ICD-9 Diagnosis Codes Effective 10/1/2006 (V24.0) Source: Centers for Medicare and Medicaid Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N
case report Oman Medical Journal [2017], Vol. 32, No. 6: Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N. Onyiriuka 1* and Theodora E. Utomi2 1Endocrine and Metabolic Unit, Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria 2Special Care Baby Unit, Department of Nursing Services, St Philomena Catholic Hospital, Benin City, Nigeria ARTICLE INFO ABSTRACT Article history: Subcutaneous fat necrosis of the newborn (SCFNN) is a rare benign inflammatory Received: 4 November 2015 disorder of the adipose tissue but may be complicated by hypercalcemia or less frequently, Accepted: 21 October 2016 hypocalcemia, resulting in morbidity and mortality. Here we report the case of a neonate Online: with subcutaneous fat necrosis who surprisingly developed hypocalcemia instead DOI 10.5001/omj.2017.99 of hypercalcemia. A full-term female neonate was delivered by emergency cesarean section for fetal distress and was subsequently admitted to the Special Care Baby Keywords: Hypocalcemia; Infant, Unit. The mother’s pregnancy was uncomplicated up to delivery. Her anthropometric Newborn; Subcutaneous Fat measurements were birth weight 4.1 kg (95th percentile), length 50 cm (50th percentile), Necrosis; Perinatal Stress. and head circumference 34.5 cm (50th percentile). The Apgar scores were 2, 3, and 8 at 1, 5, 10 minutes, respectively. There was no abnormal facies and she was fed with breast milk only. On the seventh day of life, the infant was found to have multiple nodules located in the neck, upper back, and right arm. The nodules were firm, well circumscribed with no evidence of tenderness. -

Malignant Hyperthermia
:: Malignant hyperthermia Synonyms: malignant hyperpyrexia, hyperthermia of anesthesia Syndromes with higher risk of MH: ` King-Denborough syndrome ` central core disease (CCD, central core myopathy) ` multiminicore disease (with or without RYR1 mutation) ` nemaline rod myopathy (with or without RYR1 mutation) ` hypokalemic periodic paralysis Definition: Malignant hyperthermia (MH) is a rare disorder of skeletal muscles related to a high release of calcium from the sarcoplasmic reticulum which leads to muscle rigidity in many cases and hypermetabolism. Abrupt onset is triggered either by anesthesic agents such as halogenated volatile anesthetics and depolarizing muscle relaxant such as succinylcholine (MH of anesthesia), or, occasionally, by stresses such as vigorous exercise or heat. In most cases, mutations of RYR1 and CACNA1S genes have been reported. MH is characterized by tachycardia, arrhythmia, muscle rigidity, hyperthermia, skin mottling, rhabdomyolysis (cola- colored urine) metabolic acidosis, electrolyte disturbances especially hyperkalemia and coagulopathy. Dantrolene is currently the only known treatment for a MH crisis. Further information: See the Orphanet abstract Menu Pre-hospital emergency care Recommendations for hospital recommendations emergency departments Synonyms Emergency issues Aetiology Emergency recommendations Special risks in emergency situations Management approach Frequently used long term treatments Drug interactions Complications Anesthesia Specific medical care prior to hospitalisation Preventive measures -
The Vaccine Adverse Event Reporting System (VAERS)
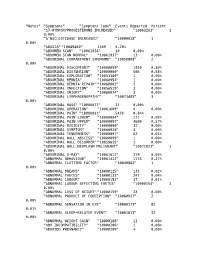
"Notes" "Symptoms" "Symptoms Code" Events Reported Percent "17-HYDROXYPROGESTERONE INCREASED" "10063263" 1 0.00% "5'NUCLEOTIDASE INCREASED" "10000028" 1 0.00% "ABASIA" "10049460" 1309 0.20% "ABDOMEN SCAN" "10061936" 10 0.00% "ABDOMEN SCAN NORMAL" "10061937" 13 0.00% "ABDOMINAL COMPARTMENT SYNDROME" "10058808" 2 0.00% "ABDOMINAL DISCOMFORT" "10000059" 1930 0.30% "ABDOMINAL DISTENSION" "10000060" 505 0.08% "ABDOMINAL EXPLORATION" "10053309" 1 0.00% "ABDOMINAL HERNIA" "10060954" 1 0.00% "ABDOMINAL HERNIA REPAIR" "10060802" 2 0.00% "ABDOMINAL INFECTION" "10056519" 3 0.00% "ABDOMINAL INJURY" "10060924" 3 0.00% "ABDOMINAL LYMPHADENOPATHY" "10073485" 3 0.00% "ABDOMINAL MASS" "10000077" 21 0.00% "ABDOMINAL OPERATION" "10061609" 6 0.00% "ABDOMINAL PAIN" "10000081" 5426 0.84% "ABDOMINAL PAIN LOWER" "10000084" 171 0.03% "ABDOMINAL PAIN UPPER" "10000087" 3699 0.57% "ABDOMINAL RIGIDITY" "10000090" 32 0.00% "ABDOMINAL SYMPTOM" "10060926" 3 0.00% "ABDOMINAL TENDERNESS" "10000097" 62 0.01% "ABDOMINAL WALL ABSCESS" "10000099" 1 0.00% "ABDOMINAL WALL DISORDER" "10059625" 1 0.00% "ABDOMINAL WALL NEOPLASM MALIGNANT" "10071023" 1 0.00% "ABDOMINAL X-RAY" "10061612" 279 0.04% "ABNORMAL BEHAVIOUR" "10061422" 1775 0.27% "ABNORMAL CLOTTING FACTOR" "10049862" 1 0.00% "ABNORMAL DREAMS" "10000125" 133 0.02% "ABNORMAL FAECES" "10000133" 247 0.04% "ABNORMAL LABOUR" "10000153" 37 0.01% "ABNORMAL LABOUR AFFECTING FOETUS" "10000154" 1 0.00% "ABNORMAL LOSS OF WEIGHT" "10000159" 23 0.00% "ABNORMAL PRODUCT OF CONCEPTION" "10060927" 2 0.00% "ABNORMAL SENSATION IN EYE" "10000173" -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

CACNA1S Gene Calcium Voltage-Gated Channel Subunit Alpha1 S
CACNA1S gene calcium voltage-gated channel subunit alpha1 S Normal Function The CACNA1S gene provides instructions for making the main piece (subunit) of a structure called a calcium channel. Channels containing the CACNA1S protein are found in muscles used for movement (skeletal muscles). These skeletal muscle calcium channels play a key role in a process called excitation-contraction coupling, by which electrical signals (excitation) trigger muscle tensing (contraction). Calcium channels made with the CACNA1S subunit are located in the outer membrane of muscle cells, so they can transmit electrical signals from the cell surface to inside the cell. The channels interact with another type of calcium channel called ryanodine receptor 1 (RYR1) channels (produced from the RYR1 gene). RYR1 channels are located in the membrane of a structure inside the cell that stores calcium ions. Signals transmitted by CACNA1S-containing channels turn on (activate) RYR1 channels, which then release calcium ions inside the cells. The resulting increase in calcium ion concentration within muscle cells stimulates muscles to contract, allowing the body to move. Health Conditions Related to Genetic Changes Malignant hyperthermia CACNA1S gene mutations account for a very small percentage of all cases of malignant hyperthermia. Malignant hyperthermia is a severe reaction to particular anesthetic drugs that are often used during surgery and other invasive procedures. The reaction involves a high fever (hyperthermia), a rapid heart rate, muscle rigidity, breakdown of muscle fibers (rhabdomyolysis), and increased acid levels in the blood and other tissues ( acidosis). Complications can be life-threatening without prompt treatment. Researchers have identified several mutations in the CACNA1S gene that are associated with an increased risk of this condition. -

Disseminated Eosinophilic Infiltration of a Newborn Infant, with Perforation of the Terminal Ileum and Bile Duct Obstruction
Arch Dis Child: first published as 10.1136/adc.56.1.66 on 1 January 1981. Downloaded from 66 Shinozaki, Saito, and Shiraki infant who acquired hepatitis from her mother. Br Med J 6 Yoshida A, Tozawa M, Furukawa N, Oya N, Kusunoki T, 1970; iv: 719-21. Kiyosawa N. HBsAg-positive chronic active hepatitis in 3 Bancroft W H, Warkel R L, Talbert A A, Russell P K. a 1 and 1/2 year-old-child (in Japanese). Shonika Shinryo Family with hepatitis-associated antigen. JAMA 1971; 1977;40: 1246-50. 217:1817-20. McCarthy J W. Hepatitis B antigen (HBAg)-positive chronic aggressive hepatitis and cirrhosis in an 8-month- Correspondence to Dr T Shinozaki, Department of old infant. A case report. JPediatr 1973; 83: 638-9. Paediatrics, Teikyo University School of Medicine, 11-1 5 Fujiwara T, Abe M, Tachi N, Jo M, Shiroda M. Kaga, 2 Chome, Itabashi-ku, Tokyo 173, Japan. HBsAg-positive infantile hepatitis associated with chronic aggressive hepatitis (in Japanese). Shonika Rinsho 1975; 28:1303-6. Received 26 November 1979 Disseminated eosinophilic infiltration of a newborn infant, with perforation of the terminal ileum and bile duct obstruction S M MURRAY AND C J WOODS Department ofPathology and Department ofPaediatrics, Victoria Hospital, Blackpool Case report SUMMARY A preterm boy died 4 days after delivery from septicaemia which at necropsy was found to be A white boy, weighing 1490 g, was born by spon- due to perforation of an eosinophilic lesion of the taneous vertex delivery at 35 weeks' gestation to a copyright. terminal ileum. -
Complex Management of a Patient with Refractory Primary Erythromelalgia Lacking a SCN9A Mutation
Complex management of a patient with refractory primary erythromelalgia lacking a SCN9A mutation Item Type Article Authors Low, Sarah; Robbins, Wendye; Tawfik, Vivianne Citation Complex management of a patient with refractory primary erythromelalgia lacking a SCN9A mutation 2017, Volume 10:973 Journal of Pain Research DOI 10.2147/JPR.S129661 Publisher DOVE MEDICAL PRESS LTD Journal Journal of Pain Research Rights © 2017 Low et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms. php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). Download date 29/09/2021 00:14:39 Item License https://creativecommons.org/licenses/by-nc/3.0/ Version Final published version Link to Item http://hdl.handle.net/10150/624081 Journal name: Journal of Pain Research Article Designation: Case Report Year: 2017 Volume: 10 Journal of Pain Research Dovepress Running head verso: Low et al Running head recto: Management of refractory erythromelalgia open access to scientific and medical research DOI: http://dx.doi.org/10.2147/JPR.S129661 Open Access Full Text Article CASE REPORT Complex management of a patient with refractory primary erythromelalgia lacking a SCN9A mutation Sarah A Low1 Abstract: A 41-year-old woman presented with burning and erythema in her extremities Wendye Robbins2,3 triggered by warmth and activity, which was relieved by applying ice. Extensive workup was Vivianne L Tawfik2 consistent with adult-onset primary erythromelalgia (EM). Several pharmacological treatments were tried including local anesthetics, capsaicin, ziconotide, and dantrolene, all providing 24–48 1Department of Internal Medicine, Banner University Medical Center, hours of relief followed by symptom flare. -

How to Avoid This Medical Emergency
Gregory L. Rose, MD; Thomas McLarney, MD; Raeford E. Brown, MD How to avoid this University of Kentucky College of Medicine, Lexington medical emergency [email protected] Avoiding an episode of malignant hyperthermia requires The authors reported no potential confl ict of interest relevant to this article. that you look for certain clues in a patient’s history. ou are asked to perform a preoperative evaluation of a PRACTICE 6-year-old boy who is due to have a tonsillectomy. Th e RECOMMENDATIONS Y family history reveals that his father had an episode that › Suspect malignant hyper- sounds like malignant hyperthermia (MH). Also, a paternal thermia (MH) if a patient uncle experienced a high fever and almost died after undergo- has night sweats, cramping, ing anesthesia. Th e boy’s parents tell you they took the boy to mottled skin, low-grade fever, a pediatrician, who did a “blood test” for MH. Th ey hand you and excessive sweating, or has a written report of an enzyme-linked immunosorbent assay, elevated creatine kinase and rhabdomyolysis on lab which tested negative for an allergy to succinylcholine. studies. B Has this child been adequately screened for MH? If you answered No, you are correct. Th e review that fol- › Make sure patients and lows explains why. their family members know that MH is life threatening, familial, and can even occur in patients whose previous The “disease of anesthesia” experiences with anesthesia MH is a pharmacogenetic disease process that occurs when have been uneventful. A predisposed individuals are exposed to certain triggering agents—specifi cally, anesthetics. -
Orphananesthesia
orphananesthesia Anaesthesia recommendations for patients suffering from Dermatomyositis Disease name: Dermatomyositis ICD 10: M33.90 Synonyms: Adult dermatomyositis, polymyositis, idiopathic inflammatory myopathy, juvenile dermatomyositis (onset < 18 yrs) Disease summary: Dermatomyositis is a chronic degenerative disease of the muscle fibres and connective tissue caused by CD4+ and T cell mediated microvasculopathy, perifascicular atrophy and muscle microinfarcts. It is a part of the idiopathic inflammatory myositis trio which includes polymyositis, dermatomyositis and inclusion body myositis. The main pathology is considered to be the perimysial ischemia leading to atrophy and degeneration. The ischemia is a result of classical complement pathway triggered by C1-q attaching to the injured endothelium leading to membrane attack complex formation and deposition in the endothelium of the capillaries. The capillary occlusion ensued by this deposition and the subsequent reperfusion is the main cause for tissue damage. The trigger for inflammation is considered to be a combined interplay of genetic, immunologic predisposition and viral infection. When the onset is less than 18 years of age, it is termed juvenile dermatomyositis. Incidence is more frequent in females than males with peak onset between 30-60 yrs. 30% adults are left with mild to severe disability. Medicine in progress Perhaps new knowledge Every patient is unique Perhaps the diagnostic is wrong Find more information on the disease, its centres of reference and patient organisations on Orphanet: www.orpha.net 1 The disease mainly involves skin and muscles but other organs are variably involved. Proximal muscle weakness is very prominent. Skin involvement involves rash. The cutaneous manifestations are a result of the vasculopathy or photosensitivity; manifestations include various eruptions, such as heliotrope rash and Gottron's papules etc. -

A STUDY of RICKETS; Incidence in London
Arch Dis Child: first published as 10.1136/adc.61.10.939 on 1 October 1986. Downloaded from Archives of Disease in Childhood, 1986, 61, 939-940 A STUDY OF RICKETS; Incidence in London. BY DONALD PATERSON, M.B. (Edin.), M.R.C.P. (London), AND RUTH DARBY, M.B., Ch.B. (Birm.). (From the Infants' Hospital, Westminster.) In order to ascertain the incidence of rickets in London a study was attempted during the months of February, MIarch and April of 1925. It was thought that these being the darkest months of the year, following on a long, sunless period, the incidence of rickets would be at its height. Our fir-st difficulty was to define the basis upon which rickets could be diagnosed. We had over and over again diagnosed rickets clinically . Commentary copyright. J 0 FORFAR The Archives of Disease in Childhood, although it radiologically and 110 (32%) showed evidence of became the official journal of the British Paediatric previous rickets clinically, although radiologically Association (BPA), was first published two years the rickets was shown to have healed. No evidence before the founding of the BPA. Appropriately, the of rickets either clinically or radiologically was senior author of this paper on rickets, Dr Donald found in 225 (67%). Interestingly from a social point Paterson, played a leading part in the founding of of view, another paper in the same issue of the the BPA and was its first Secretary. He was a Archives (by Drs W P T Atkinson, Helen Mackay, http://adc.bmj.com/ Canadian who came to Edinburgh University to W L Kinnear, and H L Shaw) showed that children study medicine. -
Sclerema Neonatorum Treated with Intravenous Immunoglobulin: a Case Report and Review of Treatments
Sclerema Neonatorum Treated With Intravenous Immunoglobulin: A Case Report and Review of Treatments Kesha J. Buster, MD; Holly N. Burford, MD; Faith A. Stewart, MD; Klaus Sellheyer, MD; Lauren C. Hughey, MD Practice Points Sclerema neonatorum is a rare neonatal panniculitis with a high mortality rate. Exchange transfusion improves survival, but its use in neonates has declined. Intravenous immunoglobulin represents a novel treatment option that may lead to increased survival in pre- term newborns with sclerema neonatorum. Sclerema neonatorum (SN)CUTIS is a rare neonatal improvement. Sclerema neonatorum remains a panniculitis that typically develops in severely poorly understood and difficult to treat neona- ill, preterm newborns within the first week of tal disorder. Although IVIG did not prevent our life and often is fatal. It usually occurs in pre- patient’s death, further studies are needed to term newborns with delivery complications such determine its clinical utility in the treatment of this as respiratory distress or maternal complica- rare disorder. tions such as eclampsia. Few clinical trials have Cutis. 2013;92:83-87. beenDo performed to address Notpotential treatments. Copy Successful treatment has been achieved via exchange transfusion (ET), but its use in neonates clerema neonatorum (SN) is a rare neonatal is declining. Similar to ET, intravenous immuno- panniculitis that typically develops in severely globulin (IVIG) enhances both humoral and Sill, preterm newborns within the first week cellular immunity and thus may decrease mor- of life. It is characterized by rapidly progressive tality associated with SN. We report a case of induration of subcutaneous fat. Treatments include SN in a term newborn who subsequently devel- supportive care, emollients, warming/maintaining oped septicemia.