Thesis Template
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Program PDF Saturday, March 28, 2020 Updated: 02-14-20
Program PDF Saturday, March 28, 2020 Updated: 02-14-20 Special ‐ Events and Meetings Congenital Heart Disease ‐ Scientific Session #5002 Session #602 Fellowship Administrators in Cardiovascular Education and ACHD Cases That Stumped Me Training Meeting, Day 2 Saturday, March 28, 2020, 8:00 a.m. ‐ 9:30 a.m. Saturday, March 28, 2020, 7:30 a.m. ‐ 5:30 p.m. Room S105b Marriott Marquis Chicago, Great Lakes Ballroom A CME Hours: 1.5 / CNE Hours: CME Hours: / CNE Hours: Co‐Chair: C. Huie Lin 7:30 a.m. Co‐Chair: Karen K. Stout Fellowship Administrators in Cardiovascular Education and Training Meeting, Day 2 8:00 a.m. LTGA, Severe AV Valve Regurgitation, Moderately Reduced EF, And Atrial Acute and Stable Ischemic Heart Disease ‐ Scientific Arrhythmia Session #601 Elizabeth Grier Treating Patients With STEMI: What They Didn't Teach You in Dallas, TX Fellowship! Saturday, March 28, 2020, 8:00 a.m. ‐ 9:30 a.m. 8:05 a.m. Room S505a ARS Questions (Pre‐Panel Discussion) CME Hours: 1.5 / CNE Hours: Elizabeth Grier Dallas, TX Co‐Chair: Frederick G. Kushner Co‐Chair: Alexandra J. Lansky 8:07 a.m. Panelist: Alvaro Avezum Panel Discussion: LTGA With AVVR And Reduced EF Panelist: William W. O'Neill Panelist: Jennifer Tremmel Panelist: Jonathan Nathan Menachem Panelist: Joseph A. Dearani 8:00 a.m. Panelist: Michelle Gurvitz Case of a Young Women With STEMI Panelist: David Bradley Jasjit Bhinder Valhalla, NY 8:27 a.m. ARS Questions (Post‐Panel Discussion) 8:05 a.m. Elizabeth Grier Young Women With STEMI: Something Doesn't Make Sense... -

SINO-VATICAN FAITH DIPLOMACY: Mapping the Factors a Ecting Bilateral Relations
Perspectives SINO-VATICAN FAITH DIPLOMACY: Mapping The Factors Aecting Bilateral Relations By Juyan Zhang CPD PERSPECTIVES ON PUBLIC DIPLOMACY Paper 2, 2017 Sino-Vatican Faith Diplomacy: Mapping the Factors Affecting Bilateral Relations Juyan Zhang April 2017 Figueroa Press Los Angeles SINO-VATICAN FAITH DIPLOMACY: MAPPING THE FACTORS AFFECTING BILATERAL RELATIONS by Juyan Zhang Published by FIGUEROA PRESS 840 Childs Way, 3rd Floor Los Angeles, CA 90089 Phone: (213) 743-4800 Fax: (213) 743-4804 www.figueroapress.com Figueroa Press is a division of the USC Bookstores Cover, text, and layout design by Produced by Crestec, Los Angeles, Inc. Printed in the United States of America Notice of Rights Copyright © 2017. All rights reserved. Except for the quotation of short passages for the purposes of criticism and review, no part of this book may be reproduced in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system now known or to be invented, without prior written permission from the author, care of Figueroa Press. Notice of Liability The information in this book is distributed on an “As is” basis, without warranty. While every precaution has been taken in the preparation of this book, neither the author nor Figueroa nor the USC University Bookstore shall have any liability to any person or entity with respect to any loss or damage caused or alleged to be caused directly or indirectly by any text contained in this book. Figueroa Press and the USC Bookstores are trademarks of the University of Southern California. ISBN-13: 978-0-18-221704-5 ISBN-10: 0-18-221704-3 About the USC Center on Public Diplomacy The USC Center on Public Diplomacy (CPD) was established in 2003 as a partnership between the Annenberg School for Communication & Journalism and the School of International Relations at the University of Southern California. -

19 09 Sep Wag.Pub
West Wagga Parish Serving: Ashmont, Collingullie, Glenfield, Lloyd, and San Isidore The West Wagga Wag September 2019 Coming Events New Baptism Font at Adoration of the Blessed Sacrament, Holy Trinity Holy Trinity! - 6 to 7am daily; - overnight from 9pm Friday After a great fund raising effort, our new Baptism font through to 7am Saturdays was installed on the 16th of August by Paul Hallett, whose family have been stone masons working in Monthly Cuppa, after 9am Mass on last Sunday of the month. churches for 5 generations. St Pope Gregory the Great Tue 3 The bowl in our new font is St John Chrysostom Fri 13 from our original font, so the The Exaltation of the bowl that caught the baptism Holy Cross Sat 14 water poured over the heads of St Robert Bellarmine Tue 17 those baptised decades ago will Sts Andrew Kim Taegon, be the bowl that catches the and Companions Fri 20 holy water for years to come. St Matthew, Apostle Sat 21 St Pius of Pietrelcina Mon 23 St Vincent de Paul Fri 27 Our first baptisms using the new font on Saturday August 17 - St Jerome Mon 30 Aliyah Elizabeth Rose Wray 8th Sept (left) and Mariusz Ethan Forro (below) Inside this issue: September Sillies 3 5 Farewell Tim Fischer Movie Unplanned in Wagga! 6 Pro-Life Work to do! 7 The Blessing of the Parish Baptism Font Wag Contacts will take place during 9am Mass on September 8. We invite everyone to come, Email: [email protected] especially those who have made generous donations Web Page: westwaggaparish.com Phone: 6931 3601 to provide our Font. -

The Guest Speakers Sister Teresa Huang, C.I.C. (Canton) and Sister Rosa Lee, C.I.C .Were Briefly Introduced by Serran Dominic Tang
The guest speakers Sister Teresa Huang, C.I.C. (Canton) and Sister Rosa Lee, C.I.C .were briefly introduced by Serran Dominic Tang. They spoke on the history and current work of the Chinese Sisters of the Immaculate Conception (C.I.C.): - A. Present Status in Hong Kong (Sister Rosa Lee) The Chinese Sisters of the Immaculate Conception (C.I.C.) was a women religious community started in Canton, China in 1932 for Chinese ladies working for Chinese communities. With the change of government in China in 1949, the C.I.C. sisters were persecuted vigorously. Between 1951-1954, six sisters were expelled from China. With the assistance of the Bishop of Hong Kong, the sisters founded St. Antonius Kindergarten and St. Antonius Primary School in Yau Tong in 1959. The St. Antonius girls’ College was founded in 1972, but was handed back to the Diocese of Hong Kong in 2017 due to manpower shortage. Their work is mainly in education and teaching catechism in various parishes. There are now only 11 nuns, with average age over 60. B. History in China (by Sister Teresa Huang from Guangzhou, China) Due to the political unrest during the Opium War and invasion by foreign powers, a group of 5 “consecrated virgins” was placed under the care of French Nuns (MEP) in 1895. A female community of nuns was started on 8th December 1902. This group was handed over to the Canadian nuns belonging to the Immaculate Conception. These Chinese nuns were separated from the Canadian nuns in 1920 by the Bishop of Canton. -
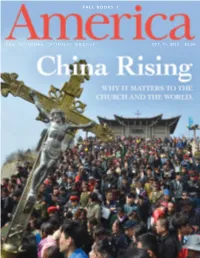
Fall Books 1
FALL BOOKS 1 THE NATIONAL CATHOLIC WEEKLY OCT. 14, 2013 $3.50 OF MANY THINGS Published by Jesuits of the United States 1958. One of the first things he saw he Society of Jesus and China 106 West 56th Street have a long and complicated at the police station was a poster New York, NY 10019-3803 history, one that goes back to indicting him: “Tang Yee-ming is Ph: 212-581-4640; Fax: 212-399-3596 T the most faithful running dog of Subscriptions: 1-800-627-9533 the very beginnings of the order. One of the co-founders of the Jesuits, the the reactionary Vatican.” Although www.americamagazine.org he was neither officially tried nor facebook.com/americamag great St. Francis Xavier, died during his twitter.com/americamag attempt to reach the Chinese mainland. sentenced, he was kept in prison for the next 22 years. Much of that time Thirty years later, in 1582, Matteo Ricci, EDITOR IN CHIEF Matt Malone, S.J. he spent in solitary confinement S.J., succeeded where Xavier had failed, EXECUTIVE EDITORS in a tiny and almost lightless cell bringing the Catholic faith as well as Robert C. Collins, S.J., Maurice Timothy Reidy furnished only with a bench for Western science, mathematics and MANAGING EDITOR Kerry Weber sleeping. astronomy to the Eastern world. Today, Since he was not permitted either LITERARY EDITOR Raymond A. Schroth, S.J. at the China Millennium Monument to write or receive letters, his relatives SENIOR EDITOR & CHIEF CORRESPONDENT in Beijing, Father Ricci is the only Kevin Clarke and friends presumed by the 1970s Westerner included in the pantheon that he was dead. -

True Catholic and Authentic Chinese: the Theologico-Political Polemic in China
InternationalTrue Catholic Journal and Authentic of China Chinese: Studies The Theologico-Political Polemic in China 257 Vol. 11, No. 2, December 2020, pp. 257-276 True Catholic and Authentic Chinese: The Theologico-Political Polemic in China Wing Kwan Anselm Lam* Department of Cultural and Religious Studies Chinese University of Hong Kong Abstract After a lengthy negotiation between the Vatican and the Chinese government over decades, both parties signed a provisional agreement on 22 September 2018. Although they did not reveal the details to the public, both sides made a compromise on the appointment of the bishop, which is the crucial part of the conflict. Among those religions in China, the Chinese government paid much more attention upon the Catholic Church. One of the reasons would be the similarity of two entities, that is the centralization of power on one person. The current policies like restricting children going to church, dismantling the cross of the church, no Christmas decoration or promotion during Christmas, which give negative impact upon the Catholic Church, while the Beijing government signed the provisional agreement on the appointment of the bishop. Pope Francis unlike his predecessor does not excommunicate those bishops ordained without the Pope’s approval but resumes their episcopal duties, while the Catholic Church in China is still under persecution. How to understand the underlying reasons of the move of the CCP and the Vatican in this agreement? This paper will investigate the nature and principles of religious policy in China and the Vatican’s stance on China affairs in the light of a theologico-political polemic. -

The B'eijing-Rome Dialogue
100 Chronicle years in camp for her activities. Though ex this has been deferred for two years but she tremely weak she nevertheless resumed her is required not to leave her place of resi work with the CPR after her release in late dence without permission from the militia. 1973. and remained active until her depar Then, between May and July, the homes of ture for the United States with her family in several Council activists were searched, in 1979. cluding those of the Khorev family in Kish During the early 1970s Lidiya~s place as inyov. the Kozorezovs in Voroshilovgrad leader of the Council was taken by Galina and the Naprienkos in Moscow. At the Rytikova. whose husband Pavel was then home ofVasili and Natasha Dimitriyev (the serving a prison term. It was during this daughter of Galina Rytikova) the CPR arc period that the Bulletin was founded; as hive was found and confiscated. Secretary. Rytikova collected the Of those affected by the searches, two ap documentation. and it was in her home that peared likely to face prosecution. Ulyana the members of the CPR compiled the Bul Germanyuk (whose husband Stepan is in letin. During 1978. Galina was forced by prison), an active member of the Council, threats of psychiatric internment to go into was arrested on 23 July while visiting her hiding with her three youngest children. daughter in the Crimea. Since then her Alexandra Kozorezova was formally children have been unable to obtain any elected President of the CPR after the emi further information about her position. -

Seminar on Religious Freedom in China
Seminar on Religious Freedom in China Date: March 2, 2003 (Sunday) Organizer: Justice and Peace Commission of the Hong Kong Catholic Diocese Topics & Speakers: An Analysis of the Current Situation of the Catholic Church in China .................. Father Gianni Criveller (Researcher at the Holy Spirit Study Centre in Hong Kong) Experience Sharing ........................... Father Franco Mella (Kwai Chung New District Christian Grassroots Group) An Analysis of the Changes in Religious Freedom in China in the Past 20 Years ......................... Anthony Lam Sui-ki (Researcher at the Holy Spirit Study Centre in Hong Kong) The Relations Between the Church in Hong Kong and the Church in China ...................................................................... Bishop Joseph Zen Ze-kiun (Bishop of Hong Kong ) Father Gianni Criveller: No Change in Religious Policy The first point that I wish to make is that the Chinese government has made no progress in its religious policy in the last 20 years. The Constitution of 1982 (Article 36) and Document No. 19 of the same year have codified Deng Xiaoping's religious policy. Since then the policy has remained the same: The Party controls religions and the Church; religions must accommodate to the goals of the Communist Party. In other words, religion is tolerated as long as it serves Party policy, which currently is the modernization of the country. Recently, the viewpoints of two Mainland scholars, Pan Yue and Li Pingye have raised hope that there might be some development in the religious policy. I am less optimistic. I do not find Pan Yue and Li Pingye's suggestions really new or positive. Pan Yue suggests that the Party should go beyond condemning religion as "the opium of people". -

Bishop Kung - a Model for All the Clergy
Bishop Kung - a Model for All the Clergy a Homily by His Excellency Most Reverend Archbishop Dominic Tang, S.J. Archbishop of Canton, China On the Occasion of the Diamond Jubilee of the Ordination to Priesthood and the 40th Anniversary as a Bishop of Bishop Ignatius Pin-Mei Kung, Bishop of Shanghai, China June 2, 1990. Stamford, Connecticut, U.S.A. (Note: Archbishop Dominic Tang, S.J. was the Archbishop of Canton, China. Archbishop Tang and Bishop Kung met in Shanghai while both were priests teaching in the Jesuit High School. About a year after Bishop Kung was appointed bishop of Soochow, Archbishop Dominic Tang was also appointed bishop of Canton on February 13, 1951. Both bishops accepted the episcopate while the Communist persecution on the Roman Catholic Church was going on. Bishop Kung was arrested on September 8, 1955. Later, Archbishop Tang was arrested on February 5, 1958. He was imprisoned for 22 years without ever being sentenced. Archbishop Tang spent some years in solitary confinement. He was released on June 9, 1980 due to the archbishop's advanced cancer. This celebration of Bishop Kung's 60th anniversary of ordination to the priesthood and 40th anniversary as bishop brought two good friends, Archbishop Tang and Bishop Kung, together in Stamford, Connecticut after 40 years of separation.) My dear Bishop Kung: My dear brothers and sisters in Christ: The Cardinal Kung Foundation - Bishop Kung - a Model for All the Clergy Page 1 Today, we gather here in this church, to thank God for giving China an outstanding shepherd and a great priest, Bishop Kung. -

News in Brief
News in Brief CHINA Tieshan, who in his answer to the parts of the Pope's speech in Manila directed Pope John Paul's Message to Chinese towards China accused the Vatican of giv Christians ing support to Chinese Catholics who do During his visit to the Philippines in not belong to the "Patriotic Association". February 1981, the Pope made his first The article states that no Chinese religious open invitation for rapprochement with the organization has the right to accept finan Catholic Church in China. (The official cial help from other religious organizations "Patriotic" Catholic Church in China does abroad. Religious organizations in China not recognize the authority of the Vatican; must be "patriotic and free". Believers meanwhile many Chinese Catholics re· have the same duty as atheists to "love main loyal to Rome (see RCL Vo!. 8, No. 4, their country and socialism and support pp. 268-73).) The Vatican believes that the aims of the Communist Party". (AKSA, there are between 500,000 and two million 20 March 1981) baptized Catholics in China, and 580 priests. "I am convinced", said the Pope, Mgr Dominic Tang "that every Catholic within your frontiers During the tour of Pope John Paul to the will fully contribute to the building up of Far East in early 1981, Cardinal Casaroli, China, since a genuine and faithful Chris the Vatican Secretary of State, paid a visit tian is also a genuine and good citizen ...". to Hong Kong to meet and convey the He said that the Church does not seek any Papal blessing to Bishop Dominic Tang, privileges in China, "but only that all those 73-year-old apostolic administrator of the who f()lIow Christ may be able to express Archbishopric of Canton. -

John Patrick Publishing Co • 800-333-3166 • Campus of Care PSYCHOTHERAPY J
St. Mary Roman Catholic Parish 55 Catoonah Street Ridgefield, CT 06877 Phone: (203) 438-6538 Fax: (203) 438-4406 Saint Mary Parish www.smcr.org CORPUS CHRISTI June 6, 2021 The Most Holy Body & Blood of Christ Corpus Christi Sunday “I Would Like to Say Mass.” Dominic Tang, the courageous Chinese archbishop, was imprisoned for twenty-one years for nothing more than his loyalty to Christ and Christ’s one, true Church. After he had spent five years of solitary confinement in a windowless, damp cell, he was told by his jailers that he could leave it for a few hours to do whatever he wanted. Five years of solitary confinement and he had a couple of hours to do what he wanted! What would it be? A hot shower? A change of clothes? Certainly, a long walk outside? A chance to call or write to family? What would it be? the jailer asked him. “I would like to say Mass,” replied Archbishop Tang. [Msgr. Timothy M. Dolan, Priests of the Third Millennium (2000), p. 216]. The Vietnamese Jesuit, Joseph Nguyen-Cong Doan, who spent nine years in labor camps in Vietnam, relates how he was finally able to say Mass when a fellow priest- prisoner shared some of his own smuggled supplies. “That night, when the other prisoners were asleep, lying on the floor of my cell, I celebrated Mass with tears of joy. My altar was my blanket, my prison clothes my vestments. But I felt myself at the heart of humanity and of the whole of creation.” (Ibid., p. -

People, Communities, and the Catholic Church in China Edited by Cindy Yik-Yi Chu Paul P
CHRISTIANITY IN MODERN CHINA People, Communities, and the Catholic Church in China Edited by Cindy Yik-yi Chu Paul P. Mariani Christianity in Modern China Series Editor Cindy Yik-yi Chu Department of History Hong Kong Baptist University Kowloon Tong, Hong Kong This series addresses Christianity in China from the time of the late Ming and early Qing dynasties to the present. It includes a number of disciplines—history, political science, theology, religious studies, gen- der studies and sociology. Not only is the series inter-disciplinary, it also encourages inter-religious dialogue. It covers the presence of the Catholic Church, the Protestant Churches and the Orthodox Church in China. While Chinese Protestant Churches have attracted much scholarly and journalistic attention, there is much unknown about the Catholic Church and the Orthodox Church in China. There is an enor- mous demand for monographs on the Chinese Catholic Church and the Orthodox Church. This series captures the breathtaking phenomenon of the rapid expansion of Chinese Christianity on the one hand, and the long awaited need to reveal the reality and the development of Chinese Catholicism and the Orthodox religion on the other. Christianity in China refects on the tremendous importance of Chinese-foreign relations. The series touches on many levels of research—the life of a single Christian in a village, a city parish, the conficts between converts in a province, the policy of the provincial authority and state-to-state relations. It concerns the infuence of dif- ferent cultures on Chinese soil—the American, the French, the Italian, the Portuguese and so on.