$120 million/US$16 million An important private collection of 20 examples of haute horology leads the season, including the Franck Muller Aeternitas Mega 4 - the most complicated wristwatch ever manufactured with a 36 complications The largest selection of vintage Patek Philippes ever offered in Asia An extraordinary collection of the famed Harry Winston Opus Series never before seen at auction Important Watches 9.30am & 2pm, Wednesday, 30 May, 2012 Woods Room, Convention Hall, Hong Kong Convention and Exhibition Centre No. 1 Harbour Road, Wan Chai, Hong Kong Click here to view a short video of auction highlights Hong Kong –Christie‟s will present more than 500 of the world‟s finest and rarest timepieces on 30 May with its Spring auction Important Watches. Valued in excess of HK$120 million/US$16 million, the sale offers an array of highly collectible horological creations that promises to excite and inspire the most discerning collectors, including masterworks from every top manufacturer. Leading the sale is one of the largest single owner collection of contemporary watches from world‟s top makers including brands never before offered at auction, the most prominent collections of Harry Winston Opus series watches ever offered at auction, an array of vintage and modern complicated wristwatches, stunning high jewellery wristwatches, as well rare and historical pocket watches. -

Time, Clocks, Day
IN NO VA TION 10 12 or better. But over the long tern1 , its fre quency can drift by several parts in 10 11 per Time, Clocks, day. In order to keep two clocks using quartz crystal oscillators synchronized to l microsec and GPS ond . you wou ld have to reset them at least every few hours. The resonators used in atomic clocks have Richard B. Langley surpassed considerably the accuracy and sta bility of quartz resonators. University of New Brunswick ATOMIC RESONATORS An atomic clock contains an oscillator whose oscillati ons are governed by a particular erating the satellite's signals. But just what atomic process. According to the quantum pic is an atomic clock? Before we answer ture of matter. atoms and molecules exist in thi s question, let"s examine so me of the well-defined energy states. An atom that bas ic concepts associated with clocks and fa lls from a higher to a lower energy state timekeeping. emits radiation in the form of light or radio waves with a frequency that is directly pro THE QUARTZ CRYSTAL RESONATOR portional to the change in energy of the All clocks contai n an oscillator, which in atom. Conversely. an atom that jumps from turn contains a frequency-determining ele a lower energy state to a higher one absorbs ment called a resonator. A resonator is any radiat ion of exactly the same frequency. The "Innovation" is a regular column in GPS device that vibrates or osc illates with a well existence of such quantum jumps means that World featuring discussions on recent defin ed frequency when excited. -

Multi-Facetted Sundials
The Scientific Tourist: Aberdeen Multi-facetted sundials Scotland is rich in multi-facetted sundials, singularly rich in fact. One is hard pressed to find two the same. As well as being individual in appearance, each one combines an appreciation of science, mathematics, high skill in stonemasonry, art and spectacle in a single object. Besides all of that, most of them are remarkably old, dating from between 1625 and 1725 in round numbers. They are mainly found in the gardens of venerable country houses, sometimes castles, or if they have been moved then they come from old country estates. These dials have usually outlasted the original houses of the aristocracy who commissioned them. A good many are described and some illustrated in Mrs Gatty’s famous book of sundials1 and more recently in Andrew Somerville’s account of The Ancient Sundials of Scotland2. The very top of the great sundial at Glamis Castle, from an illustration by Mrs Their widespread occurrence over Scotland attests to the fact that Gatty they were fashionable for about a century but, curiously enough, we don’t know why that was so. Were they just ‘fun’ to have in the garden, effectively a pillar with multiple clock faces on it, sometimes more than 50? Each dial is quite small so they aren’t precision instruments but people didn’t worry overmuch about the exact time of day in 1700. Were they a symbolic representation of ‘Science’ in the garden, a centre-piece and statement in a formal garden, just as later in the 18th century one may have found an orrery in the library -

{TEXTBOOK} Grand Complication : the Race to Build the Worlds Most Legendary Watch Ebook, Epub
GRAND COMPLICATION : THE RACE TO BUILD THE WORLDS MOST LEGENDARY WATCH PDF, EPUB, EBOOK Stacy Perman | 360 pages | 18 Aug 2018 | Washington Square Press | 9781439190098 | English | none Grand Complication : The Race to Build the Worlds Most Legendary Watch PDF Book Why I finished it: The team that put this book together obviously have children of their own. The Basel Fair. There is no limit to what you can learn if you are dedicated and always strive to do a little bit better each time. Hardcover , pages. Link to this review by snow tagged thriller. Any competition from Zenith was further mitigated by the fact that Zenith was a relatively small-scale producer of chronographs at this time, and did not pose a competitive threat in many of the most important markets for example, Zenith was unable to sell watches in the United States because the Zenith Electronics company had prior use of the name. She was excited to find out about the High Line , an elevated railroad trestle that has been turned into a green pedestrian walkway. Heuer and Breitling were direct competitors in the market for sports chronographs, but created a partnership to develop the Chronomatic automatic chronographs. They added complications, the name given to elements like alarms, celestial charts, and calendars. Just a moment while we sign you in to your Goodreads account. Use of special metals and alloys were used to produce the same colors, along with extreme efforts to maintain the dimensions and functionality. A picture book full of haiku that shows love throughout the four seasons. -

The Art of Horological Complications
the art of horological complications 2020/2021 THE ART OF Horological Complications © Gerhard D. Wempe KG, Hamburg 2020 Author: Thomas Wanka 2020/2021 Noble radiance BREITLING 81 Metal bracelets make wristwatches into sporty luxury items 8 Chronomat Limited Wempe Edition 82 ROLEX 19 HUBLOT 85 Oyster Perpetual GMT-Master II 20 Big Bang Integral Titanium 86 Oyster Perpetual Day-Date 40 22 CHOPARD 89 PATEK PHILIPPE 25 Alpine Eagle Chronograph 90 Nautilus Chronograph 5980/1R 26 Nautilus 5711/1R 28 GIRARD-PERREGAUX 93 Laureato Ininity - exclusively available at Wempe 94 BREGUET 31 Marine Tourbillon Équation Marchante 32 ROGER DUBUIS 97 Classique 7337 34 Excalibur Spider Huracán 98 A. LANGE & SÖHNE 37 FERDINAND BERTHOUD 101 Odysseus 38 Chronomètre FB 1 102 Zeitwerk Minute Repeater 40 ULYSSE NARDIN 105 JAEGER-LECOULTRE 43 Executive Blast Black 106 Master Control Chronograph Calendar 44 TUDOR 109 Master Grande Tradition Grande Complication 46 Black Bay Fifty-Eight Navy Blue 110 CARTIER 49 TAG HEUER 113 Pasha de Cartier 50 Carrera Heuer 02 114 VACHERON CONSTANTIN 53 WEMPE IRON WALKER GLASHÜTTE I/SA 117 Overseas Perpetual Calendar Ultra-Thin 54 Iron Walker Automatic Chronograph 118 IWC SCHAFFHAUSEN 57 Iron Walker Automatic Diver‘s Watch 120 Portugieser Perpetual Calendar 58 LONGINES 123 GLASHÜTTE ORIGINAL 61 Spirit Pilot‘s Chronograph 124 Senator Cosmopolite 62 MONTBLANC 127 WEMPE CHRONOMETERWERKE GLASHÜTTE I/SA 65 Heritage Manufacture Pulsograph Limited Edition 128 Chronometerwerke Automatic Pilot‘s Watch Bronze 66 NOMOS GLASHÜTTE 131 175 Years -

Date and Time Terms and Definitions
Date and Time Terms and Definitions Date and Time Terms and Definitions Brooks Harris Version 35 2016-05-17 Introduction Many documents describing terms and definitions, sometimes referred to as “vocabulary” or “dictionary”, address the topics of timekeeping. This document collects terms from many sources to help unify terminology and to provide a single reference document that can be cited by documents related to date and time. The basic timekeeping definitions are drawn from ISO 8601, its underlying IEC specifications, the BIPM Brochure (The International System of Units (SI)) and BIPM International vocabulary of metrology (VIM). Especially important are the rules and formulas regarding TAI, UTC, and “civil”, or “local”, time. The international standards that describe these fundamental time scales, the rules and procedures of their maintenance, and methods of application are scattered amongst many documents from several standards bodies using various lexicon. This dispersion makes it difficult to arrive at a clear understanding of the underlying principles and application to interoperable implementations. This document collects and consolidates definitions and descriptions from BIPM, IERS, and ITU-R to clarify implementation. There remain unresolved issues in the art and science of timekeeping, especially regarding “time zones” and the politically driven topic of “local time”. This document does not attempt to resolve those dilemmas but describes the terminology and the current state of the art (at the time of publication) to help guide -
Complication
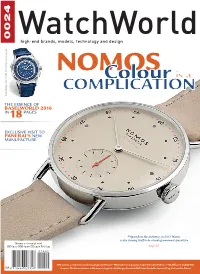
0024 WatchWorld high-end brands, models, technology and design NOMColourOS is a NTERVIEW I COMPLICATION Patek Philippe Ref. 5930G World Time Chronograph Patek Philippe Ref. 5930G World THE ESSENCE OF BASELWORLD 2016 IN 18 PAGES EXCLUSIVE VISIT TO Panerai’s NEW MANUFACTURE Apart from the aesthetics, in 2016 Nomos is also showing itself to be a leading movement specialist Volume 11 – issue 38, 2016 SEK 69,00 NOK 69,00 DK 59,00 Fi € 6,95 - page 52 - IWC unveils a new in-house chronograph movement • What’s the most popular Jaeger-LeCoultre Reverso? • Montblanc’s mighty wat- chmen • The Heuer Autavia is the new vintage hit • Frédérique Constant CEO Peter Stas talks about selling his brand to Citizen COVER STORY By Lex Stolk The new in-house DUW 3001 calibre from Nomos Glashütte is a sexy slim movement he taxi ride from Tegel, the antiqua- The best from Berlin and Glashütte ted airport of Berlin that is still in use only because the new Branden- burg airport still isn't operational Tfive years after its scheduled completion date, NOMOS' split to the neighbourhood of Kreuzberg, generates a nostalgic music moment in my mind. In the 1983 song ‘Over de Muur’ [Over the Wall] (the Cold War was still in full swing and the Wall would not be torn down for another six years) PERSONALITY the Klein Orkest wasn't just singing about the lack of freedom in East Berlin but also about the situation in the free Western district. “But what does that freedom mean, without a home, without a job? Berlin stands for trends, Glashütte stands for technology. -

Product Manual CH-4434 Hölstein Phone +41 61 956 11 11 Fax +41 61 951 20 65 [email protected] Contents
Oris SA Ribigasse 1 Product Manual CH-4434 Hölstein Phone +41 61 956 11 11 Fax +41 61 951 20 65 [email protected] www.oris.ch Contents. 7 English Introduction . 9 Adjusting Oris watches to fit the wrist . 20 Watches with leather straps . 20 Starting Oris watches . 10 Watches with rubber straps . 20 Crown positions . 10 Watches with metal bracelets . 20 Standard crown . 10 Fine adjustment of folding clasps . 20 Screw-down crown . 10 Crown with Oris Quick Lock system (QLC) . 10 Notes . 22 Screw-down pushers . 10 Accuracy . 22 Automatic winding watches . 11 Chronometer . 22 Manual winding watches . 11 Water-resistance . 24 Use and maintenance . 24 Setting and operating Oris watches . 12 Date, day of the week and time . 12 Technical information and Setting the date . 12 summary tables . 26 Worldtimer . 12 Pictograms . 26 Worldtimer with 3rd time zone and compass . 13 Metals for cases and straps . 27 2nd time zone on outer rotating bezel . 14 PVD coatings . 27 2nd time zone indicator on inner rotating Sapphire crystal . 27 bezel with vertical crown . 14 Mineral glass . 28 2nd time zone with additional 24 hr hand . 14 Plexi glass . 28 2nd time zone with additional 24 hr hand and Luminescent dials and hands . 28 city markers on the rotating bezel . 14 Metal bracelets, leather and rubber straps . 28 Chronograph . 15 Lunar calendar . 29 Complication . 15 Time zones . 30 Regulator . 16 Movements . 30 Pointer calendar . 16 Alarm with automatic winding . 16 International guarantee for Oris watches . 32 Tachymeter scale – measuring speeds . 17 Telemeter scale – measuring distances . 17 Proof of ownership . -

THE COLLOQUIUM on REQUIREMENTS for UTC and CIVIL TIMEKEEPING on EARTH (Preprint) AAS 13-501
(Preprint) AAS 13-501 THE COLLOQUIUM ON REQUIREMENTS FOR UTC AND CIVIL TIMEKEEPING ON EARTH John H. Seago, * Robert L. Seaman, † P. Kenneth Seidelmann and Steven L. Allen § On May 29 and May 30, 2013, the Colloquium on Requirements for UTC and Civil Timekeeping on Earth was hosted in Charlottesville, Virginia by the Uni- versity of Virginia (UVa), the UVa Astronomy Department, and the Jefferson Scholars Foundation. This paper highlights various technical perspectives sup- porting requirements and various recommendations discussed by colloquium participants. INTRODUCTION In response to some colloquium participants and other professionals, and in keeping with ear- lier proceedings,1 the authors have provided an extended summary of the proceedings of the col- loquium on Requirements for UTC and Civil Timekeeping on Earth. This summary highlights some of the perspectives (which are not necessarily the perspectives of the authors) discussed during the meeting in relation to requirements surrounding the topic of redefining the civil time- scale Coordinated Universal Time. However, this summary is no substitute for the wealth of de- tailed information to be discovered by careful review of the succeeding manuscripts and discus- sions; rather, it is hoped that the highlighting of specific points here encourages the reader to ex- plore the remainder of the proceedings thoroughly. The reader should appreciate that words like “need”, “must”, “shall”, “necessary”, “obligation”, “fundamental”, and of course, “required” throughout these proceedings