And Biomarker-Based Algorithm for Management of Acute Gvhd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Interleukins in Therapeutics
67 ISSN: 2347 - 7881 Review Article Interleukins in Therapeutics Anjan Khadka Department of Pharmacology, AFMC, Pune, India [email protected] ABSTRACT Interleukins are a subset of a larger group of cellular messenger molecules called cytokines, which are modulators of cellular behaviour. On the basis of their respective cytokine profiles, responses to chemokines, and interactions with other cells, these T-cell subsets can promote different types of inflammatory responses. During the development of allergic disease, effector TH2 cells produce IL-4, IL- 5, IL-9, and IL-32. IL-25, IL- 31, and IL-33 contributes to TH2 responses and inflammation. These cytokines have roles in production of allergen-specific IgE, eosinophilia, and mucus. ILs have role in therapeutics as well as diagnosis and prognosis as biomarker in various conditions. Therapeutic targeting of the IL considered to be rational treatment strategy and promising biologic therapy. Keywords: Interleukins, cytokines, Interleukin Inhibitors, Advances INTRODUCTION meaning ‘hormones’. It was Stanley Cohen in Interleukins are group of cytokines that were 1974 who for the first time introduced the term first seen to be expressed by leucocytes and ‘‘cytokine’’. It includes lymphokines, they interact between cells of the immune monokines, interleukins, and colony stimulating systems. It is termed by Dr. Vern Paetkau factors (CSFs), interferons (IFNs), tumor (University of Victoria) in1979.Interleukins (IL) necrosis factor (TNF) and chemokines. The are able to promote cell growth, differentiation, majority of interleukins are synthesized by and functional activation. The question of how helper CD4 T lymphocytes as well as through diverse cell types communicate with each monocytes, macrophages, and endothelial cells. -

Challenges and Approaches for the Development of Safer Immunomodulatory Biologics
REVIEWS Challenges and approaches for the development of safer immunomodulatory biologics Jean G. Sathish1*, Swaminathan Sethu1*, Marie-Christine Bielsky2, Lolke de Haan3, Neil S. French1, Karthik Govindappa1, James Green4, Christopher E. M. Griffiths5, Stephen Holgate6, David Jones2, Ian Kimber7, Jonathan Moggs8, Dean J. Naisbitt1, Munir Pirmohamed1, Gabriele Reichmann9, Jennifer Sims10, Meena Subramanyam11, Marque D. Todd12, Jan Willem Van Der Laan13, Richard J. Weaver14 and B. Kevin Park1 Abstract | Immunomodulatory biologics, which render their therapeutic effects by modulating or harnessing immune responses, have proven their therapeutic utility in several complex conditions including cancer and autoimmune diseases. However, unwanted adverse reactions — including serious infections, malignancy, cytokine release syndrome, anaphylaxis and hypersensitivity as well as immunogenicity — pose a challenge to the development of new (and safer) immunomodulatory biologics. In this article, we assess the safety issues associated with immunomodulatory biologics and discuss the current approaches for predicting and mitigating adverse reactions associated with their use. We also outline how these approaches can inform the development of safer immunomodulatory biologics. Immunomodulatory Biologics currently represent more than 30% of licensed The high specificity of the interactions of immu- biologics pharmaceutical products and have expanded the thera- nomodulatory biologics with their relevant immune Biotechnology-derived peutic options available -

BIOLOGIC THERAPIES ASTHMA DYKEWICZ F BW.Pdf
11/30/2011 Biologic Asthma Therapies and Individualized Medicine Disclosures Advisory boards Mark S. Dykewicz, MD Merck (advisor, honorarium) Director, Allergy & Immunology Shire (advisor, honorarium) Fellowship Program Director Wake Forest University School of Medicine Editorial boards Winston-Salem, North Carolina USA Allergy & Asthma Proceedings American Journal of Rhinology & Allergy Clinical Reviews in Allergy & Immunology Journal of Angioedema Learning Objective Biological therapies May fill unmet needs, potentially in To better understand the use of biologic subpopulations or phenotypes of patients with modifiers in individualized asthma more severe asthma. treatment. May provide insight into mechanisms of asthma Sheharyar, Durrani, Busse. Biological Therapy for Asthma. ACCP PCCSU Article | 03.15.11 Omalizumab (Anti-IgE) Biologics with action against IgE (omalizumab) Biologic mechanism: Mab against IgE; decreases IgE Cytokines levels; results in down-regulation of IgE receptor IL-4 and/or IL-13 Patient subsets: persistent asthma selected for IL-5 specific IgE to perennial allergen, total serum IgE in Chemokine Receptors specified range CCR3 Benefits: 8 trials (n=3429) Rodrigo. Chest 2011 139:28 CXCR2 decreases in exacerbations, dose of inhaled and oral Transcription Factors corticosteroids, hospitalizations PPARs (peroxisome proliferator-activated receptors) improvement in QOL when used as add-on Rx Prostaglandin Receptors no improvement in lung function. CRTH2 6 1 11/30/2011 IL-4 Modifiers IL-13 Altrakincept Solubilized IL-4 Failed to show efficacy in large phase Pleiotropic cytokine of Th2 cells, promotes IgE receptor fragment, 3 trial. production neutralizes IL-4 Adcock et al (2008) May contribute to key features of asthma Pascolizumab Monoclonal Ab Phase 2 study of pascolizumab IL-13 production inhibited by inhaled glucocorticoids against IL- 4 discontinued because of inefficacy. -

Biological Therapies for Atopic Dermatitis: an Update (Review)
EXPERIMENTAL AND THERAPEUTIC MEDICINE 17: 1061-1067, 2019 Biological therapies for atopic dermatitis: An update (Review) DIANA DELEANU1-3 and IRENA NEDELEA1,2 1Allergology and Immunology Discipline, ‘Iuliu Hatieganu’ University of Medicine and Pharmacy, 400058 Cluj-Napoca; Departments of 2Allergy and 3Internal Medicine, ‘Professor Doctor Octavian Fodor’ Regional Institute of Gastroenterology and Hepatology, 400162 Cluj-Napoca, Romania Received July 6, 2018; Accepted August 22, 2018 DOI: 10.3892/etm.2018.6989 Abstract. Severe atopic dermatitis, which affects both adults in low-income countries (3). Furthermore, the past decades and children, is a debilitating disorder with a significant decline brought a 2-3-fold increase in prevalence in industrialized of patients' quality of life. Although aetiopathogenic factors countries (3). Generally AD onset is in early childhood, as are currently a topic of study and interpretation, the main one of the first steps of the ‘atopic march’, which describes the features of atopic eczema are skin barrier disturbance and natural history of atopic manifestations, and it is character- immune dysregulation. Severe refractory disease that fails to ized by xerotic skin and acute flare-ups of intensely pruritic improve with conventional therapy may benefit from biologic eczematous lesions (4). Recent studies recognize a predilection therapy. Progress in understanding immunopathology of atopic of AD for persistence in adulthood, with a lifetime prevalence dermatitis have allowed identification of therapeutic molecular accounting for 34.1% (5). Early onset, allergic rhinitis and targets in the field of biological therapy. We reviewed the hand eczema in childhood are high-risk factors for persistent different biological treatments with a focus on novel targeted AD (5). -
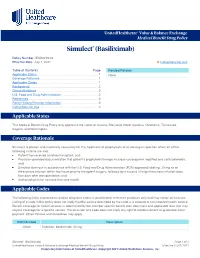
Simulect® (Basiliximab)
UnitedHealthcare® Value & Balance Exchange Medical Benefit Drug Policy Simulect® (Basiliximab) Policy Number: IEXD0219.02 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policies Applicable States ........................................................................... 1 None Coverage Rationale ....................................................................... 1 Applicable Codes .......................................................................... 1 Background.................................................................................... 2 Clinical Evidence ........................................................................... 2 U.S. Food and Drug Administration ............................................. 2 References ..................................................................................... 2 Policy History/Revision Information ............................................. 2 Instructions for Use ....................................................................... 3 Applicable States This Medical Benefit Drug Policy only applies to the states of Arizona, Maryland, North Carolina, Oklahoma, Tennessee, Virginia, and Washington. Coverage Rationale Simulect is proven and medically necessary for the treatment of prophylaxis of acute organ rejection when all of the following criteria are met: Patient has received a kidney transplant; and Physician provided documentation that patient’s prophylaxis therapy includes cyclosporine modified and corticosteroids; and Simulect -

New Treatments for Atopic Dermatitis Targeting Skin Barrier Repair Via the Regulation of FLG Expression
Journal of Clinical Medicine Review New Treatments for Atopic Dermatitis Targeting Skin Barrier Repair via the Regulation of FLG Expression Anna D˛ebi´nska 1st Department and Clinic of Paediatrics, Allergology and Cardiology, Wroclaw Medical University, Chałubi´nskiego2a, 50-368 Wrocław, Poland; [email protected]; Tel.: +48-510-066-478 or +71-770-30-91; Fax: +48-713-281-206 Abstract: Atopic dermatitis (AD) is one of the most common chronic, inflammatory skin disorders with a complex etiology and a broad spectrum of clinical phenotypes. Despite its high prevalence and effect on the quality of life, safe and effective systemic therapies approved for long-term management of AD are limited. A better understanding of the pathogenesis of atopic dermatitis in recent years has contributed to the development of new therapeutic approaches that target specific pathophysiological pathways. Skin barrier dysfunction and immunological abnormalities are critical in the pathogenesis of AD. Recently, the importance of the downregulation of epidermal differentiation complex (EDC) molecules caused by external and internal stimuli has been extensively emphasized. The purpose of this review is to discuss the innovations in the therapy of atopic dermatitis, including biologics, small molecule therapies, and other drugs by highlighting regulatory mechanisms of skin barrier-related molecules, such as filaggrin (FLG) as a crucial pathway implicated in AD pathogenesis. Keywords: atopic dermatitis; skin barrier; filaggrin; biologicals; small molecule therapies Citation: D˛ebi´nska,A. New Treatments for Atopic Dermatitis 1. Introduction Targeting Skin Barrier Repair via the Atopic dermatitis (AD) is one of the most common chronic inflammatory skin disor- Regulation of FLG Expression. -

Atopic Dermatitis (AD)
This activity is provided by PRIME Education. There is no fee to participate. This activity is supported by education grants from AbbVie, Inc., Sanofi Genzyme and Regeneron Pharmaceuticals. © 2019 PRIME® Education, LLC. All Rights Reserved.. Overview This downloadable fact‐sheet provides an easy‐to‐follow collection of the latest evidence shaping the treatment and management of psoriasis (PsO) and atopic dermatitis (AD). Learn about validated tools, evidence‐based strategies, and new and emerging targeted therapies that can be incorporated in daily practice to improve outcomes for patients with these conditions. © 2019 PRIME® Education, LLC. All Rights Reserved.. 2 1 Learning Objectives • Identify major barriers to evidence‐based treatment and management in federal and public sectors • Implement appropriate methods for diagnosis and assessment of disease activity • Assess current evidence on targeted biologic and small‐molecule therapies to guide treatment decisions for patients with moderate to severe disease • Monitor treatment responses according to treat‐to‐target principles and methods • Apply current evidence and guidelines to inform treatment decisions for patients with inadequate responses to initial therapies • Incorporate patient‐reported outcomes and shared decision‐making into clinical practice • Apply effective strategies for multidisciplinary care coordination and shared patient management © 2019 PRIME® Education, LLC. All Rights Reserved.. 3 Accreditation In support of improving patient care, PRIME® is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team. This activity was planned by and for the healthcare team, and learners will receive 2.25 Interprofessional Continuing Education (IPCE) credits for learning and change. -

Atopic Dermatitis: an Expanding Therapeutic Pipeline for a Complex Disease
REVIEWS Atopic dermatitis: an expanding therapeutic pipeline for a complex disease Thomas Bieber 1,2,3 Abstract | Atopic dermatitis (AD) is a common chronic inflammatory skin disease with a complex pathophysiology that underlies a wide spectrum of clinical phenotypes. AD remains challenging to treat owing to the limited response to available therapies. However, recent advances in understanding of disease mechanisms have led to the discovery of novel potential therapeutic targets and drug candidates. In addition to regulatory approval for the IL-4Ra inhibitor dupilumab, the anti- IL-13 inhibitor tralokinumab and the JAK1/2 inhibitor baricitinib in Europe, there are now more than 70 new compounds in development. This Review assesses the various strategies and novel agents currently being investigated for AD and highlights the potential for a precision medicine approach to enable prevention and more effective long-term control of this complex disease. Atopic disorders Atopic dermatitis (AD) is the most common chronic inhibitors tacrolimus and pimecrolimus and more 1,2 A group of disorders having in inflammatory skin disease . About 80% of disease cases recently the phosphodiesterase 4 (PDE4) inhibitor cris- common a genetic tendency to typically start in infancy or childhood, with the remain- aborole. For the more severe forms of AD, besides the develop IgE- mediated allergic der developing during adulthood. Whereas the point use of ultraviolet light, current therapeutic guidelines reactions. These are atopic dermatitis, food allergy, allergic prevalence in children varies from 2.7% to 20.1% across suggest ciclosporin A, methotrexate, azathioprine and 3,4 rhino- conjunctivitis and countries, it ranges from 2.1% to 4.9% in adults . -

Pharmacokinetic-Pharmacodynamic Modelling of Systemic IL13 Blockade by Monoclonal Antibody Therapy: a Free Assay Disguised As Total
pharmaceutics Article Pharmacokinetic-Pharmacodynamic Modelling of Systemic IL13 Blockade by Monoclonal Antibody Therapy: A Free Assay Disguised as Total John Hood 1,*, Ignacio González-García 1 , Nicholas White 1, Leeron Marshall 1,2, Vincent F. S. Dubois 1 , Paolo Vicini 1,3 and Paul G. Baverel 1,4 1 Clinical Pharmacology and Quantitative Pharmacology, AstraZeneca, Cambridge CB21 6GH, UK; [email protected] (I.G.-G.); [email protected] (N.W.); [email protected] (L.M.); [email protected] (V.F.S.D.); [email protected] (P.V.); [email protected] (P.G.B.) 2 Salford Royal Foundation Trust, Salford M6 8HD, UK 3 Confo Therapeutics, 9052 Ghent, Zwijnaarde, Belgium 4 Roche Pharma Research and Early Development, Clinical Pharmacology, Pharmaceutical Sciences, Roche Innovation Center Basel F. Hoffmann-La Roche Ltd., CH-4070 Basel, Switzerland * Correspondence: [email protected]; Tel.: +44-1223-749-6288 Abstract: A sequential pharmacokinetic (PK) and pharmacodynamic (PD) model was built with Nonlinear Mixed Effects Modelling based on data from a first-in-human trial of a novel biologic, MEDI7836. MEDI7836 is a human immunoglobulin G1 lambda (IgG1λ-YTE) monoclonal antibody, Citation: Hood, J.; González-García, with an Fc modification to reduce metabolic clearance. MEDI7836 specifically binds to, and function- I.; White, N.; Marshall, L.; Dubois, ally neutralizes interleukin-13. Thirty-two healthy male adults were enrolled into a dose-escalation V.F.S.; Vicini, P.; Baverel, P.G. clinical trial. Four active doses were tested (30, 105, 300, and 600 mg) with 6 volunteers enrolled Pharmacokinetic-Pharmacodynamic per cohort. Eight volunteers received placebo as control. -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

B Cell Immunity in Solid Organ Transplantation
REVIEW published: 10 January 2017 doi: 10.3389/fimmu.2016.00686 B Cell Immunity in Solid Organ Transplantation Gonca E. Karahan, Frans H. J. Claas and Sebastiaan Heidt* Department of Immunohaematology and Blood Transfusion, Leiden University Medical Center, Leiden, Netherlands The contribution of B cells to alloimmune responses is gradually being understood in more detail. We now know that B cells can perpetuate alloimmune responses in multiple ways: (i) differentiation into antibody-producing plasma cells; (ii) sustaining long-term humoral immune memory; (iii) serving as antigen-presenting cells; (iv) organizing the formation of tertiary lymphoid organs; and (v) secreting pro- as well as anti-inflammatory cytokines. The cross-talk between B cells and T cells in the course of immune responses forms the basis of these diverse functions. In the setting of organ transplantation, focus has gradually shifted from T cells to B cells, with an increased notion that B cells are more than mere precursors of antibody-producing plasma cells. In this review, we discuss the various roles of B cells in the generation of alloimmune responses beyond antibody production, as well as possibilities to specifically interfere with B cell activation. Keywords: HLA, donor-specific antibodies, antigen presentation, cognate T–B interactions, memory B cells, rejection Edited by: Narinder K. Mehra, INTRODUCTION All India Institute of Medical Sciences, India In the setting of organ transplantation, B cells are primarily known for their ability to differentiate Reviewed by: into long-lived plasma cells producing high affinity, class-switched alloantibodies. The detrimental Anat R. Tambur, role of pre-existing donor-reactive antibodies at time of transplantation was already described in Northwestern University, USA the 60s of the previous century in the form of hyperacute rejection (1). -

Gist Right: Five Leading Dermatologists Balance Education and Engagement in New Web Series
PRACTICAL DERMATOLOGY® NEWS << VOLUME 16, NO. 11 • NOVEMBER 2019 Gist Right: Five Leading Dermatologists Balance Education and Engagement in New Web Series Five leading dermatologists are taking on social >> media misinformation one YouTube video at a time. Doris Day, MD; Jeanine Downie, MD; Sabrina Fabi, MD; Ava Shamban, MD; and Ruth Tedaldi, MD are the faces—and the brains—of “The Gist,” a new web series aimed at giving dermatology patients the facts about aesthetic and medical conditions and treatments. “We were constantly seeing lots of social media presence that is not accurate or expert in nature. We talk about it all the time,” says Dr. Tedaldi. The physicians wanted to find a way to reach the masses with facts and science, rather than hype. The concept of a web-based discussion format program was born. “We were very motivated and very excited,” Dr. Tedaldi says. “Really what we want to do is open the field of aes- thetic medicine.” “We want to take the fright factor out of cosmetic derma- benefit of having not just one opinion; you have the five tology,” adds Dr. Downie. opinions. It’s very difficult to go see even one dermatologist, The team knew that producing the series would require but to be able to have access to five very educated derma- more resources than they could muster. They approached tologists?” Allergan, and the company agreed to support the program The panelists may not always reach consensus, but viewers to grow the market for everyone as a non-branded venue. “can find the truth somewhere in between,” Dr.